Abstract
Aim
The present study was undertaken to examine the role of IL-4 (− 590 C/T) (rs2243250) and IL-6 (− 174G/C) (rs1800795) polymorphism and the serum levels of IL-4 and IL-6 in chronic kidney disease (CKD).
Methods
The IL-4 (− 590C/T) and IL-6 (− 174 G/C) polymorphisms were genotyped in 132 CKD patients and 161 controls using PCR–RFLP. Serum IL-4 and IL-6 quantifications were performed by ELISA.
Results
Significant susceptible associations of CT genotype (OR = 4.56; p < 1.84 × 10–9) and T allele (OR = 1.56; p < 0.010) of IL-4 (− 590C/T) and CC genotype (OR = 2.63; p < 0.032) of IL-6 (− 174G/C) were observed for CKD. The CC genotype (OR = 0.27; p < 9.314 × 10–7) and C allele (OR = 0.63; p < 0.010) of IL-4 (− 590 C/T) revealed strong protective associations. Five-fold increased levels were observed for both IL-6 (p < 0.0001) and IL-4 (p < 0.0043) cytokines in CKD patients than the controls. The IL-4 serum levels (pg/ml) increased significantly in patients with CT and TT genotypes of IL-4 (− 590 C/T) than the controls (6.18 ± 1.80 vs. 3.33 ± 0.48 and 6.14 ± 1.96 vs. 3.21 ± 0.56 respectively). For IL-6 (− 174 G/C) polymorphism, the patients with CC genotype (6.50 ± 1.30 vs. 3.49 ± 1.39) revealed with higher IL-6 serum levels followed by GC genotype (5.00 ± 1.91 vs. 4.01 ± 1.74).
Conclusion
The genotypes of IL-4 (590 C/T) and IL-6 (174 G/C) polymorphisms contribute differential susceptibility in south Indian CKD patients. A fivefold increased serum levels of IL-4 (anti-inflammatory) and IL-6 (pro- and anti-inflammatory) cytokines were documented in CKD patients. There observed an opposite trend in disease association for these two cytokines and associated SNPs with CKD in south India.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a disease showing progressive loss of renal function, with decline in the estimated glomerular filtration rate (eGFR) (stages 1–5), that required either dialysis or kidney replacement therapy (KRT) [8, 39, 81]. The measurement of creatinine and urea helps to assess the renal function by reflecting the glomerular filtration rate (GFR). The calculation of the urea: creatinine ratio is help establishing a renal and/or non-renal cause. Cytokines are factors mainly influencing the atherosclerosis leading to CKD and subsequent ESRD [65]. The stability between anti-and/or pro-inflammatory cytokines determines the inflammatory response and mediates the progression of CKD [6]. These pro-inflammatory (IL-1, IL-6 and TNF-a) and anti-inflammatory (IL-4, IL-10 and IL-13) cytokines play essential roles in the development of CKD pathogenesis. Previous reports have documented a wide spectrum of impact of different cytokines on the glomerular basement membrane of kidneys in different populations [13, 15, 82]. Further, the polymorphism (SNPs) present within the coding and non-coding regions of cytokine genes may cause inter individual variation in their expression, leading to individual differences in immune responses leading to CKD [2, 43, 60, 66, 68]. The single nucleotide polymorphisms (SNPs) within the promoter region of these cytokine genes were reportedly influence the cytokine levels [73]. The cytokine gene promoter polymorphism vary among different ethnic groups and may contribute differently in disease processes and pathology [23, 36, 47, 78]. Further, the differences in graft survival rates among Black and other world populations have suggested the strong role of cytokines. However, other confounding issues such as socioeconomic factors, therapeutic compliance and immunological variables too contribute significantly.
The gene for IL-6 gene is located on human chromosome 7p15–p21 and the interleukin is primarily produced by T cells and macrophages [18]. The IL-6 is secreted by a number of cells including lymphocytes, adipocytes, macrophages, endothelial cells and fibroblasts. This cytokine has the ability to induce endothelial damage, stimulating the intracellular adhesion molecule-1 (ICAM-1) and enhancing the migration of leucocytes across the endothelial surfaces [56]. IL-6 cytokine has dual roles, and it exhibits both pro-anti-inflammatory effects [46]. The pro-inflammatory cytokines (IL-6) and tumour necrosis factor-α (TNF-α) were the key orchestrators of inflammatory response. Thus, these cytokines acted as key factors that accelerated atherogenesis, morbidity and mortality in kidney failure patients undergoing haemodialysis [3].
Recent studies have documented a clear correlation between expression of IL-6 and acute kidney injury (AKI). The cells such as mesangial, endothelial, podocytes and tubular epithelial (TECs) can secrete IL-6 under certain clinical conditions. The high glucose level induces IL-6 dependent secretion and stimulates IL-6 signal transduction in podocytes. This was inferred by blocking IL-6 and its downstream mediators such as IL-6R and gp130 attenuating the progression of diabetic nephropathy [33]. The reduced clearance of IL-6 as a consequence of impaired renal function also contributes to its accumulation. Further, the elevated IL-6 level could be attributed to oxidative stress, chronic inflammation and fluid overload. In ESRD patients, the therapeutic hemodialysis and peritoneal dialysis too stimulate IL-6 production and increased level of inflammatory response [4, 57, 71].
Previous studies have documented the association of polymorphisms in IL-6 promoter regions such as 572 G/C, 634 C/G, 174 G/C and 597 G/A with several diseases [60]. Among these, IL-6 (174 G/C) regulate a broad range of immune activities such as production of acute phase proteins and cell adhesion molecules that in turn orchestrated the release of other cytokines in response to inflammatory stimuli [34]. The 174G/C polymorphism in IL-6 gene revealed an independent risk factor for diabetic nephropathy in Greek and Turkish T2DM patients [31, 55]. The IL-6 (174-G/C) polymorphism has been reported to influence IL-6 expression, particularly the G allele being associated with accelerated expression [17, 26, 58, 72, 77]. Interestingly, IL-6 (174 G/C) polymorphism has reportedly been associated in a number of chronic diseases including arthritis, coronary heart disease and diabetes [16, 17, 83]. The higher level of IL-6 (− 174 G/C) was associated with advanced carotid plaques [21]. However, no significant correlation of − 174G/C polymorphism with ESKD was documented [15].
The IL-4 gene is 0.9 kb long and consists 4 exons located on chromosome 5 (5q31) along with other Th2-related cytokine genes (IL-3, -5, -9, -13 and -15) [38, 48]. IL-4 is an anti-inflammatory cytokine mainly involved in adaptive immunity and inhibits the secretion of IL-1, IL-6 and pro-inflammatory tumor necrosis factor (TNF) that in turn effectively down regulates macrophage function and stimulates the proliferation of activated T and B cells, regulates the differentiation of B cells, promotes type-2 T helper (Th2) cell activity and inhibits Th1 cell differentiation [50, 54, 62, 76]. The increased production of IL-4 is associated with reduced inflammation in CKD rats [69]. Further, in mouse model depicting inflammatory renal disease, the adoptive transfer of IL-4 induced M2 macrophages significantly reduces histological injury [80]. A number of previous studies too have implicated the IL-4 (590 C/T) (rs2243250) promoter region polymorphism with atopic dermatitis [40], multiple sclerosis, rheumatoid arthritis [59] and atopic asthma [41].
The present study was to investigate the association of SNPs in IL-4 (590 C/T) and IL-6 (174 G/C) polymorphisms and to correlate the serum levels of these cytokines with CKD pathogenesis in a south Indian CKD cohort.
Materials and methods
Enrollment of samples
A total of 132 CKD patients and 161 healthy controls were enrolled during 2017–2019. The subjects were recruited from private hospitals in and around Madurai, Tamil Nadu. Enrolment of CKD patient was done under the supervision of the physician as per the guidelines of Kidney Disease Quality Outcome Initiative [51]. The present CKD study groups include dialysis, non-dialysis and post-transplant subjects with and without complications in the age group > 15 years. Pregnant women, AIDS and pediatric kidney failure cases were excluded. The healthy volunteers were selected randomly from the same geographical region without any major medical illness. A questionnaire was obtained from each patient and written informed consent was obtained from all the participants. The study was approved by the Institutional Ethical Committee (Ref. No: version 04 MMHRC-IEC).
IL-6 and IL-4 cytokines serum levels
Three ml blood was collected in vacutainer and centrifuged at 2000 rpm for 10 min for serum separation. The separated serum was stored at – 80 °C in cryovials until further analysis. To measure the serum levels of IL-6 and IL-4, an enzyme-linked immunosorbent assay (ELISA) was performed for 50 CKD patients and 50 controls using cytokine detection kits (Bioassay Technology Laboratory, China).
Detection of IL-4 and IL-6 SNPs
To detect IL-4 (590C/T) and IL-6 (174 G/C) gene polymorphism, all DNA samples were tested by PCR–RFLP method as described previously with slight modifications [32]. The following primers were used for IL-4 (590 C/T): F: 5′-TAAACTTGGGAGAACATGGT, R: 5′-TGGGGAAAGATAGAGTAATA; and for IL-6 (174 G/C) F: 5′-TAGCCTCAATGACGACCTAAGCT-3′; R: 5′-GGGCTGATTGGAAACCTTATTAAG-3′. PCR reactions were performed in a volume of 12 µl containing 50 ng of genomic DNA, 0.24 mM dNTP, 0.04 U of Taq polymerase, 10X buffer, and 0.5 µm forward and reverse primers. The PCR conditions with initial denaturation at 95 °C for 5 min, followed by 30 cycles of 94 °C for 30 s, annealing at 55 °C for 30 s, and extension of 72 °C for 30 s with a final extension at 72 °C for 5 min were followed. The amplified PCR products was analyzed by 1.5% agarose gel electrophoresis. The amplified products of 252 bp product of IL-4 (590 C/T) were digested with AvaII (TT: 252 bp; GC: 252 + 192 + 60 bp; CC: 192 + 60 bp) and 532 bp product of IL-6 (174 G/C) was digested with BsmF1 (GG: 532 bp; GC: 532 + 474 + 58 bp; CC: 474 + 58 bp) enzyme and electrophorosed on 3% agarose gel at 100 V for 20 min. The digested products were detected in a Gel Documentation System (Vilbert Lourmat, France).
Statistical analysis
The cytokine levels were measured by Mann–Whitney test using Graphpad prism software. The Chi square test was used to test the deviation from Hardy–Weinberg Equilibrium (HWE) by comparing the observed and expected frequencies. The sample size of the study was calculated as described previously [5, 28]. The association between IL-4 (590C/T) and IL-6 (174 G/C) gene polymorphism with CKD was determined by using the Odds Ratio (OR) and 95% confidence intervals. The p value < 0.05 was considered statistically significant. Clinical characteristics are compared by using the Student unpaired t- test and the χ2 test.
Results
Demographic characteristics
A total of 132 CKD patients (108 males; average age: 50.69 ± 15.29 years and 24 females; average age: 48.41 ± 15.53 years) and 161 healthy controls (96 males; average age: 43.34 ± 13.11 years; and 65 females; average age: 40.06 ± 13.15 years) were enrolled for the study. The study cohorts consisted more of males than females, attesting the fact of higher incidence of CKD in males [7, 22]. The clinical parameters such as urea (114.75 ± 35.97 mg/dl; range: 35–243 mg/dl), serum creatinine (7.99 ± 3.45 mg/dl; range: 1.8–40.1 mg/dl), and hemoglobin (8.92 ± 1.74 g/dl; range: 5.2–13.6 g/dl) were documented. The estimated glomerular filtration rate (eGFR) for the study cohort was 11.15 ± 11.93 ml/min/1.73 m2). The most common documented comorbidities among the study subjects were diabetes, hypertension, cardiomyopathy and stroke. Ninety percent of (90.90%; n = 119) patients had undergone dialysis and the remaining 9.09% (n = 14) patients falls under non-dialysis group. Patients with Diabetic-CKD (39.9%; n = 60) and Non-diabetic-CKD (48.54%; n = 73) were analyzed separately.
Serum cytokine levels
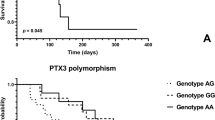
Circulating serum levels of IL-4 and IL-6 cytokines in CKD patients and healthy controls were measured by ELISA method (pg/ml). We observed a significantly increased level of IL-4 and IL-6 cytokines in CKD patients than the controls (Fig. 1). Further, gender-based analyses have not revealed any significant variations (Table 1). The correlation analysis of serum IL-4 level and IL-4 (− 590C/T) genotypes have revealed higher IL-4 cytokine levels in CKD patients with CT genotype (p < 0.0001) followed by TT (0.028) genotype (data not shown). The CKD patients with CC genotype revealed moderately elevated serum level of IL-4. Similarly, serum level of the IL-6 in relation to IL-6 (− 174G/C) genotypes have revealed an higher IL-6 levels in CKD patients with CC genotype followed by the GG genotype as compared to serum levels in the controls (Fig. 2B; Table 2).
Genotype/allele frequencies of IL-4 (590 C/T) and IL-6 (174 G/C) polymorphism
The genotype and allele frequencies of IL-4 (590 C/T) and IL-6 (174 G/C) gene polymorphism for pooled (P), male (M) and female (F) CKD patients were presented (Table 3). We observed a significantly increased frequencies of heterozygous CT genotype (P: OR = 4.56; p < 1.84 × 10−9; M: OR = 4.17; p < 2.97 × 10−6; F: OR = 6.33; p < 5.72 × 10−4) and T allele (P: OR = 1.56; p < 0.010) of IL-4 (590 C/T) gene polymorphism in CKD pooled patients. Further, decreased frequencies of CC genotype (P: OR = 0.27; p < 9.314 × 10−7; M: OR = 0.30; p < 1.98 × 10−4; F: OR = 0.18; p < 0.004) and C allele (P: OR = 0.637; p < 0.010) revealed significant association. We observed a weak protective association for TT genotype (OR = 0.439; p < 0.059) in CKD patients, however, without a statistical significance. Similarly, an increased frequency of CC genotype (OR = 2.63; p < 0.032) and a decreased frequency of GC genotype (OR = 0.54; p < 0.021) of IL-6 (174 G/C) among CKD patients were documented. No significant gender-based differences were observed for IL-6 (− 174 G/C) genotypes.
Genetic model analysis
The disease association analyses based on genetic models for IL-6 (174 G/C) and IL-4 (590 C/T) genotypes with CKD susceptibility were presented (Table 3). For IL-6 (174 G/C) genotypes, a significantly increased risk of CKD susceptibility was observed for Recessive (OR = 2.638; p < 0.993) and Additive (OR = 1.892; p < 0.239) models, however, without a statistical significance. Nonetheless, a significant protective association was observed for Co-dominant model (OR = 0.543; p < 0.017). Whereas for IL-4 (590 C/T) genotypes, there observed an increased risk of association for Dominant (OR = 3.763; p < 0.000) and Co-dominant (OR = 4.560; p < 0.000) models. Interestingly, a significant protective association was observed for Recessive model (OR = 0.272; p < 0.000) (Table 4). Thus, there observed to be an opposite trend in disease associations for these two cytokine markers with CKD in south India.
Discussion
Inflammation is one of the common factors to increase with the severity of the CKD disease. The cytokine SNPs and their genotypes have been associated with unfavorable outcomes in patients undergoing organ transplantation. Expression level of cytokines can be influenced by polymorphisms (SNPs) in the genes encoding these cytokines, as demonstrated for IL-1 [63], IL-10 [10, 75], IL-6 [67] and IL-4 [20]. Certain polymorphisms such as HLA alleles (MHC) [64], allograft inflammatory factor-1 (AIF-1) [79], RANTES/CCL5 [35], CTLA4 and TLR4 gene products [19] have all been implicated in acute graft dysfunction (GD), acute rejection (AR) and graft dysfunction (GD).
IL-4 is a multifunctional cytokine and negatively regulates proinflammatory cytokine production in renal inflammation. The study results have revealed a significant disease association of CT genotype and T allele of IL-4 (590 C/T) polymorphism in CKD patients. The genetic model analyses have revealed susceptible association for ‘dominant’ and ‘co-dominant’ models in IL-4 (590 C/T). However, we observed a susceptible association of ‘recessive’ and ‘additive’ models for IL-6 without statistical significance. Thus, genetic model analyses have presented a diverse trend for these cytokines in CKD. Present observations are in concordance with earlier reports in north Indian population that documented the increased frequency of T allele and TT genotype of IL-4 (− 590 C/T) in diabetic CKD cases than the controls. However, no significant differences in allele frequencies were observed in CKD patients without T2DM. Thus, the presence of T allele of IL-4 (− 590 C/T) gene polymorphism is associated with increased risk of diabetic CKD [52].
The T allele of IL-4 (590 C/T) polymorphism influenced the prognosis and the clinical course of the disease in INS patients from North India [25]. It has been documented earlier IL-4 (590 C/T) polymorphism was reportedly associated with the susceptibility to ESRD patients from north India [49]. A significant association was documented in IL-4 (590 C/T) in T2DM patients with diabetic nephropathy (DN) from Rafsanjan population from southeast Iran [30]. In another study from a Japanese population, IL-4 polymorphism was shown to be associated with the progression in immunoglobulin mediated nephropathy [44]. However, no significant differences were documented between IL-4 (590 C/T) allele distribution in Caucasians (UK) and Kuwait idiopathic nephritic syndrome (INS) patients [1, 53]. The frequency of T allele was significantly lower in Japanese Children with INS [32]. Further, it has been reported that T allele of the IL-4 (590 C/T) polymorphism was strongly associated with increased IL-4 gene promoter activity [27, 29]. We observed a striking male:female difference in cytokine levels with reference to this SNP, substantiating the predominance of CKD in males. The gender-based disease associations were exceedingly pronounced for CC (OR = 0.305) genotype towards protective and for CT (OR = 4.174) genotype towards susceptible associations.
The data presented here documented a significant association for CC genotype of IL-6 (174 G/C) polymorphism. We observed a higher risk of association in ‘recessive’ and ‘additive’ models, however, without statistical significance. The protective association of ‘co-dominant’ model for IL-6 (174 G/C) polymorphism reiterated the significance of its pro-inflammatory role in disease process. Several previous reports have documented IL-6 (174 G/C) polymorphism as a predictive marker for the progression of complications, especially in kidney patients with T2DM disease [74]. Some previous studies involving patients with other inflammatory clinical entities have reported CC genotype as protective, as it maintains lower circulating levels of IL-6 [17, 42]. An association of GG and GC genotypes with increased IL-6 levels than the CC genotype in Caucasian and African American ESRD patients undergoing long-term dialysis was reported [2]. Further, it is interesting to note that the individuals with higher IL-6 production were shown to be at increased risk for acute organ rejection episodes [9, 45]. The development of oxidative stress, accumulation of uremic toxins, fluid overload with other CKD related manifestations may contribute to this rise in plasma IL-6 levels and hence the observed higher degree of inflammation. The dialysis procedure also contributes to the inflammatory response, thereby increasing IL-6 production. It has been reported that the hemodialysis (HD) may increase the production of cytokines of pro-inflammatory immune response [61]. Further, chronic HD patients were shown to exhibit increased inflammation as pro-inflammatory mediators were released in uremic milieu [11].
Conclusions
Our findings suggest that polymorphisms at the anti-inflammatory IL-4 and pro-inflammatory IL-6 cytokines could be a useful predictor for CKD diagnosis and prognosis. The limitation of our study is the relatively small number of patients examined for these circulating inflammatory markers. Hence, future investigation with larger cohort is necessary to confirm these findings and to translate these observations into deliverables in clinical management of CKD. A clear understanding of cytokine dynamics will facilitate better clinical management of highly debilitating diseases such as chronic kidney disease in a transplantation setting.
Availability of data and materials
We do have all the research data required for the manuscript and we will provide all the data and material for the publication.
References
Al Rushood M, Al-Eisa AA, Haider MZ (2020) Interleukin-4 and interleukin-13 gene polymorphisms in children with idiopathic nephrotic syndrome. Front Pediatr 8:591349. https://doi.org/10.3389/fped.2020.591349
Balakrishnan VS, Guo D, Rao M, Jaber BL, Tighiouart H, Freeman RL, Huang C, King AJ, Pereira BJ, HEMO Study Group (2004) Cytokine gene polymorphisms in hemodialysis patients: association with comorbidity, functionality, and serum albumin. Kidney Int 65(4):1449–1460. https://doi.org/10.1111/j.1523-1755.2004.00531.x
Bologa RM, Levine DM, Parker TS et al (1998) Interleukin-6 predicts hypoalbuminemia, hypocholesterolemia, and mortality in hemodialysis patients. Am J Kid Dis 32:107–114. https://doi.org/10.1053/ajkd.1998.v32.pm9669431
Caglar K, Peng Y, Pupim LB, Flakoll PJ, Levenhagen D, Hakim RM et al (2002) Inflammatory signals associated with hemodialysis. Kidney Int 62(4):1408–1416
Cai J, Zeng D (2004) Sample size/power calculation for case-cohort studies. Biometrics 60(4):1015–1024
Carrero JJ, Park SH, Axelsson J, Lindholm B, Stenvinkel P (2009) Cytokines, atherogenesis, and hypercatabolism in chronic kidney disease: a dreadful triad. Semin Dial 22(4):381–386. https://doi.org/10.1111/j.1525-139X.2009.00585.x
Carrero JJ, Hecking M, Chesnaye NC, Jager KJ (2018) Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol 14(3):151–164
Corredor Z, Filho M, Rodríguez-Ribera L, Velázquez A, Hernández A, Catalano C, Hemminki K, Coll E, Silva I, Diaz JM, Ballarin J, Vallés Prats M, Calabia Martínez J, Försti A, Marcos R, Pastor S (2020) Genetic variants associated with chronic kidney disease in a Spanish population. Sci Rep 10(1):144. https://doi.org/10.1038/s41598-019-56695-2
Cox ED, Hoffmann SC, DiMercurio BS et al (2001) Cytokine polymorphic analyses indicate ethnic differences in the allelic distribution of in-terleukin-2 and interleukin-6. Transplantation 72:720–726
Crawley E, Woo P, Isenberg DA (1999) Single nucleotide polymorphic haplotypes of the interleukin-10 5’ flanking region are not associated with renal disease or serology in Caucasian patients with systemic lupus erythematosus. Arthritis Rheum 42(9):2017–2018. https://doi.org/10.1002/1529-0131(199909)42:9%3c2017::AID-ANR34%3e3.0.CO;2-I
Cobo G, Lindholm B, Stenvinkel P (2018) Chronic inflammation in end-stage renal disease and dialysis. Nephrol Dial Transpl 33(3):iii35–iii40
Cui ZH, Lu XT, **ao KL, Chen Y, Li HQ (2019) Association of interleukin-6 -174G/C polymorphism with the risk of diabetic nephropathy in type 2 diabetes: a meta-analysis. Curr Med Sci 39(2):250–258. https://doi.org/10.1007/s11596-019-2027-1
Davin JC (2016) The glomerular permeability factors in idiopathic nephrotic syndrome. Pediatr Nephrol 31(2):207–215. https://doi.org/10.1007/s00467-015-3082-x
Fathy SA, Mohamed MR, Ali M, El-Helaly AE, Alattar AT (2019) Influence of IL-6, IL-10, IFN-γ and TNF-α genetic variants on susceptibility to diabetic kidney disease in type 2 diabetes mellitus patients. Biomarkers 24(1):43–55. https://doi.org/10.1080/1354750X.2018.1501761
Fang X, Zhu Z, Yang S, Ji Y, Wang L (2016) Association of IL-4 and IL-4 receptor gene polymorphisms with the risk, immunotherapeutic effects and prognosis of advanced renal cell carcinoma. Int J Clin Exp Med 9:11449–11457
Fernández-Real JM, Broch M, Vendrell J, Gutiérrez C, Casamitjana R, Pugeat M, Richart C, Ricart W (2000) Interleukin-6 gene polymorphism and insulin sensitivity. Diabetes 49(3):517–520. https://doi.org/10.2337/diabetes.49.3.517
Fishman D, Faulds G, Jeffery R, Mohamed-Ali V, Yudkin JS, Humphries S, Woo P (1998) The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Investig 102(7):1369–1376. https://doi.org/10.1172/JCI2629
Fisman EZ, Tenenbaum A (2010) The ubiquitous interleukin-6: a time for reappraisal. Cardiovasc Diabetol 9:62. https://doi.org/10.1186/1475-2840-9-62
Funami K, Matsumoto M, Oshiumi H, Inagaki F, Seya T (2017) Functional interfaces between TICAM-2/TRAM and TICAM-1/TRIF in TLR4 signaling. Biochem Soc Trans 45:929–935
Gonzales JR, Gröger S, Haley G, Bödeker RH, Meyle J (2010) The interleukin-4 -34TT and -590TT genotype is correlated with increased expression and protein production in aggressive periodontitis. Mol Immunol 47(4):701–705. https://doi.org/10.1016/j.molimm.2009.10.025
Hassan MO, Duarte R, Dickens C, Dix-Peek T, Naidoo S, Vachiat A, Grinter S, Manga P, Naicker S. Interleukin-6 gene polymorhisms and interleukin-6 levels are associated with atherosclerosis in CKD patients. Clin Nephrol. 2020;93(1):82–86. https://doi.org/10.5414/CNP92S114.
Hecking M, Bieber BA, Ethier J, Kautzky-Willer A, Sunder-Plassmann G, Saemann MD et al (2014) Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the dialysis outcomes and practice patterns study (DOPPS). PLOS Med 11(10):e1001750
Hoffmann SC, Stanley EM, Cox ED, DiMercurio BS, Koziol D, Harlan DM et al (2002) Ethnicity greatly influences cytokine gene polymorphism distribution. Am J Transpl 2:560–567
Howell MW (2013) Interleukin-10 gene polymorphisms and cancer. Madame Curie Bioscience Database [internet]. Landes Bioscience
Jafar T, Agrawal S, Mahdi AA, Sharma RK, Awasthi S, Agarwal GG (2011) Cytokine gene polymorphism in idiopathic nephrotic syndrome children. Indian J Clin Biochem IJCB 26(3):296–302. https://doi.org/10.1007/s12291-011-0126-2
Joffe YT, Collins M, Goedecke JH (2013) The relationship between dietary fatty acids and inflammatory genes on the obese phenotype and serum lipids. Nutrients 5(5):1672–1705. https://doi.org/10.3390/nu5051672
Jun TY, Lee KU, Pae CU, Chae JH, Bahk WM, Kim KS, Han H (2003) Polymorphisms of interleukin-4 promoter and receptor gene for schizophrenia in the Korean population. Psychiatry Clin Neurosci 57(3):283–288. https://doi.org/10.1046/j.1440-1819.2003.01118.x
Kasiulevicius V, Sapoka V, Filipaviciute R (2006) Sample size calculation in epidemiologicalstudies. Gerontology 7:225–231
Kawashima T, Noguchi E, Arinami T, Yamakawa-Kobayashi K, Nakagawa H, Otsuka F, Hamaguchi H (1998) Linkage and association of an interleukin 4 gene polymorphism with atopic dermatitis in Japanese families. J Med Genet 35(6):502–504. https://doi.org/10.1136/jmg.35.6.502
Kazemi AM (2010) Interleukin-4 gene polymorphisms in type 2 diabetic patients with nephropathy. Iran J Kidney Dis 4(4):302–306
Karadeniz M, Erdogan M, Berdeli A, Yilmaz C (2014) Association of interleukin-6 -174 G>C promoter polymorphism with increased risk of type 2 diabetes mellitus patients with diabetic nephropathy in Turkey. Genet Test Mol Biomarkers 18:62–65
Kobayashi Y, Arakawa H, Suzuki M, Takizawa T, Tokuyama K, Morikawa A (2003) Polymorphisms of interleukin-4–related genes in Japanese children with minimal change nephrotic syndrome. Am J Kidney Dis 42(2):271–276. https://doi.org/10.1016/s0272-6386(03)00652-8
Kim DI, Park SH (2013) Sequential signaling cascade of IL-6 and PGC-1alpha is involved in high glucose-induced podocyte loss and growth arrest. Biochem Biophys Res Commun 435:702–707
Kristiansen OP, Mandrup-Poulsen T (2005) Interleukin-6 and diabetes: the good, the bad, or the indifferent? Diabetes 54(Suppl 2):S114–S124. https://doi.org/10.2337/diabetes.54.suppl_2.s114
Kruger B, Boger CA, Obed A et al (2007) RANTES/CCL5 polymorphisms as a risk factor for recurrent acute rejection. Clin Transpl 21:385–390
Kuffner T, Whitworth W, Jairam M, McNicholl J (2003) HLA class II and TNF genes in African Americans from the Southeastern United States: regional differences in allele frequencies. Hum Immunol 64:639–647
Lara-Gómez RE, Moreno-Cortes ML, Muñiz-Salazar R, Zenteno-Cuevas R (2019) Association of polymorphisms at -174 in IL-6, and -308 and -238 in TNF-α, in the development of tuberculosis and type 2 diabetes mellitus in the Mexican population. Gene 702:1–7. https://doi.org/10.1016/j.gene.2019.03.050
Le Beau MM, Lemons RS, Espinosa R 3rd, Larson RA, Arai N, Rowley JD (1989) Interleukin-4 and interleukin-5 map to human chromosome 5 in a region encoding growth factors and receptors and are deleted in myeloid leukemias with a del(5q). Blood 73(3):647–650
Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU (2011) The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int 80(1):17–28. https://doi.org/10.1038/ki.2010.483
Liang J, Liu Y, Xue R, Chen L, Chen H, Shao L, Wang J, Zhang X (2017) Interleukin 4–590C/T (rs2243250) polymorphism is associated with increased risk of atopic dermatitis: meta-analysis of case-control studies. Dermat Contact Atopic Occup Drug 28(2):144–151. https://doi.org/10.1097/DER.0000000000000265
Liu S, Li T, Liu J (2012) Interleukin-4 rs2243250 polymorphism is associated with asthma among Caucasians and related to atopic asthma. Cytokine 59(2):364–369. https://doi.org/10.1016/j.cyto.2012.05.006
Libra M, Signorelli SS, Bevelacqua Y, Navolanic PM, Bevelacqua V, Polesel J, Talamini R, Stivala F, Mazzarino MC, Malaponte G (2006) Analysis of G(-174)C IL-6 polymorphism and plasma concentrations of inflammatory markers in patients with type 2 diabetes and peripheral arterial disease. J Clin Pathol 59(2):211–215. https://doi.org/10.1136/jcp.2004.025452
Luttropp K, Lindholm B, Carrero JJ, Glorieux G, Schepers E, Vanholder R, Schalling M, Stenvinkel P, Nordfors L (2009) Genetics/genomics in chronic kidney disease–towards personalized medicine? Semin Dial 22(4):417–422. https://doi.org/10.1111/j.1525-139X.2009.00592.x
Masutani K, Miyake K, Nakashima H, Hirano T, Kubo M, Hirakawa M, Tsuruya K, Fukuda K, Kanai H, Otsuka T, Hirakata H, Iida M (2003) Impact of interferon-gamma and interleukin-4 gene polymorphisms on development and progression of IgA nephropathy in Japanese patients. Am J Kidney Dis 41(2):371–379. https://doi.org/10.1053/ajkd.2003.50046
Marshall SE, McLaren AJ, Haldar NA, Bunce M, Morris PJ, Welsh KI (2000) The impact of recipient cytokine genotype on acute rejection after renal transplantation. Transplantation 70:1485–2149
Mauer J, Denson JL, Brüning JC. Versatile functions for IL-6 in metabolism and cancer. Trends Immunol. 2015;36(2):92–101. https://doi.org/10.1016/j.it.2014.12.008.
Meenagh A, Williams F, Ross OA, Patterson C, Gorodezky C, Hammond M et al (2002) Frequency of cytokine polymorphisms in populations from western Europe, africa, Asia, the Middle East and south America. Hum Immunol 63:1055–1061
Mire-Sluis AR (1998) Interleukin-4. In: Cytokines. Academic Press, London, pp 53–68
Mittal RD, Manchanda PK (2007) Association of interleukin (IL)-4 intron-3 and IL-6 -174 G/C gene polymorphism with susceptibility to end-stage renal disease. Immunogenetics 59(2):159–165. https://doi.org/10.1007/s00251-006-0182-6
Mosmann TR, Coffman RL (1989) TH1 and TH2 cells: different patterns of lymphokine secretion lead to different functional properties. Annu Rev Immunol 7:145–173. https://doi.org/10.1146/annurev.iy.07.040189.001045
National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis. 2012;60(5):850-86. https://doi.org/10.1053/j.ajkd.2012.07.005.
Neelofar K, Ahmad J, Ahmad A, Alam K (2017) Study of IL4-590C/T and IL6-174G/C gene polymorphisms in type 2 diabetic patients with chronic kidney disease in North Indian population. J Cell Biochem 118(7):1803–1809. https://doi.org/10.1002/jcb.25853
Parry RG, Gillespie KM, Parnham A, Clark AG, Mathieson PW (1999) Interleukin-4 and interleukin-4 receptor polymorphisms in minimal change nephropathy. Clin Sci 96(6):665–668
Paul WE (1991) Interleukin-4: a prototypic immunoregulatory lymphokine. Blood 77(9):1859–1870
Papaoikonomou S, Tentolouris N, Tousoulis D, Papadodiannis D, Miliou A, Papageorgiou N et al (2013) The association of the 174G>C polymorphism of interleukin 6 gene with diabetic nephropathy in patients with type 2 diabetes mellitus. J Diabetes Complicat 27:576–579
Piggott R, Dillon LP, Hemingway IH, Gearing AJ (1992) Soluble forms of E-selectin, ICAM-1 and VCAM-1 are present in the supernatants of cytokine activated cultured endothelial cells. Biochem Biophys Res Commun 187(2):584–589. https://doi.org/10.1016/0006-291x(92)91234-h
Pecoits-Filho R, Heimburger O, Barany P, Suliman M, Fehrman-Ekholm I, Lindholm B et al (2003) Associations between circulating inflammatory markers and residual renal function in CRF patients. Am J Kidney Dis 41:1212–1218
Popko K, Gorska E, Demkow U (2010) Influence of interleukin-6 and G174C polymorphism in IL-6 gene on obesity and energy balance. Eur J Med Res 15(2):123–127. https://doi.org/10.1186/2047-783x-15-s2-123
Qiu LJ, Ni J, Cen H, Wen PF, Zhang M, Liang Y, Pan HF, Mao C, Ye DQ (2015) Relationship between the IL-4 gene promoter -590C/T (rs2243250) polymorphism and susceptibility to autoimmune diseases: a meta-analysis. J Eur Acad Dermatol Venereol JEADV 29(1):48–55. https://doi.org/10.1111/jdv.12435
Rao M, Wong C, Kanetsky P, Girndt M, Stenvinkel P, Reilly M, Raj DS (2007) Cytokine gene polymorphism and progression of renal and cardiovascular diseases. Kidney Int 72(5):549–556. https://doi.org/10.1038/sj.ki.5002391
Rysz J, Banach M, Cialkowska-Rysz A, Stolarek R, Barylski M, Drozdz J, Okonski P. Blood serum levels of IL-2, IL-6, IL-8, TNF-alpha and IL-1beta in patients on maintenance hemodialysis. Cell Mol Immunol. 2006;3(2):151–4.
Seder RA, Paul WE, Davis MM, de St F, Groth B (1992) The presence of interleukin 4 during in vitro priming determines the lymphokine-producing potential of CD4+ T cells from T cell receptor transgenic mice. J Exp Med 176(4):1091–1098. https://doi.org/10.1084/jem.176.4.1091
Shirodaria S, Smith J, McKay IJ, Kennett CN, Hughes FJ (2000) Polymorphisms in the IL-1A gene are correlated with levels of interleukin-1alpha protein in gingival crevicular fluid of teeth with severe periodontal disease. J Dent Res 79(11):1864–1869. https://doi.org/10.1177/00220345000790110801
Sheldon S, Hasleton PS, Yonan NA et al (1994) Rejection in heart transplantation strongly correlates with HLA-DR antigen mismatch. Transplantation 58:719–722
Silverstein DM (2009) Inflammation in chronic kidney disease: role in the progression of renal and cardiovascular disease. Pediatr Nephrol (Berlin, Germany) 24(8):1445–1452. https://doi.org/10.1007/s00467-008-1046-0
Stern DL (2000) Evolutionary biology. The problem of variation. Nature 408(6812):529–531. https://doi.org/10.1038/35046183
Smith AJ, D’Aiuto F, Palmen J, Cooper JA, Samuel J, Thompson S, Sanders J, Donos N, Nibali L, Brull D, Woo P, Humphries SE (2008) Association of serum interleukin-6 concentration with a functional IL6 -6331T>C polymorphism. Clin Chem 54(5):841–850. https://doi.org/10.1373/clinchem.2007.098608
Smith AJ, Humphries SE (2009) Cytokine and cytokine receptor gene polymorphisms and their functionality. Cytokine Growth Factor Rev 20(1):43–59. https://doi.org/10.1016/j.cytogfr.2008.11.006
Souza MK, Neves RVP, Rosa TS, Cenedeze MA, Arias SCA, Fujihara CK et al (2018) Resistance training attenuates inflammation and the progression of renal fibrosis in chronic renal disease. Life Sci 206:93–97
Spoto B, Mattace-Raso F, Sijbrands E, Leonardis D, Testa A, Pisano A, Pizzini P, Cutrupi S, Parlongo RM, D’Arrigo G, Tripepi G, Mallamaci F, Zoccali C (2015) Association of IL-6 and a functional polymorphism in the IL-6 gene with cardiovascular events in patients with CKD. Clin J Am Soc Nephrol CJASN 10(2):232–240. https://doi.org/10.2215/CJN.07000714
Takahashi T, Kubota M, Nakamura T, Ebihara I, Koide H (2000) Interleukin-6 gene expression in peripheral blood mononuclear cells from patients undergoing hemodialysis or continuous ambulatory peritoneal dialysis. Ren Fail 2000(22):345–354
Terry CF, Loukaci V, Green FR (2000) Cooperative influence of genetic polymorphisms on interleukin 6 transcriptional regulation. J Biol Chem 275(24):18138–18144. https://doi.org/10.1074/jbc.M000379200
Tindall EA, Severi G, Hoang HN, Ma CS, Fernandez P, Southey MC, English DR et al (2010) Australian prostate cancer BioResource: comprehensive analysis of the cytokine-rich chromosome 5q31.1 region suggests a role for IL-4 gene variants in prostate cancer risk. Carcinogenesis 31:1748–1754
Thandavan T, Abraham G, Soundararajan P et al (2015) Interleukin 6 strongly correlates with malnutrition inflammation score and it is strong predictor for mortality in hemodialysis patients. Urol Nephrol Open Access J 2(2):40–42. https://doi.org/10.15406/unoaj.2015.02.00030
Turner D, Grant SC, Yonan N, Sheldon S, Dyer PA, Sinnott PJ, Hutchinson IV (1997) Cytokine gene polymorphism and heart transplant rejection. Transplantation 64(5):776–779. https://doi.org/10.1097/00007890-199709150-00021
Vitetta ES, Ohara J, Myers CD, Layton JE, Krammer PH, Paul WE (1985) Serological, biochemical, and functional identity of B cell-stimulatory factor 1 and B cell differentiation factor for IgG1. J Exp Med 162(5):1726–1731. https://doi.org/10.1084/jem.162.5.1726
Vickers MA, Green FR, Terry C, Mayosi BM, Julier C, Lathrop M, Ratcliffe PJ, Watkins HC, Keavney B (2002) Genotype at a promoter polymorphism of the interleukin-6 gene is associated with baseline levels of plasma C-reactive protein. Cardiovasc Res 53(4):1029–1034. https://doi.org/10.1016/s0008-6363(01)00534-x\
Visentainer JE, Sell AM, da Silva GC, Cavichioli AD, Franceschi DS, Lieber SR et al (2008) TNF, IFNG, IL6, IL10 and TGFB1 gene polymorphisms in South and Southeast Brazil. Int J Immunogenet 35:287–293
Vu D, Tellez-Corrales E, Shah T, Hutchinson I, Min DI (2013) Influence of cyclooxygenase-2 (COX-2) gene promoter-1195 and allograft inflammatory factor-1 (AIF-1) polymorphisms on allograft outcome in Hispanic kidney transplant recipients. Hum Immunol 74:1386–1391
Wang Y, Wang YP, Zheng G, Lee VW, Ouyang L, Chang DH, Mahajan D, Coombs J, Wang YM, Alexander SI, Harris DC (2007) Ex vivo programmed macrophages ameliorate experimental chronic inflammatory renal disease. Kidney Int 72(3):290–299. https://doi.org/10.1038/sj.ki.5002275
Welfare AIOHA (2014) Projections of the prevalence of treated end-stage kidney disease in Australia, 2012–2020. In: Cat. No. PHE 176. AIHW, pp 1–51
Wei CL, Cheung W, Heng CK, Arty N, Chong SS, Lee BW, Puah KL, Yap HK (2005) Interleukin-13 genetic polymorphisms in Singapore Chinese children correlate with long-term outcome of minimal-change disease. Nephrol Dial Transpl 20(4):728–734. https://doi.org/10.1093/ndt/gfh648
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V (2000) Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 148(2):209–214. https://doi.org/10.1016/s0021-9150(99)00463-3
Acknowledgements
The authors were thankful to various central facilities such as Tissue Ty** Services, MKU and UGC, New Delhi, DST-WoSA New Delhi for financial support.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BK and RC conceptualized the idea, supervised the data collection and analysis, revised the manuscript critically for important intellectual content. VS and SP collected the data, analysed it. SK and DT supervised in the data collection. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The well-defined detailed questionnaire was obtained from each patient. Written informed consent was collected from all the participants and the study was approved by the Institutional Ethical Committee (Ref. No: version 04 MMHRC-IEC).
Consent for publication
Consent for the data publication was obtained.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sevak, V., Chinniah, R., Pandi, S. et al. Association of IL-4 (− 590 C/T) and IL-6 (− 174 G/C) gene polymorphism in South Indian CKD patients. Egypt J Med Hum Genet 25, 17 (2024). https://doi.org/10.1186/s43042-024-00476-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-024-00476-8