Abstract
Background
Lumbar spine injuries in fast bowlers account for the greatest missed playing time in cricket. A range of extrinsic and intrinsic variables are hypothesised to be associated with low back pain and lumbar spine injury in fast bowlers, and an improved understanding of intrinsic variables is necessary as these may alter load tolerance and injury risk associated with fast bowling. This review critically evaluated studies reporting intrinsic variables associated with low back pain and lumbar spine injury in fast bowlers and identified areas for future investigation.
Methods
OVID Medline, EMBASE, SPORTDiscus, CINAHL, Web of Science and SCOPUS databases were last searched on 3 June 2022 to identify studies investigating intrinsic variables associated with low back pain and lumbar spine injury in cricket fast bowlers. Terms relevant to cricket fast bowling, and intrinsic variables associated with lumbar spine injury and low back pain in fast bowlers were searched. 1,503 abstracts were screened, and 118 full‐text articles were appraised to determine whether they met inclusion criteria. Two authors independently screened search results and assessed risk of bias using a modified version of the Quality in Prognostic Studies tool.
Results
Twenty-five studies met the inclusion criteria. Overall, no included studies demonstrated a low risk of bias, two studies were identified as moderate risk, and twenty-three studies were identified as high risk. Conflicting results were reported amongst studies investigating associations of fast bowling kinematics and kinetics, trunk and lumbar anatomical features, anthropometric traits, age, and neuromuscular characteristics with low back pain and lumbar spine injury.
Conclusion
Inconsistencies in results may be related to differences in study design, injury definitions, participant characteristics, measurement parameters, and statistical analyses. Low back pain and lumbar spine injury occurrence in fast bowlers remain high, and this may be due to an absence of low bias studies that have informed recommendations for their prevention. Future research should employ clearly defined injury outcomes, analyse continuous datasets, utilise models that better represent lumbar kinematics and kinetics during fast bowling, and better quantify previous injury, lumbar anatomical features and lumbar maturation.
Trial registration
Open Science Framework https://doi.org/10.17605/OSF.IO/ERKZ2.
Key points
• No included studies were judged to have an overall low risk of bias.
• Inconsistencies in results of studies investigating associations between intrinsic variables and low back pain and lumbar spine injury may be due to differences in study design, injury definitions, participant characteristics, measurement parameters, and statistical analyses.
• Clearly defined injury outcomes, use of continuous datasets, models that better represent lumbar kinematics and kinetics during fast bowling, and improving the quantification of lumbar maturation, previous injury, and lumbar anatomical features represent areas for future research.
Similar content being viewed by others
Background
Although cricket is a non-contact sport, injury prevalence rates for fast bowlers have been reported to be as high as 20.6% [1] and exceed those reported in football (20%) [2] and rugby (12.0%) [3]. Injury rates of this magnitude may stem from the fast bowling action, which comprises a run-up and straight-arm hurling movement [4], resulting in extreme lumbar motions [5] and torques [6] in the presence of high ground reaction forces (GRF) [7]. These events are postulated to place the lumbar region of fast bowlers at a heightened risk of injury; reflected in high incidences of low back pain (LBP) [8, 9] and lumbar spine injury [1], often manifesting as lumbar intervertebral disc and pars interarticularis abnormalities [10]. Stress fractures of the lumbar spine represent 15% of all missed playing time in cricket [1], and up to 67% of fast bowlers will sustain this injury during their career [11]. Furthermore, stress fractures of the lumbar spine present potentially serious consequences for fast bowlers [11] as they generally cause many months of absence from cricket [12,13,14], and if not appropriately managed can result in chronic lesions characterised by non-union and recurrence [12, 13].
Multiple risk factors or variables are proposed to interact with one another to contribute to injury susceptibility in athletes [15], and a range of extrinsic and intrinsic variables are hypothesised to be associated with LBP and lumbar spine injury in fast bowlers [16]. Extrinsic variables include bowling workloads [4], match formats [1], and footwear [17]; whereas intrinsic variables may incorporate muscular strength and endurance [18], ranges of motion [18], previous injury [19], biomechanics of the fast bowling technique [5], age [20], and muscle activation [21], morphology [10] and morphometry [22]. Since intrinsic and extrinsic variables do not act in isolation, intrinsic variables may determine the level of risk predisposed [15] to a fast bowler, as elevated risk may cause subsequent exposure to fast bowling to become an inciting event associated with injury [15]. Identifying intrinsic variables is important because they can affect the load tolerance of tissues [23], and an improved understanding of their significance may contribute to the formation of a “cumulative risk profile” [24] for an individual fast bowler. This would represent a holistic assessment of the cumulative influence of intrinsic variables on injury risk with thoughtful consideration of their interaction with one another and with extrinsic variables [24], as this may determine a fast bowler’s capacity to withstand specific training and competition bowling loads, and influence planning and management of the same.
No prior systematic review has specifically reported on intrinsic risk factors associated with LBP and lumbar spine injury in fast bowlers. A narrative review conducted by Johnson et al. [11] reported that excessive shoulder counter rotation (SCR) in adolescents, and excessive contralateral lumbar side-flexion in adults were features of the fast bowling technique that were associated with an increased risk of develo** a lumbar stress fracture (LSF). A systematic review examining the association of intrinsic risk factors and successful interventions for LBP in all cricketers (batters, bowlers and wicketkeepers) by Morton et al. [25] identified acute bone stress on MRI scans as a risk factor for LBP and LSF in bowlers. Subsequent systematic reviews examined the association of extrinsic and intrinsic risk factors with all non-contact (lower limb, lumbar, trunk and upper limb) injuries in adult [16] and adolescent [26] fast bowlers. Olivier et al. [16] reported that bowling biomechanics, bowling workload, neuromuscular factors, and previous injury were risk factors for injury, whereas Forrest et al. [26] concluded that injury was associated with bowling biomechanics (excessive lateral trunk flexion and pelvis/hip kinematics), reduced trunk endurance, poor lumbo-pelvic-hip movement control, and early signs of lumbar bone stress on MRI.
The above mentioned systematic reviews [16, 25, 26] presented risk of bias assessments as summary numerical scores using the Downs and Black tool [25], the Joanna Briggs Institute Meta Analysis of Statistics Assessment and Review Instrument [16], and the Newcastle–Ottawa Quality Assessment Scale [26]. The Cochrane Risk of Bias Tool recommends when assessing the risk of bias in studies, it is advisable to select a tool that does not present assessments as summary numerical scores [27], as these have been demonstrated to be poor indicators of study quality [28]. The use of a tool that facilitates a structured assessment, is not based on a scoring system, and is easily adapted for specific needs, is advisable when assessing a study’s risk of bias [28]. Furthermore, previous systematic reviews [16, 25, 26] have not provided detailed information regarding risk of bias evaluations for individual studies, and it has been recommended that researchers should provide supporting statements to justify how risk of bias judgements were reached to minimise subjectivity and maximise consistency of interpretation [29].
The relationship between lumbar spine pathology, missed playing time and LBP in fast bowlers is not straightforward [30], and this is illustrated by asymptomatic fast bowlers presenting with MRI detected pathology [31] as well as high incidences of adolescent fast bowlers presenting with LBP not causing an absence from bowling [9]. Notwithstanding this, lumbar bone stress injuries (LBSI) have been long recognised as a common cause of LBP in fast bowlers [8], and young fast bowlers presenting with LBP contralateral to their bowling arm side represent a high yield population for which an MRI scan provides value for the diagnosis of LBSI [12]. To better understand biases and evidence in the previous literature, it is necessary to examine intrinsic variables that have been associated in studies reporting both LBP and lumbar spine injury, regardless of the presence or absence of symptoms, radiological findings and missed playing time.
Despite extensive research and resources dedicated to identifying intrinsic and extrinsic variables as independent markers for risk of develo** LBP and lumbar spine injury in fast bowlers, there has been limited success in predicting and preventing these issues [1]. Whether this lack of predictive insight is related to yet to be identified independent variables, heterogeneity of participant populations [16] or diversity of research methodologies [30] requires further exploration. For example, a recent systematic review reported minimal strength in reported associations between lower back injury and fast bowling workload metrics due to biases within injury and workload measurements in the existent literature [32]. Furthermore, the use of causal inference to classify markers of risk as causal or non-causal may be required, since interventions to prevent injury should be targeted at established causal associations [33].
Given the burden and potential long-term consequences of LBP and LSF in fast bowlers, it is important to better investigate strategies to reduce their incidence [11], and the identified gap in the literature provides an opportunity to conduct a more robust appraisal of intrinsic variables associated with these entities in fast bowlers. The purpose of this review was to critically evaluate studies reporting intrinsic variables that have been associated with LBP and lumbar spine injury in fast bowlers. A further aim was to identify areas for future investigation to assist in the development of effective strategies for the prevention of LBP and lumbar spine injury in fast bowlers.
Methods
This systematic review was specified a priori through protocol registration with the Open Science Framework (https://doi.org/10.17605/OSF.IO/ERKZ2, 30 July 2020), and was developed and reported in accordance with the PRISMA-P guidelines for Systematic Reviews [34].
Data sources and search strategy
For the purposes of data extraction, aspects of a modified PICOC (Population, Intervention, Comparison, Outcome, and Context) framework were applied. Studies evaluating intrinsic variables as risk factors (Intervention) in the development of pain and injuries (Outcome) to the lumbar spine (Context) in cricket fast bowlers (Population) were systematically identified, and the search algorithm was derived from this PICOC framework. Studies published in English or with an available English translation from inception to 27 July 2020 were considered for inclusion into this systematic review. OVID Medline, EMBASE, SPORTDiscus, CINAHL, Web of Science and SCOPUS databases were searched, and the following Boolean search strings were used: (“Cricket” OR “Fast Bowling” OR “Fast Bowler”) AND (“Risk Factor*” OR “Risk” OR “Factor*” OR “Variable” OR “Intrinsic” OR “Age” OR “Adolescent” OR “Young” OR “Adult” OR “Technique” OR “Biomechanic*” OR “Kinematic*” OR “Kinetic*” OR “Strength” OR “Flexibility” OR “Range of motion” OR “Muscle” OR “Asymmetry” OR “Cross Sectional Area” OR “Volume”) AND (“Pain” OR “Injury” OR “Fracture” OR “Stress” OR “Stress Fracture” OR “Stress Reaction” OR “Reaction” OR “Pars interarticularis” OR “Pars” OR “Pedicle” OR “Spondylolysis” OR “Spondylolisthesis” OR “Bone” OR “Oedema” OR “Edema”) AND ( “Low Back” OR “Back” OR “Lumbar” OR “Lumbar Spine”). A detailed search strategy for each database is included in Additional file 1 and this search was repeated on 21 September 2021 and 3 June 2022 to identify new literature. The reference lists of previous systematic reviews were examined to ensure that all potentially relative articles were located, and additional studies were extracted via manual searches of bibliographies, relevant journals, and websites.
Eligibility criteria
The following criteria were employed to determine the eligibility of literature for inclusion in this review:
Types of studies
A range of peer-reviewed journal articles that investigated intrinsic variables associated with the incidence of LBP and lumbar spine injury during fast bowling in cricket were eligible for inclusion. This incorporated both observational (prospective cohort, retrospective cohort, case control, cross-sectional, case series) and interventional (randomised controlled trial, non-randomised controlled trial, quasi-experimental) study designs.
Types of participants
Studies included male and female fast bowlers of all age groups and playing levels as participants. A fast bowler was defined as a bowler with a fast run-up, with ball release (BR) speed generally above 100 kph and a wicketkeeper generally standing back from the stumps due to increased BR speed [4].
Types of outcome measures
Outcome measures included any lumbar spine condition that resulted in the loss of at least one day of sporting activity, a match time loss injury [1], abnormal radiological features of the lumbar spine, LBSI or LSF, LBP experienced at time of testing or during a study period, a history of LBP, a history of lumbar spine injury, a history of LBSI or a history of LSF.
Types of intrinsic variables
Intrinsic variables associated with LBP and lumbar spine injury during fast bowling in cricket that included, but were not limited to, participants’ age, previous injury or pain, biomechanics of the fast bowling technique, muscle strength and endurance, ranges of motion, posture, anthropometric measures, proprioception, bone marrow oedema (BMO) detected on Magnetic Resonance Imaging (MRI), bone mineral density (BMD), bone mineral content (BMC), spinal and trunk muscle thickness, cross sectional area (CSA) and volume.
Study selection
All studies identified through search strategies were uploaded into Covidence software [35] and following this, two authors (PF and DB) independently and blindly screened study titles and abstracts to determine their eligibility for inclusion in full text screening. Narrative reviews, systematic reviews, meta-analyses, opinion pieces, non-peer-reviewed articles, conference proceedings, and articles with full-text unavailable were excluded. The full text of eligible studies was then blindly evaluated in an independent manner by the same authors to determine inclusion into the main body of the review. Any disagreements regarding article inclusion were resolved independently by a third author (MW).
Data extraction
Data from included studies was extracted by two reviewers (PF and DB) using a modified template based on the Checklist for critical Appraisal and data extraction for systematic Reviews of prediction Modelling Studies (CHARMS) [36]. Extracted data included authors, design, study inference, location, duration, dates, participant information (number, playing level, age, gender, presence of control group), investigated variables, injury outcome, and reported results. Disagreements were resolved through discussion, and if consensus could not be reached, the third reviewer (MW) was consulted.
Risk of bias assessment
The methods of risk of bias assessment for included studies were changed from the review protocol registered on the Open Science Framework. Risk of bias was assessed using a version of the Quality in Prognostic Studies (QUIPS) tool [37] modified for this review. QUIPS considers the following six domains to assess potential risk of bias: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting [37]. Each bias domain contained prompting and consideration items assessed with the terms ‘yes’, ‘partial’, ‘no’ or ‘not reported’; and methodological comments supporting each item’s assessment were recorded. Additional file 2 details defined criteria for the rating of studies. Since responses to individual items may balance or override others, item responses were considered together to assess the risk of bias of each domain, and each domain was rated as having a high, moderate, or low risk of bias.
In line with the Cochrane Risk of Bias Tool for intervention studies [27] and the QUADAS-2 Tool for diagnostic studies [38], computing summated scores for overall study quality using QUIPS is not recommended [27], and this approach was used for this review. Overall study risk of bias was determined as follows: 1) If all domains were low risk, or if one domain was no higher than moderate risk, then a study was classified as low risk, 2) If one or more domains were high risk, or if ≥ 3 domains were moderate risk, then a study was classified as high risk, 3) All studies in between were classified as moderate risk [39]. Two reviewers (PF and DB) assessed risk of bias independently, but were not blinded to authors, title, or journal, and a Quadratic Weighted Kappa score [40] was calculated to determine the level of agreement of individual risk of bias domain judgements between the two reviewers. Disagreements were resolved through discussion, and if consensus could not be reached, the third reviewer (MW) was consulted.
Results
Study selection
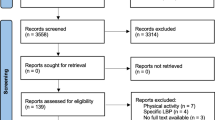
As depicted in Fig. 1, database searching generated 2109 studies, and a further 15 were identified following manual searching. 1503 studies remained after duplicates were removed, and 1385 were deemed irrelevant during the title/abstract screening process. Of the 118 studies retained for full text evaluation, 93 were excluded, leaving 25 studies [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] for inclusion into this review.
Risk of bias of studies
The results of risk of bias assessments for each of the six QUIPS domains are presented in Table 1, and Additional file 3 contains detailed information regarding these evaluations. The study screening reviewers (PF and DB) agreed on 124 of 150 items prior to consensus, resulting in a Quadratic Weighted Kappa [54] of 0.84 (95% CI 0.75–0.92). Agreement on domains ranged from 76% (prognostic factor measurement) to 88% (study participation and study confounding). No included studies were categorised as having an overall low risk of bias, two were moderate risk [51, 63], and twenty-three were high risk [41,42,43,44,45,46,47,48,49,50, 52,53,54,55,56,57,58,59,60,61,62, 64, 65]. Figure 2 depicts a summary of judgements for each domain’s risk of bias as percentages. Potential sources of bias (moderate risk %, high risk %) were classified as study participation (72%, 28%), study attrition (36%, 16%), prognostic factor measurement (24%, 52%), outcome measurement (36%, 28%), study confounding (32%, 40%), and statistical analysis and reporting (40%, 20%).
Study characteristics
General
Extracted data from included studies [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] is presented in Table 2. Studies consisted of thirteen prospective cohort [41,42,43,44,45,46,47,48,49,50,51,52,53], five cross-sectional [54,55,56, 62, 63], three retrospective cohort [57,58,59], two combined retrospective/prospective cohort [60, 61], retrospective case series [64], and interventional [65] designs. Prospective research was conducted over one cricket season [42, 46,47,48,49,50, 52, 61] or multiple years [41, 44, 45, 51, 53, 60, 65]. Sixteen studies were conducted in Australia [42,43,44, 46, 47, 49, 52, 54,55,56,57,58,59,60, 64, 65], six in the United Kingdom [41, 45, 51, 53, 61, 63] and three in South Africa [48, 50, 62]. Dates of data collection ranging from 1986 [42] through to 2020 [59] were reported in twelve studies [42, 43, 45, 46, 51, 52, 54, 56, 59,60,61, 65]. A causal association between investigated variables and LBP and lumbar spine injury was implied in twenty-one studies [41,42,43, 45, 48,49,50,51,52,53,54,55,56, 58,59,60,61,62,63,64,65].
Participants
Mean chronological age was reported in all studies [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65], ranging from 13.2 [65] to 24.9 years [51], and four studies included age-matched control groups [44, 51, 55, 64]. Only two studies did not contain exclusively male participants, with one including females only [58] and another females and males [57]. Studies recruited elite level adults [45, 47, 51, 53, 57, 58, 60, 61, 63, 64], elite level adolescents [46, 54, 55, 59, 61, 62, 65], club and/or school level adolescents [42, 43, 46, 56], adolescents at varying skill levels [41, 44, 49], and club level adults [48, 50]. At commencement of seventeen studies [41,42,43,44,45,46,47,48,49,50, 52,53,54, 56, 61, 64, 65], bowlers were deemed fit to bowl and had no knowledge of abnormal radiological features, but may have experienced LBP in two of these [43, 56]. Six studies [55, 57, 58, 60, 62, 63] included bowlers with and without injury outcomes at commencement, and two studies [51, 59] exhibited incomplete disclosure of injury status at commencement.
Injury outcomes
Eleven studies [42, 44,45,46,47, 51, 52, 59, 60, 63, 64] reported injury if a combination of lumbar symptoms, abnormal radiology and missed playing time were present. LBSI was defined across studies [46, 47, 52, 59, 64] as an MRI confirmed stress reaction (BMO with no cortical breach) or stress fracture (BMO with cortical breach) [52]. LSF [42, 45, 51, 60, 63] and pars interarticularis lesions [44] were reported as partial or complete fractures [45], or with no description of cortical breach presence [42, 44, 51, 60, 63]. Soft tissue injuries [42, 46, 47, 60] were reported without elucidation [42], or defined as disc, muscle, or ligament injury [46], injuries other than bone stress [47], or categorised as back sprain (disc, facet joint or ligament) injuries [60]. Six studies described LBP in the absence of radiology findings as an injury outcome [48, 50, 57, 58, 61, 62]; derived from questionnaires investigating previous LBP occurrence [48, 50, 61, 62], self-reported LBP in the previous 12 months [57, 58], recording of LBP during a study [48, 50, 61], or self-reported LBP verified by medical records [57, 58].
Studies describing injury in the absence of symptoms [43, 53,54,55,56, 65] reported LBSI determined from MRI reports [53], disc degeneration determined by MRI features [43, 54,55,56, 65], and Computed Tomography (CT) diagnosed bone abnormalities categorised as spondylolysis, spondylolisthesis, or pedicle sclerosis [54, 55]. Two studies [41, 49] categorised injury in bowlers with and without symptoms; with one defining injury as LBP affecting a bowler’s ability to perform in a match and expanded this to include asymptomatic bowlers with MRI detected lumbar bone stress [49]. Subsequent research categorised injury as symptomatic LBSI causing missed playing time as well as MRI reported LBSI in asymptomatic bowlers [41].
Intrinsic variables measured
A summary of intrinsic variables reported in included studies is contained in Table 3 and definitions for these variables are contained in Additional file 4. Twelve studies investigated bowling technique biomechanical variables [42, 43, 49, 53,54,55,56, 58,59,60,61, 65] utilising two-dimensional (2-D) motion analysis [42, 43, 54,55,56, 65], three-dimensional (3-D) motion analysis [49, 53, 58, 60], both 2-D and 3-D motion analysis [59], and inertial measurement units (IMUs) [61]. Four studies assessed trunk kinematics [55, 58, 59, 61]; whereas eight measured both trunk and lower limb kinematics[42, 43, 49, 53, 54, 56, 60, 65]. Seven studies quantified kinetics [42, 49, 53, 54, 56, 60, 61]; six measured GRF with force plates/platforms [42, 49, 53, 54, 56, 60], and IMUs captured sacral and tibial rates of loading and impacts in another [61]. Biomechanical testing environments were laboratory based [42, 43, 53, 54, 56, 58, 60, 65], outdoors [61], laboratory and netted [59], and not specified in two studies [43, 55]. Discrete point analysis techniques were used to identify kinematic and kinetic variables in all biomechanical studies [42, 43, 49, 53,54,55,56, 58,59,60,61, 65]. Descriptive variables collected included BR height [42, 54, 56], BR speed [53, 54, 56, 59], approach velocity [42, 49, 53, 54], delivery stride length [54, 56], and delivery stride alignment [54].
Ten studies applied radiological investigations to assess trunk and lumbar anatomical characteristics [41, 44,45,46,47, 50, 52, 62,63,64]. MRI was used to quantify Quadratus Lumborum (QL) muscle asymmetry [44, 46, 47], whereas Ultrasound (US) was employed to measure Multifidus CSA [50] as well as Transversus Abdominis, Internal Oblique and External Oblique thickness [62]. Three studies utilised MRI to investigate BMO presence in lumbar vertebrae and its association with future injury [45, 52, 64], and one examined lumbar intervertebral disc degeneration for this purpose [45]. Dual Energy X-ray Absorptiometry (DEXA) was used to assess lumbar spine BMC and BMD [41, 63], vertebral body area [41], and skeletal age was assessed with DEXA of the left hand [41] and analysed by the Tanner and Whitehouse Three method [66]. Chronological age [41, 51, 54, 59] and a history of LBP or lumbar injury [48, 50, 61] were investigated as variables that may be associated with future LBP and lumbar spine injury.
Strength measures included testing of maximal trunk flexion and extension strength [42, 54], maximal hip abduction and extension strength [59], isokinetic hamstring and quadriceps muscle strength [42], calf muscle and single leg bridge capacity [49], and shoulder depression/horizontal flexion strength [42]. Abdominal muscular function was assessed with prone and side plank tests [49], and a 60 s sit up test [42, 54, 56], whereas trunk extensor endurance was assessed with the Biering-Sorensen test [49, 57, 59].
Range of motion assessments included sit-and-reach [41, 42, 54], shoulder flexibility [42], lumbar flexion [57], extension [57], and lateral flexion in standing [57, 59], passive straight leg raise [41, 57], modified Thomas test for hip extension [57], hip external and internal rotation [41, 49, 59], bent knee fall-out for hip flexibility [41], and ankle dorsiflexion with lunge testing [41, 49, 59]. Physical characteristics including skinfold levels [42, 54, 56], foot arch features [42, 49, 54], body mass [42, 54, 56, 59], fat free mass [41], body mass index (BMI) [46, 47], segment anthropometrics [42], posture [42, 54], standing height [41, 59], and aerobic capacity [42, 59] were assessed. Lumbar Reposition Error (LRE) in neutral spine and fast bowling specific positions [48], a single leg decline squat test [49], a lumbopelvic stability test [49, 59], and a Star Excursion Balance Test (SEBT) [59] were employed as neuromuscular control assessments.
Results of individual studies
Age
Prospective research reported an association between LSF and younger chronological age in professional fast bowlers (mean age 24.87); as 74% of LSFs occurred in bowlers aged under 25 years, with an annual incidence of 4.90 LSFs per 100 bowlers aged 18 to 22 compared to 2.46 across the entire cohort [51]. A range of associations between age and injury have been reported in adolescent cohorts [41, 54, 59]; as LBSI risk was 2.99 times higher for each year younger in bowlers aged 15 to 20 years [59], and bowlers with LBSI were older than injury free bowlers (median 18.4 vs 16.4 years) [54], whilst injured bowlers were 1.3 years older than uninjured bowlers, despite no difference in average skeletal age or maturation [41].
Previous lumbar injury
No associations were reported between incidence of previous and future lumbar injury in two studies [48, 50]. However, previous LBP is potentially a good prognostic indicator for recurrent injury, as all bowlers who developed LBP during a prospective study reported previous LBP at study commencement [61].
BMC/BMD
Non-significant associations were reported in two studies investigating relationships between lumbar BMD and injury [41, 63]. In a cross-sectional study, adult bowlers with previous LSF had 3.6% and 1.7% lower BMD in dominant and non-dominant sides of lumbar vertebrae respectively compared to bowlers without LSF history [63]. In contrast, prospective research reported greater non-dominant side BMD of the L3 and L4 vertebrae by way of larger effect sizes in adolescents who developed LBSI [41].
Trunk and lumbar muscle morphology and morphometry
Asymmetries presenting as increased QL volume on the bowling arm side have been associated with symptomatic L4 pars lesion development [44] in adolescents. However, subsequent research reported no significant association between QL CSA asymmetry and future LBSI in adolescents [46] and adults [47].
Whilst Multifidus CSA on the contralateral side to the bowling arm at L3 and L5 was reported to be smaller in adults who developed a lumbar injury, no associations were reported for between-sides percentage differences or asymmetry [50]. The individual and total combined thicknesses of three abdominal muscles (Transversus Abdominus, Internal Oblique, External Oblique) on the side opposite to the bowling arm were reported to be greater in pain-free adolescents compared to those experiencing LBP [62].
Presence of BMO
In elite bowlers, BMO at baseline MRI was associated with symptomatic LSF development at a mean of 10 weeks from scan time [45], and bowlers with cortical breach at baseline developed symptoms within 4 weeks, compared to a mean of 11 weeks for those with no cortical breach [45]. In adolescents who underwent six MRI scans throughout an eight-month cricket season, all participants who sustained a symptomatic LBSI had corresponding site BMO detected in the scan immediately prior to diagnosis, with a mean of 96 days between initial BMO appearance and symptom reporting [52]. When results of all scans were pooled, a relative risk of 22.3 (95% CI 1.4 to 256.6) was reported for detected BMO leading to a symptomatic LBSI; with a Positive Predictive Value of 39.5 and a Negative Predictive Value of 100 [52]. Elite bowlers nominated for screening by their medical team with a BMO intensity ratio of ≥ 2.0 on MRI were reportedly at 1.8 times greater risk of sustaining LBSI in the following 12 months compared to bowlers with no abnormal BMO detected; with a median of 258 days between scan time and injury diagnosis [64].
Biomechanics of fast bowling
Biomechanical studies were prospective [42, 43, 49, 53], cross-sectional [54,55,56], retrospective [58, 59], combined prospective/retrospective [60, 61], and interventional [65] in nature. In predominantly adolescent fast bowlers, greater BR height was associated with lower back injuries [42] and lumbar bone abnormalities [54], but not disc degeneration [56]. The association of BR speed and lumbar spine injury is inconsistent, as studies in adults [53] and adolescents [54, 56] reported no associations, whereas subsequent research reported LBSI risk increasing 1.1 times for every km/h faster BR speed in adolescents [59].
Reported associations between shoulder alignment and lumbar spine injury are inconsistent. A front-on shoulder alignment at back foot contact (BFC) has been associated with LSF in adults [60], and with LSF [54], lumbar disc [54] and lower back [42] injuries in adolescents. Interestingly, other studies have reported no association with disc degeneration in adolescents [56] or lower back injury in adolescent [49, 61] or adult [53, 61] bowlers.
A front-on shoulder alignment at BFC has been linked to increased SCR, which is the change between shoulder alignment at BFC and the minimum shoulder alignment during the delivery stride [60], however, the association of SCR with lumbar spine injury is inconsistent. SCR has been associated with LSF [42], disc abnormalities [56, 65], and radiological abnormalities [54] in adolescents, and LSF in adults [60]. Subsequent studies however reported no association between SCR and LBP history in elite females [58], adolescents and adults [61]; or future lumbar spine injury in adolescent [49, 59, 61] and adult cohorts [53, 61].
In adults, associations between increased hip counter rotation and hip-shoulder separation (HSS) at BFC with LSF and back sprain injury respectively were reported; and a large HSS angle at BFC along with high SCR define a mixed technique [60]. Higher rates of radiological abnormalities [54], disc degeneration [43, 56, 65], and LBP [55] in adolescents, and lower back injuries in adults [60] have been associated with a mixed technique. However, other studies reported no such associations with LBP history in elite females [58] or lumbar spine injury in adolescent [49, 59, 61] or adult fast bowlers [53, 61].
Conflicting results have been reported for associations between lateral flexion away from the bowling arm and lumbar spine injury [49, 53, 58, 59, 61]. Thorax lateral flexion was greater during the delivery stride in elite females with LBP history [58], and at front foot contact (FFC) and BR in adolescents who developed lumbar spine injury [49]. Injured elite males had less thoracolumbar lateral flexion at BFC and BR, and a medium effect size for increased lumbopelvic lateral flexion at BR [53]; whilst no association was reported for lumbopelvic lateral flexion range between FFC and BR and injury elsewhere [49]. Further to this, large effect sizes have been reported for increased lumbar lateral flexion at BFC in adults who did not develop LBP [61], and a recent 2-D study demonstrated no relationship between trunk lateral flexion and LBSI in adolescents [59].
Thorax flexion and extension relative to the pelvis did not have any association with LBP history in elite females [58]. Lumbopelvic flexion/extension has an inconsistent relationship with injury; as this was not associated with lower back injury in adolescents [49], but in adults each 1° increment in the lumbopelvic extension angle at FFC increased the odds of LBSI by 1.25 [53]. Furthermore, large effect sizes have been reported for greater thoracolumbar extension at BFC in adults with LBP history [61], and for reduced lumbar extension at BFC and FFC in adults who did not develop LBP [61].
Associations between LBP and lumbar spine injury and rotation metrics are inconsistent [49, 53, 58, 61]. Neither thorax rotation relative to the pelvis [58] or lumbopelvic rotational range [49] were associated with LBP history in elite females [58] or lower back injury in adolescents [49]. However, subsequent research reported that injured adults had increased thoracolumbar rotation away from the bowling arm at the instance of BFC [53]. In adolescents without LBP history, large effect sizes were reported for increased thoracic rotation away from the bowling arm at BFC and an increased range of thoracic rotation between BFC and FFC [61]. In the same study, a large effect size for reduced lumbar rotation at FFC was observed in adults who did not develop LBP [61].
Pelvis-shoulder separation at BFC had no association with LBP history in elite females [58] or LBSI in adults [53]. Increased pelvis rotation beyond front-on at BR was reported in adolescents who developed lower back injury [49] and increased anterior pelvic tilt at FFC and increased ipsilateral pelvic drop in transitions between BFC and BR were reported in adults who sustained LBSI [53].
Injured adults were reported to have more flexed rear hip and knee angles at the instance of BFC, and the degree of rear hip flexion was reported to categorise LBSI in 76% of bowlers, with odds of injury reduced by a factor of 0.88 for each 1° increment in rear hip extension [53]. Reduced front hip flexion during FFC has been associated with LSF [42] and lower back injury [49] in adolescents, and LSF in adults [60]. Conversely, adults with LBSI were reported to have more flexed front hip angles at FFC and possess less front hip extension in transitions between BFC and BR [53].
The relevance of front knee angles to injury [42, 49, 53, 56, 60, 65] has also yielded conflicting results. Whilst predominantly adolescent bowlers who developed LSF tended to have increased front knee extension [42], and non-injured adults displayed increased front knee flexion during FFC [60], other studies have reported no association of front knee flexion during FFC and at BR with lumbar spine injury in adolescents [49, 56, 65] and adults [53]. No associations were reported in adults between LBSI and front foot and front leg plant angles at the instant of FFC [53].
GRF magnitudes at BFC and FFC have not been significantly associated with lumbar spine injury [42, 49, 53, 54, 56, 60]; however, adults who experienced LSF displayed tendencies for higher vertical GRF at BFC, and faster rates of peak braking and vertical force development during FFC [60]. Large effect sizes were reported for reduced peak tibial Z axis acceleration and faster time to peak resultant tibial acceleration at FFC in adults with LBP history [61], whereas those who did not develop LBP experienced higher time to peak resultant tibial acceleration at BFC and higher tibial loading variables at FFC [61]. Large effect sizes were reported for greater time-to-peak vertical and resultant acceleration at the sacrum in adults who developed LBP [61]. Injured adolescents displayed increased peak lateral flexion power and normalised peak flexion and lateral flexion lumbar moments in comparison to non-injured counterparts [49].
Physical characteristics
Whilst an association was reported in adolescents between lower longitudinal foot arch height and LSF [42], other research reported no such relationship with lower back injury [49] or radiological abnormalities [54]. An association between higher BMI and LBSI was reported in adolescents [46], but not in adults [47]; and adolescents were reportedly 1.1 times more likely to sustain LBSI for every centimetre taller in standing height [59].
Range of motion assessments have yielded conflicting results, with sit and reach scores being lower in adolescents with intervertebral disc abnormalities [54], but not in those with disc degeneration [56] or LBSI [41]. Elite females with LBP history had reduced lumbar lateral flexion range to the bowling arm side [57]; however, lumbar lateral flexion range was not associated with LBSI in in adolescent males [59]. Hip internal rotation of the non-dominant leg was reported to be 7.2° less in adolescents who sustained an LBSI, however this was not statistically significant [41].
Analyses of muscle strength and endurance have reported varying associations with lumbar spine injury incidence [42, 49, 54, 56, 57, 59]. Greater front leg quadriceps and bowling arm shoulder depression and horizontal flexion strength have been reported in predominantly adolescent bowlers with LSF and lumbar injuries respectively [42]. Whilst reduced trunk extensor endurance was reported in adolescents who developed lower back injury [49]; other research reported no association between this and LBP history in elite females [57], or LBSI in adolescents [59].
Reduced performance of the lumbopelvic stability test in adolescents was reported to be associated with a 1.7 times increased risk of lower back injury in one study [49], but not related to LBSI in another [59]. In adolescents, increased knee valgus angle during a single leg decline squat on both legs was reportedly associated with increased lower back injury risk [49]. Whilst SEBT distance was deemed not to be significant in multivariate analysis, adolescents who sustained LBSI performed less efficiently on this test [59]. LRE in two neutral spine and six fast bowling specific positions was associated with LBP history, and LRE in two neutral positions was associated with a future lower back injury [48].
Discussion
This systematic review reported on intrinsic factors associated with LBP and lumbar spine injury in fast bowlers. Conflicting results were reported amongst studies investigating fast bowling biomechanics [42, 43, 49, 53,54,55,56, 58,59,60,61, 65], trunk and lumbar muscle asymmetries [44, 46, 47, 50, 62], anthropometric characteristics [42, 46, 47, 49, 54, 56, 59], muscle strength and endurance [42, 54, 56, 57, 59, 63], ranges of motion [41, 42, 49, 54, 57, 59], neuromuscular control [48, 49, 59], age [41, 51, 54, 59], and lumbar BMD [41, 63]; whereas more consistent results were described when reporting lumbar vertebra BMO and its association with subsequent LBSI [45, 52, 64]. Inconsistencies in results may reflect differences in study design, injury definitions, participant characteristics, measurement parameters, and statistical analyses.
Risk of bias
Risk of bias appraisal is essential as increased bias affects the internal validity of studies [37, 67] that may inform strategies for injury prevention in fast bowlers. Aspects of bias relating to assessed QUIPS domains and how these inform directions for future research will be discussed herein, particularly given the high overall risk of bias in many studies evident in Fig. 2.
Participation bias
Eighteen studies [41, 43, 44, 46, 48,49,50,51,52,53,54,55,56, 59, 60, 62, 63, 65] were classified as having a moderate risk of participation bias, and the remaining seven [42, 45, 47, 57, 58, 61, 64] were rated as high risk. Studies with the lowest sample sizes [43, 45, 47,48,49,50, 54,55,56,57,58, 62, 63] may have been inadequately powered [68], and this possibly contributed to the low replicability of results from included studies. The non-reporting of recruitment methodologies [44, 46, 49, 62, 63] and response rates to recruitment [48, 50] may reflect an absence of eligible participants and reduced study representativeness. Volunteer bias [67] may have occurred in studies that recruited higher proportions of injured participants [53, 62] and in research not reporting injury history, which was described in only four included studies [44, 48, 50, 61]. Selection bias [67] may have occurred in studies exhibiting targeted recruitment of participants by coaches [42, 45, 57, 58, 61], selectors [47], and medical staff [64], and in another excluding 15 asymptomatic bowlers at study commencement due to MRI findings [49]. Survivor bias may have existed in professional cohorts [47, 51, 57, 58, 60, 63], as previously injured bowlers may have become slow bowlers, specialist batters, or no longer be playing cricket at the elite level [57].
The transparent reporting of recruitment across adolescent, adult, amateur and professional fast bowling cohorts is an important first step in reducing participation bias. Multifaceted recruitment methods incorporating personal contact, social media initiatives, and partnerships with stakeholders based on education and dissemination of research results will improve power and representativeness of future research [68], and subsequent random selection of participants from pre-established cohorts can reduce volunteer bias [69]. Sample size calculations were conducted for only one included study [61], and these should be considered in future studies incorporating accuracy in parameter estimation, sequential testing, and Bayesian models, as these approaches may improve the precision of measurements and detection of small effects [70]. Moreover, the establishment of international collaborations to acquire datasets of sufficient sample size and heterogeneity may improve the external validity of future research [71].
Attrition bias
Apart from lowering study power, attrition threatens both external and internal validity of results [72], as participants who are most impaired are more likely to be lost to follow-up [73]. A moderate risk of attrition bias was judged to be present in the following study designs that did not report participants potentially lost to follow-up; prospective with one cricket season length [42, 46,47,48, 50], prospective in elite environments over multiple seasons [45, 53], and combined retrospective/prospective [60, 61]. Prospective research not reporting dropouts in non-elite environments over multiple years [43, 65] was classified as high risk, as was a study not describing reasons for six participants missing from initial recruitment [49], and another with a reported dropout rate of 45% [41].
Reducing attrition using matching retention strategies to samples prior to study implementation, including careful consideration of unintended burden for participants [74] is required in future prospective research. In studies where attrition has occurred, bias can be reduced with reporting of sample size at each data collection point, reasons associated with loss of participants, and statistical analysis of dropouts versus those remaining across demographic data, pre-test responses, and variables particular to studies [72].
Prognostic factor measurement bias
Six studies [48, 50, 52, 58, 61, 63] were classified as having a moderate risk of prognostic factor measurement bias, and thirteen were rated as high risk [42,43,44, 46, 47, 53,54,55,56, 59, 60, 64, 65]. The use of single trials [42, 43, 48, 53,54,55,56, 60, 65] to assess fast bowling biomechanics was judged to increase risk of bias, as too few trials may not appropriately represent long-term technique [75], and individual movement patterns and movement variability associated with fast bowling technique fluctuate within bowling sessions [76]. Increased bias was judged when MRI assessments were scheduled at a time to allow bowlers further recovery [64], and when injuries pooled for analysis were sustained prior to and following biomechanical testing [60], as the assumption of similar bowling technique before and after injury is tenuous.
The dichotomising of continuous variables into discrete categories using arbitrarily chosen or data driven thresholds [71] was judged to increase risk of bias [42,43,44, 46, 47, 50, 54, 55, 58,59,60, 65]; as this practice discards information, reduces statistical power, and is biologically implausible [77] through its assumption that all participants within a category possess equal risk of injury [78]. Studies not referencing the reliability of measurements were adjudged to possess increased bias risk [42, 43, 53,54,55,56, 59,60,61, 65], and whilst two studies understandably employed a multicentre approach for MRI [52, 64], inter-rater reliability for BMO detection in one of these [52] was reported as “moderate” in subsequent research [79]. Studies investigating associations between QL asymmetry and injury that could access images across limited vertebral levels [44, 46, 47] were deemed prone to increased bias risk, as was a study that reported bowling technique biomechanical variables for only 68% of recruited participants [59].
The highlighting of these potential biases can guide future researchers and approaches that include quantifying the number of fast bowling trials to provide a stable estimate of key performance and biomechanical variables, standardising protocols to improve inter-rater detection of radiological abnormalities, and accounting for previous injury in study designs and analyses. Furthermore, continuous variables should remain continuous and be modelled appropriately [71], and the validity and reliability of employed measurement tools should be established to limit misclassification bias [67].
Outcome measurement bias
Nine studies [44, 48, 56,57,58, 60, 61, 63, 65] were classified as having a moderate risk of outcome measurement bias, and seven [41,42,43, 49, 53,54,55] were rated as high risk. Increased bias was adjudged when methodologies or reliability associated with LBP and lumbar spine injury outcomes were not reported [42,43,44, 53,54,55,56, 65]. Potential recall bias may have caused under-reporting of injury incidence in studies relying on retrospective data sourced from participants [48, 60, 61], or from medical records [57, 58, 63]. Cross-sectional [55, 56, 62, 63], retrospective [45, 54, 57,58,59, 61, 64], and prospective studies with one cricket season follow up [42, 46,47,48,49,50, 52, 61] were deemed to exhibit increased bias due to missing, adverse, or otherwise injury outcomes that may have occurred over a prolonged period of observation [80].
Studies that employed CT to investigate LSF presence [42, 54, 55] are prone to misclassification bias [67, 81], as CT possesses reduced sensitivity in diagnosing stress reactions [81]. Research categorising injury on radiological findings alone [43, 53,54,55,56, 65] or studies including both asymptomatic bowlers with abnormal radiology and bowlers with symptoms [41, 49] were considered to display increased risk of bias. Reported dissociations between lumbar symptoms and MRI [31, 52] and CT [82] detected abnormalities support this judgement, as a proportion of fast bowlers with radiological abnormalities will not experience symptomatic injuries and missed playing time [31, 52, 82].
Multiple injury definitions within and between studies confound the relevance of investigated variables [37], and future studies should employ injury definitions that encompass symptoms, clinical signs, and imaging findings, as these may better represent injury burdens in fast bowling cohorts. The creation of a multidisciplinary consensus for LBP and lumbar spine injury diagnosis in fast bowlers may be an important step in improving the external validity of future research.
Confounding bias
Future studies investigating causality should carefully consider the concept of confounding bias, as injury is the result of a complex interplay between tissue loading and a range of modifiable and non-modifiable physiological factors including tissue specific mechanical properties and adaptations that affect tissue resilience [15, 83]. Studies implying causality that did not account for confounders [43, 45, 50, 53, 55, 58, 60,61,62, 65] were rated as having a high risk of confounding bias; whereas those that accounted for a limited number of confounders [48, 51, 52, 63, 64] or measured confounders and did not account for them in a multivariate analysis [42, 54, 56] were rated as moderate risk. Reportedly significant associations in these studies may have been distorted by confounders that were related to an investigated variable as well as LBP or lumbar spine injury.
Future projects should incorporate directed acyclic graphs (DAGs), as these can illustrate confounders to include and adjust for and improve the understanding of mediating effects and bias implications of confounders [84, 85]. Furthermore, the effect of investigated variables and confounders on injury risk may change over time [15, 86] due to changes in the mechanical properties of muscle, tendon, and bone tissue [83] in response to training and match loads. Whilst several included studies accounted for bowling workloads [51, 52, 64], future research should longitudinally account for multiple variables as time-varying effect-measure modifiers and/or time varying confounders [87].
Statistical analysis and reporting bias
Studies classified as having a high risk of statistical analysis and reporting bias were typified by inadequate reporting [42, 54, 55] and when the 95% Confidence Intervals of risk ratios for variables reported to be significant included 1.0 [49, 64]. Studies with reported associations based on p-values alone [43, 45, 48, 56, 57, 60, 62, 65] were rated as moderate risk, as p-values do not provide a good measure of evidence regarding a hypothesis or quantify the size of an effect [88]. The use of post-hoc power analyses to detect differences in bowlers with and without injury [46, 47] was judged to increase risk of bias, as it is not conceptually valid to interpret power pertaining to observed study results [89], as this should be included in study rationale and design prior to conduct [90].
Low risk (and primarily more recent) studies [41, 44, 50,51,52,53, 58, 59, 61, 63] were characterised by appropriate interpretations of associations based on effect sizes [41, 50, 53, 58, 61, 63], relative risk ratios [50], predictive values [52], and regression models [44, 51, 53, 59]. Whilst the inclusion of these measures to accompany p-value and Confidence Interval reporting is promising, further steps are required to produce more transparent and informative research. Approaches such as Bayesian methods, likelihood ratios, and Bayes Factors may more directly address the size and certainty of effects, or whether a hypothesis is correct [71, 88]. Furthermore, future researchers should report both relative and absolute measures of association to draw conclusions, as these may better identify minimal important differences in injury risk [91].
Summary of evidence
Notwithstanding reported discrepancies, the credibility of extracted results in this review are potentially compromised due to 23 of the 25 included studies being assessed as having an overall high risk of bias. Regardless, discussion within this context of the summary of evidence can inform priorities and strategies for future research.
Age
Inconsistent associations of age and injury in adolescent populations [41, 54, 59] may be due to disparate study designs and injury outcomes of included studies; as radiological abnormalities were assessed in a cross-sectional study [54], symptomatic LBSI was examined in retrospective research [59], and a combination of these outcomes was investigated prospectively [41]. The association of younger age and LBSI in professional bowlers [51] is supported by research reporting fast bowlers with LBSI possessing mean age of 22.2 years [13], being predominantly 24 years or younger [92], and demonstrating 3.7 to 6.7 times greater likelihood of sustaining these injuries than other age groups if they are under the age of 22 [20].
These findings are consistent with longitudinal measurements of bone turnover and BMD indicating lumbar bone accrual continues beyond longitudinal growth cessation [93,94,95], with 23.1 to 24.9 years reported as the 95% Confidence Interval for attainment of peak BMD in males [95]. The lumbar vertebrae undergo maturation at secondary ossification centres in the vertebral body ring [96,97,98], and the mamillary, transverse and spinous processes [96] through cartilaginous, apophyseal and epiphyseal stages [98] that do not correlate consistently with chronological age [96,97,98,99]. Furthermore, the timing and rates of growth and maturation of lumbar musculature are variable; as Erector Spinae and Multifidus often reach maximal CSA before skeletal maturity, whereas Psoas Major and QL can continue to increase in size after skeletal maturity [100].
Previous reviews examining LBP and lumbar spine injury in fast bowlers have classified adolescent [26] and adult [16] cohorts separately, with caution advised in generalising injury associated factors from cricketers below 18 years to adults [16, 26]. Whilst disparities in spinal anatomy exist between adolescents and adults [101], future research should examine neuromuscular [102], physiological and mechanical adaptations [83] as a function of training age [83, 103] and maturation status [102], as these factors may influence resilience to fast bowling [1]. Regardless, a linear relationship between skeletal maturity and chronological age is disputable [104], and the rationale for classifying fast bowlers by chronological age should be re-considered. Whilst one included study [41] reported the non-significance of skeletal age, future studies should investigate associations of lumbar maturation metrics and injury outcomes.
LBP and lumbar spine injury
Irrespective of study design, the residual effects of previous injury potentially distort reported associations between investigated variables and reported outcomes of LBP and lumbar spine injury. An index LBSI in a fast bowler may be associated with recurrence at the same site, contralaterally, or at a different lumbar level [13, 105]; however, the nature of any association is undetermined, as the effects of injury on the cellular and mechanical aspects of lumbar bone are unknown. Future studies should clearly define the nature and site of previous injuries and employ statistical designs to account for their influence on investigated variables and injury incidence.
Comparing the significance of variables derived from studies that defined outcomes as varied as LBP in the absence of radiology [48, 50, 57, 58, 61, 62], radiological abnormalities in the absence of LBP [43, 53,54,55,56, 65], or a combination of LBP, abnormal radiology and missed playing time [42, 44,45,46,47, 51, 52, 59, 60, 63, 64] is problematic. Whilst the appearance of LBP has been reported to be a common finding in fast bowlers without accompanying missed playing time [9]; spondylolysis is the most common cause of LBP in young athletes [106], and LBSI should be suspected in a fast bowler presenting with LBP contralateral to their bowling arm side [12]. The significance of LBP as a surrogate for lumbar spine injury in fast bowlers is yet to be determined due to previously described attrition biases in the published literature [41,42,43, 45,46,47,48,49,50, 53, 60, 61, 65], and studies being cross sectional [54,55,56, 62, 63], retrospective [57,58,59,60,61, 64], or prospective with limited follow up periods [42, 46,47,48,49,50, 52, 61]. To better understand the relationship between LBP and lumbar spine injury in fast bowlers, there is a requirement for longitudinal studies that concurrently examine these outcomes over prolonged surveillance periods.
BMC/BMD
Injury causality cannot be established in cross-sectional research that reported trends for less marked asymmetry of lumbar BMC/BMD being associated with LSF history [63]. These trends are supported by lumbar vertebral BMC/BMD being reduced at 21 to 24 weeks post LSF in fast bowlers in comparison to baseline [105]; and a post-injury delay in BMC/BMD recovery may be associated with LBSI recurrences [105]. The contrasting trend for bowlers with greater contralateral side BMD who developed LBSI [41] suggests that LBSI risk may be somewhat independent of BMD. Future studies should aim to investigate additional factors that may regulate bone modelling and adaptation to mechanical loading such as vitamin D status, genetic variants associated with vitamin D and collagen pathways [107], and vertebral trabecular bone quality [108].
Trunk and lumbar muscle morphology and morphometry
Contrasting QL asymmetry associations may be consequential of a limited number of images available for analysis [44, 46, 47], and distinctive CSA [46, 47] and volumetric [44] assessments. The generation of volumes via muscle profile templates over multiple years [44] possibly distorted measurements, as QL CSA growth is non-uniform during adolescence [100]. Disparities may also reflect variability in the size, number, and attachments of QL fascicles between individuals [109]. Whilst increases in asymmetry have been linked to higher lumbopelvic lateral flexion loads in fast bowlers [110], finite element modelling suggests that asymmetry may reduce lumbar loads due to the geometrical proximity of QL’s line of action to the centre of spinal rotation and impacted facet joints during fast bowling postures [111].
The hypothesis of modified trunk control explaining the association between reduced non-bowling arm side Internal Oblique thickness and LBP [62] is problematic as bowling workloads were not accounted for as a confounder in this cross-sectional study. LBP-related reductions in bowling volume and intensity prior to testing may have influenced this finding, as repetitive fast bowling can preferentially hypertrophy the non-bowling arm side Internal Oblique over the course of a cricket season [112].
Since fatty infiltration within trunk and lumbar musculature has been associated with LBP [113], future research should quantify lean muscle mass. Whilst individual muscles are postulated to influence lumbar function due to spinal and fascial attachments [114], lumbopelvic function depends on coordinated activation [115] rather than specific muscles with unique architectural properties or mechanical advantages [116]. High levels of paraspinal and gluteal muscle activation have been reported around BFC and BR in injury-free fast bowlers [21], and whilst the applicability of these findings is unknown, further research is required to establish the role of trunk and lumbopelvic musculature in LBP and lumbar spine injury in fast bowlers.
Presence of BMO
Distinctions in associations between BMO and future lumbar spine injury may be attributed to studies reporting the significance of detected BMO [45, 52] and BMO intensity ratios [64] with p-values [45], predictive values [52], and risk ratios [52, 64]. Earlier symptom reporting with detected BMO and cortical breach in comparison to no cortical breach [45] may be indicative of bowlers being at a later stage of the bone stress injury continuum at study commencement [117].
Whilst excellent reliability for BMO intensity quantification has been reported [64, 79]; the inter-rater reliability of BMO detection is uncertain, as its Kappa was 0.483 (95% CI 0.368–0.580) [79] in relation to one cohort [52] and not reported in two others [45, 64]. The reporting of BMO intensity ratio ≥ 2.0 resulting in a 1.8 times greater risk of sustaining LBSI in the following 12 months should be viewed cautiously as the 95% Confidence Interval associated with its risk ratio included 1.0 (95% CI 0.6–5.5) [64].
Whilst a relative risk of 22.3 was reported for detected BMO leading to a symptomatic LBSI in adolescents, 61% of all participants with BMO detected on one or more scans did not experience a symptomatic LBSI; with 37% experiencing persistent BMO and no symptoms, and the remaining 24% experiencing BMO resolution and no symptoms [52]. The undetermined significance of BMO presents implications for its measurement in future research, and in addition to BMO detection and intensity, the quantification of lumbar intervertebral disc degeneration [118], vertebral morphometry [119], trabecular bone quality [108], paraspinal muscle morphometry [120], facet orientation [121], and facet degeneration [122] may be prudent, as these variables potentially influence relationships between quantified BMO and symptoms.
Biomechanics of fast bowling
Reported associations from research relating to front-on shoulder alignment at BFC [42, 54], SCR [42, 54, 56, 65] and a mixed technique [43, 54,55,56, 65] were replicated in only one [60] of six subsequent studies [49, 53, 58,59,60,61]. Likewise, disparities exist between the reported significance of trunk and lumbar lateral flexion [49, 53, 58, 59, 61], flexion/extension [49, 53, 58, 61], and rotation [49, 53, 58, 61], as well as hip [42, 49, 53, 60] and knee angles [42, 49, 53, 56, 60, 65] during FFC. The lack of reproducibility in biomechanical research is concerning since the modification of shoulder alignment, SCR, a mixed technique, trunk lateral flexion, and lower limb kinematics are emphasised in contemporary injury prevention and coaching programs [123, 124].
The non-consensus of predisposing or predictive biomechanical variables is understandable as these were gathered from research with disparate cohorts and study designs. Biomechanical research was conducted across adolescent [42, 43, 49, 54,55,56, 59, 61, 65] and adult [53, 57, 58, 60, 61] cohorts at club/school [42, 43, 56], high-performance/elite [53,54,55, 57,58,59,60,61, 65], and diverse [49] skill levels. The utility of biomechanical factors from cross-sectional [54,55,56] and retrospective [57,58,59,60,61] cohorts for injury prediction and prevention is questionable, since fast bowling techniques employed by these bowlers may have been influenced by existing or previous injury, as pain may alter muscle activity and mechanical behaviours at multiple levels of the motor system [125]. Furthermore, as previous LBP or lumbar spine injury was documented in only one biomechanical study [61], the significance of biomechanical factors collected from prospectively monitored cohorts that did not account for this [42, 43, 49, 60, 65] may be similarly affected.
Precise temporal characteristics of BFC and FFC were reported in only three studies [53, 58, 61], and their limited reporting [42, 43, 49, 54,55,56, 59, 60, 65] may have caused variables across biomechanical research to be collected from arbitrary and inconsistent points of the fast bowling action. Formulating precise and consistently defined parameters for the measurement and reporting of these events is necessary to improve the external validity of research. The restriction of data analysis in all included biomechanical studies [42, 43, 49, 53,54,55,56, 58,59,60,61, 65] to discrete time points or joint and/or segmental maxima and minima, represents a clear limitation [126], and future research needs to assess coordinated movement patterns utilising continuous datasets over the entire fast bowling movement [127]. Moreover, assessing variability in movement may provide an improved understanding of stresses that potentially reduce or increase cumulative loads on internal structures [76, 128] of fast bowlers, and these detailed analyses can be achieved with time-series based procedures such as Statistical Parametric Map** [126, 129].
The threshold for SCR deemed to be “excessive” was inconsistent, with this being greater than 10° [54,55,56], 20° [43, 65], 30° [53, 58, 60] or 40° [59]. 2-D studies [42, 43, 54, 56, 59, 65] captured kinematic data with one high-speed camera positioned laterally and another overhead, thus introducing the risk of perspective error due to the multi-planar nature of fast bowling [5]. Moreover, SCR is a 2-D description of shoulder alignment in the transverse plane [60] that does not consistently represent 3-D derived fast bowling spinal kinematics [58, 130, 131], and bowlers classified with mixed and non-mixed actions exhibited no significant differences in lower trunk extension, lateral flexion, and axial rotation percentages utilised in the fast bowling action [130]. These findings further indicate a requirement for future research to investigate alternative methods of analysis and classification of fast bowling techniques.
Whilst 3-D studies [49, 53, 58, 60] utilised numerous cameras to reconstruct a three-dimensional space, they defined the thoracic and lumbar spine as singular rigid body segments [126]. Individual thoracic and lumbar vertebrae move in an uncorrelated manner [132, 133], and the L4 and L5 posterior elements may experience dissimilar maximal stresses in response to an applied physiological load [134]. Biomechanical data collected with rigid segments should be viewed with caution [133], and future research must explore methodologies capable of assessing multi-segmental motion of the thoracic and lumbar regions [133] and the quantification of spinal curvature [126] during fast bowling.
The significance of excessive lateral flexion in relation to injury thorax [49, 58], thoracolumbar [53], lumbopelvic [49, 53], trunk [59] and lumbar [61] segments is uncertain. In studies that have reported excessive lateral flexion to be significant, its presence may have predated or be consequential of LBP history [58], and it has been associated with both symptomatic and asymptomatic bowlers [49, 53]. In described conference proceedings, fast bowlers who sustained LBSI utilised lower proportions of available lower trunk lateral flexion range and a non-significantly increased amount of lower trunk extension than non-injured counterparts [10].
Increases in lumbar extension at BFC [61] and FFC [53] deemed to elevate LBP and LBSI risk respectively were coexistent with increased anterior pelvic tilt in one study [53], and analysis of continuous datasets may illuminate causal interactions between these variables and injury. Whilst the described influences of thoracic and lumbar rotation [49, 53, 61] are conflicting, reported increases in thoracic rotation away from the direction of delivery in bowlers without LBP history [61] may inform biomechanical and physical preparation initiatives designed to reduce lumbar spine stress during fast bowling. More detailed analyses of lateral flexion, extension and rotation are required as these movements have been designated as injurious due to hypothesised stresses on posterior lumbar vertebral elements [134, 135].
The reported association of increased rear hip flexion at BFC instant with LBSI is proposed to be representative of poor pelvifemoral control [53], which is defined by the interaction of the pelvis on the femur [136]. Whilst no reliable or valid test for this entity exists, this is associated with perceptions amongst cricket coaches that rear leg kinematics are important determinants of fast bowling performance [137], and future research investigating the origins and consequences of observed kinematics at BFC may inform interventions to improve performance and reduce injury.
Although reduced front hip flexion during FFC is theorised to cause injury due to higher GRF [42, 60] and forces transmitted to the lumbar region [49]; more flexed front hip angles in conjunction with increased pelvic anterior tilt and ipsilateral drop are also proposed to be detrimental [53]. Whilst a straighter front knee during FFC [42, 60] is suggested to be a trade-off between improved bowling performance and heightened injury risk [138]; foot horizontal impulse magnitude [139], plant angle and strike position [140] during FFC may be more important determinants of knee kinematics and GRF.
The absence of consistent findings relating high GRF at FFC with injury [42, 49, 53, 54, 56, 60, 61] may reflect discrepancies of GRF in laboratory versus match settings due to shortened run-up lengths and altered foot placement strategies [30]. Attainment of match intensity bowling speeds during testing may improve the ecological validity of future research, as reduced bowling speeds may cause disproportionately large reductions in lumbar loads [141]. IMUs may contribute to the assessment of match intensity fast bowling kinetics in future studies, as they can be used in a field environment and have good measurement validity [61, 142].
GRF dissipation may supersede the influence of GRF magnitudes since reduced force attenuation during landing may increase stresses on more proximal structures [143, 144]. Investigating the force attenuating ability of the lower limbs and lumbopelvic region through eccentric strength [145], range of motion [146, 147], and stiffness [148, 149] assessments should be considered in future research. Whilst higher lumbar flexion and lateral flexion loads have been associated with injury [49], previous research has not investigated the influence of muscle forces on lumbar compressive loads [6, 49, 150], and future studies should incorporate musculoskeletal models that better simulate spinal loading [151].
As biomechanical research has been conducted in primarily male and most likely Caucasian populations, the generalisability of findings to females and other racial groups may be limited. Female fast bowlers may adopt a bowling technique where BR speed is contributed to more by whole body angular momentum and pelvis and trunk rotation about the longitudinal axis in comparison to their male colleagues [152]. Furthermore, during landings, males demonstrate greater centre of mass displacement indicating a softer landing technique than females to absorb forces experienced during initial ground impact [153]. Differences in neuromuscular control strategies adopted during fast bowling and landing may alter the influence of extrinsic and intrinsic variables on the development of LBP and lumbar spine injury in female fast bowlers, thus indicating a requirement for future research in female fast bowling populations.
Physical characteristics
Conclusions from included studies investigating physical characteristics [41, 42, 46,47,48,49, 54, 56, 57, 59] may inform contemporary programs for injury prevention [154, 155]. Prospective [41, 42, 46,47,48,49], cross-sectional [54, 56], and retrospective [57, 59] designs, as well as indeterminate reliability of musculoskeletal screening procedures [156] may have contributed to inconsistencies in results.
The reporting of a reduced lumbo-pelvic stability test score resulting in a 1.7 times increased risk of sustaining lower back injury should be viewed cautiously as the 95% Confidence Interval associated with its risk ratio included 1.0 (95% CI 0.78–4.10) [49]. This test is based on the Sahrmann five-level core stability test [157], which displays questionable reliability and validity; as abdominal activity does not sequentially increase during its ascending levels [158], and the ICC for test–retest reliability is moderate (r = 0.649) [159]. Future research should examine methodologies to assess lumbopelvic stability in upright positions evaluating dynamic lumbar spine and pelvis control in sagittal, frontal, and transverse planes of motion over the weightbearing leg [160, 161].
The assessment of pelvifemoral stability with a single leg decline squat conceptually lacks validity, as the presence of a decline alters femoral rotation and knee valgus [162], displaces the body’s centre of mass posteriorly [163], and reduces hip strength required to control knee alignment [162, 164]. Future assessments of hip control should focus on hip muscle strength, and multiplanar knee, femoral, pelvis and spine alignment in single leg stance [165]. Whilst reduced lumbar proprioception may result in increased end-range lumbar loading [166], assessing this at speeds more representative of fast bowling with simulated back and front foot landings may be valuable in future studies.
The significance of reduced lumbar extensor endurance in fast bowlers is uncertain as it was investigated in three studies [49, 57, 59] and associated with injury in only one [49]. Future research investigating the significance of lumbar extensor strength and endurance should quantify lumbar sagittal curvature and extensor muscle volume, as these factors may influence the magnitude of muscle forces required for biomechanical stability of the lumbopelvic region [167, 168].
Limitations
The heterogeneity of investigated variables did not enable a meta-analysis to be performed, and yet to be identified variables may be associated with LBP and lumbar spine injury. Whilst the level of agreement of risk assessments for individual QUIPS bias domains was high, final judgements were subjective to some degree. It is possible that relevant articles were not identified during the search process, and studies published in languages other than English may have been overlooked. Positive publication bias was a likely factor in the non-retrieval of studies, and the exclusion of grey literature and conference proceedings may have contributed to this.
Conclusion
This review has identified inconsistencies in findings from studies investigating associations between intrinsic variables and LBP and lumbar spine injury. These discrepancies may be related to differences in study design, injury definitions, participant characteristics, measurement parameters, and statistical analyses. LBP and lumbar spine injury occurrence in fast bowlers remain high, and this may be due to an absence of low bias studies that have informed recommendations for their prevention. Careful study design, precise measurement, appropriate statistical analysis, and clearly defined measurement and injury outcomes represent important strategies for minimising bias and improving the representativeness of findings. Future research should prioritise analysis of continuous datasets, models that better represent lumbar kinematics and kinetics during fast bowling, and improved quantification of previous injury, lumbar anatomical features and lumbar maturation.
Availability of data and materials
All data and material reported in this systematic review is from peer-reviewed publications. All extracted data is included in this published article [and its supplementary information files].
Abbreviations
- 2-D:
-
Two-dimensional
- 3-D:
-
Three- dimensional
- BFC:
-
Back foot contact
- BMC:
-
Bone mineral content
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- BMO:
-
Bone marrow oedema
- BR:
-
Ball release
- CHARMS:
-
Checklist for critical Appraisal and data extraction for systematic Reviews of prediction Modelling Studies
- CI:
-
Confidence Interval
- CL:
-
Contralateral
- CSA:
-
Cross sectional area
- CT:
-
Computed Tomography
- DAGs:
-
Directed acyclic graphs
- DEXA:
-
Dual Energy X-ray Absorptiometry
- EO:
-
External Oblique
- F/E:
-
Flexion/extension
- FFC:
-
Front foot contact
- GRF:
-
Ground reaction forces
- HSS:
-
Hip-shoulder separation
- IMUs:
-
Inertial measurement units
- IO:
-
Internal Oblique
- LBP:
-
Low Back Pain
- LBSI:
-
Lumbar bone stress injury
- LRE:
-
Lumbar Reposition Error
- LSF:
-
Lumbar stress fracture
- MF:
-
Multifidus
- MRI:
-
Magnetic Resonance Imaging
- QL:
-
Quadratus Lumborum
- QUIPS:
-
Quality in Prognostic Studies
- ROC:
-
Receiver operating characteristic
- RR:
-
Risk ratio
- SCR:
-
Shoulder counter rotation
- SEBT:
-
Star Excursion Balance Test
- SPECT:
-
Single Photon Emission Computerised Tomography
- US:
-
Ultrasound
References
Orchard JW, Kountouris A, Sims K. Incidence and prevalence of elite male cricket injuries using updated consensus definitions. Open Access J Sport Med. 2016;7:187–94. https://doi.org/10.2147/OAJSM.S117497.
Kurittu E, Vasankari T, Brinck T, Parkkari J, Heinonen OJ, Kannus P, Hänninen T, Köhler K, Leppänen M. Injury incidence and prevalence in Finnish top-level football–one-season prospective cohort study. Sci Med Football. 2022;6(2):141–7. https://doi.org/10.1080/24733938.2021.1917775.
Moore IS, Ranson C, Mathema P. Injury risk in international rugby union: three-year injury surveillance of the Welsh national team. Orthop J Sport Med. 2015;3(7):2325967115596194. https://doi.org/10.1177/2325967115596194.
Orchard JW, Blanch P, Paoloni J, Kountouris A, Sims K, Orchard JJ, Brukner P. Cricket fast bowling workload patterns as risk factors for tendon, muscle, bone and joint injuries. Br J Sport Med. 2015;49(16):1064–8. https://doi.org/10.1136/bjsports-2014-093683.
Bartlett RM, Stockill NP, Elliott BC, Burnett AF. The biomechanics of fast bowling in men’s cricket: a review. J Sport Sci. 1996;14(5):403–24. https://doi.org/10.1080/02640419608727727.
Ferdinands RE, Kersting U, Marshall RN. Three-dimensional lumbar segment kinetics of fast bowling in cricket. J Biomech. 2009;42(11):1616–21. https://doi.org/10.1016/j.jbiomech.2009.04.035.
Hurrion PD, Dyson R, Hale T. Simultaneous measurement of back and front foot ground reaction forces during the same delivery stride of the fast-medium bowler. J Sport Sci. 2000;18(12):993–7. https://doi.org/10.1080/026404100446793.
Annear PT, Chakera TM, Foster DH, Hardcastle PH. Pars interarticularis stress and disc degeneration in cricket’s potent strike force: the fast bowler. Aust N Z J Surg. 1992;62(10):768–73. https://doi.org/10.1111/j.1445-2197.1992.tb06915.x.
Dennis RJ, Finch CF, Farhart PJ. Is bowling workload a risk factor for injury to Australian junior cricket fast bowlers? Br J Sport Med. 2005;39(11):843–6. https://doi.org/10.1136/bjsm.2005.018515. discussion -6.
Ranson C, Burnett A, King M, O’Sullivan P, Cornish R, Batt M. Acute lumbar stress injury, trunk kinematics, lumbar MRI and paraspinal muscle morphology in fast bowlers in cricket. In ISBS - Conf Proc Arch. Injuries/Rehabilitation; 2008. p. 233–6.
Johnson M, Ferreira M, Hush J. Lumbar vertebral stress injuries in fast bowlers: a review of prevalence and risk factors. Phys Ther Sport. 2012;13(1):45–52. https://doi.org/10.1016/j.ptsp.2011.01.002.
Orchard J, Saw R, Kountouris A, Redrup D, Farhart P, Sims K. Management of lumbar bone stress injury in cricket fast bowlers and other athletes. S Afr J Sport Med. 2023;35(1). https://doi.org/10.17159/2078-516X/2023/v35i1a15172.
Saw R, Saw A, Kountouris A, Orchard J. Upper lumbar bone stress injuries in Elite cricketers. Clin J Sport Med. 2022;32(2):e121–5. https://doi.org/10.1097/JSM.0000000000000884.
Singh SP, Rotstein AH, Saw AE, Saw R, Kountouris A, James T. Radiological healing of lumbar spine stress fractures in elite cricket fast bowlers. J Sci Med Sport. 2021;24(2):112–5. https://doi.org/10.1016/j.jsams.2020.06.018.
Meeuwisse WH, Tyreman H, Hagel B, Emery C. A dynamic model of etiology in sport injury: the recursive nature of risk and causation. Clin J Sport Med. 2007;17(3):215–9. https://doi.org/10.1097/JSM.0b013e3180592a48.
Olivier B, Taljaard T, Burger E, Brukner P, Orchard J, Gray J, Botha N, Stewart A, Mckinon W. Which extrinsic and intrinsic factors are associated with non-contact injuries in adult cricket fast bowlers? Sport Med. 2016;46(1):79–101. https://doi.org/10.1007/s40279-015-0383-y.
Finch CF, Elliott BC, McGrath AC. Measures to prevent cricket injuries: an overview. Sport Med. 1999;28(4):263–72. https://doi.org/10.2165/00007256-199928040-00004.
Dennis RJ, Finch CF, McIntosh AS, Elliott BC. Use of field-based tests to identify risk factors for injury to fast bowlers in cricket. Br J Sport Med. 2008;42(6):477–82. https://doi.org/10.1136/bjsm.2008.046698.
Davies R, du Randt R, Venter D, Stretch R. Cricket: nature and incidence of fast bowling injuries at an elite, junior level and associated risk factors. S Afr J Sport Med. 2008;20(4):115–8. https://doi.org/10.17159/2078-516X/2008/v20i4a27520.
Blanch P, Orchard J, Kountouris A, Sims K, Beakley D. Different tissue type categories of overuse injuries to cricket fast bowlers have different severity and incidence which varies with age. S Afr J Sport Med. 2015;27(4):108–13. https://doi.org/10.17159/2078-516x/2015/v27i4a436.
Forrest M, Hecimovich M, Dempsey A. Lumbopelvic muscle activation patterns in adolescent fast bowlers. Eur J Sport Sci. 2016;16(6):677–84. https://doi.org/10.1080/17461391.2015.1135985.
Martin C, Olivier B, Benjamin N. Asymmetrical abdominal muscle morphometry is present in injury free adolescent cricket pace bowlers: a prospective observational study. Phys Ther Sport. 2017;28:34–42. https://doi.org/10.1016/j.ptsp.2017.08.078.
Bartlett R, Bussey M. Sports biomechanics: reducing injury risk and improving sports performance. New York, NY: Routledge; 2013.
Hamstra-Wright KL, HuxelBliven KC, Napier C. Training load capacity, cumulative risk, and bone stress injuries: a narrative review of a holistic approach. Front Sport Act Living. 2021;3:665683. https://doi.org/10.3389/fspor.2021.665683.
Morton S, Barton CJ, Rice S, Morrissey D. Risk factors and successful interventions for cricket-related low back pain: a systematic review. Br J Sport Med. 2014;48(8):685–91. https://doi.org/10.1136/bjsports-2012-091782.
Forrest MRL, Hebert JJ, Scott BR, Brini S, Dempsey AR. Risk factors for non-contact injury in adolescent cricket pace bowlers: a systematic review. Sport Med. 2017;47:2603–19. https://doi.org/10.1007/s40279-017-0778-z.
Higgins JP, Altman DG, Gøtzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, Cochrane Bias Methods Group. The Cochrane Collaboration’s tool for as assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Whiting P, Wolff R, Mallett S, Simera I, Savovic J. A proposed framework for develo** quality assessment tools. Syst Rev. 2017;6(1):204. https://doi.org/10.1186/s13643-017-0604-6.
Frampton G, Whaley P, Bennett M, Bilotta G, Dorne JL, Eales J, James K, Kohl C, Land M, Livoreil B, Makowski D. Principles and framework for assessing the risk of bias for studies included in comparative quantitative environmental systematic reviews. Environ Evid. 2022;11(1):12.
Senington B, Lee RY, Williams JM. Ground reaction force, spinal kinematics and their relationship to lower back pain and injury in cricket fast bowling: a review. J Back Musculoskelet Rehabil. 2018;31(4):671–83. https://doi.org/10.3233/BMR-170851.
Ranson CA, Kerslake RW, Burnett AF, Batt ME, Abdi S. Magnetic resonance imaging of the lumbar spine in asymptomatic professional fast bowlers in cricket. J Bone Jt Surg. 2005;87(8):1111–6. https://doi.org/10.1302/0301-620X.87B8.16405.
Perrett C, Lamb P, Bussey M. Is there an association between external workload and lower-back injuries in cricket fast bowlers? A systematic review. Phys Ther Sport. 2020;41:71–9. https://doi.org/10.1016/j.ptsp.2019.11.007.
Stovitz SD, Verhagen E, Shrier I. Distinguishing between causal and non-causal associations: implications for sports medicine clinicians. Br J Sport Med. 2019;53(7):398–9. https://doi.org/10.1136/bjsports-2017-09852034.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9. https://doi.org/10.1186/2046-4053-4-1.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org. Accessed 20 Aug 2020.36.
Moons KG, de Groot JA, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. 2014;11(10):e1001744.
Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–8. https://doi.org/10.7326/0003-4819-158-4-201302190-00009.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MMG, Sterne JAC, Bossuyt PMM, QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009.
Grooten WJA, Tseli E, Ang BO, Boersma K, Stalnacke BM, Gerdle B, Enthoven P. Elaborating on the assessment of the risk of bias in prognostic studies in pain rehabilitation using QUIPS-aspects of interrater agreement. Diagn Progn Res. 2019;3(1):1–11. https://doi.org/10.1186/s41512-019-0050-0.
Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85(3):257–68. https://doi.org/10.1093/ptj/85.3.257.
Keylock L, Alway P, Felton P, McCaig S, Brooke-Wavell K, King, M, Peirce N. Lumbar bone stress injuries and risk factors in adolescent cricket fast bowlers. J Sport Sci. 2022:1–7. https://doi.org/10.1080/02640414.2022.2080161.
Foster D, John D, Elliott B, Ackland T, Fitch K. Back injuries to fast bowlers in cricket: a prospective study. Br J Sport Med. 1989;23(3):150–4. https://doi.org/10.1136/bjsm.23.3.150.
Burnett AF, Khangure MS, Elliott BC, Foster DH, Marshall RN, Hardcastle PH. Thoracolumbar disc degeneration in young fast bowlers in cricket: a follow-up study. Clin Biomech. 1996;11(6):305–10. https://doi.org/10.1016/0268-0033(96)00007-1.
Engstrom CM, Walker DG, Kippers V, Mehnert AJH. Quadratus lumborum asymmetry and L4 pars injury in fast bowlers: a prospective MR study. Med Sci Sport Exerc. 2007;39(6):910–7. https://doi.org/10.1249/mss.0b013e3180408e25.
Ranson CA, Burnett AF, Kerslake RW. Injuries to the lower back in elite fast bowlers: acute stress changes on MRI predict stress fracture. J Bone Jt Surg. 2010;92(12):1664–8. https://doi.org/10.1302/0301-620X.92B12.24913.
Kountouris A, Portus M, Cook J. Quadratus lumborum asymmetry and lumbar spine injury in cricket fast bowlers. J Sci Med Sport. 2012;15(5):393–7. https://doi.org/10.1016/j.jsams.2012.03.012.
Kountouris A, Portus M, Cook J. Cricket fast bowlers without low-back pain have larger quadratus lumborum asymmetry than injured bowlers. Clin J Sport Med. 2013;23(4):300–4. https://doi.org/10.1097/JSM.0b013e318280ac88.
Olivier B, Stewart AV, McKinon W. Injury and lumbar reposition sense in cricket pace bowlers in neutral and pace bowling specific body positions. Spine J. 2014;14(8):1447–53. https://doi.org/10.1016/j.spinee.2013.08.036.
Bayne H, Elliott B, Campbell A, Alderson J. Lumbar load in adolescent fast bowlers: a prospective injury study. J Sci Med Sport. 2016;19(2):117–22. https://doi.org/10.1016/j.jsams.2015.02.011.
Olivier B, Gillion N, Stewart AV, McKinon W. Reduced nondominant lumbar multifidi cross-sectional area is a precursor of low back injury in cricket fast bowlers. Scand J Med Sci Sport. 2017;27(12):1927–33. https://doi.org/10.1111/sms.12814.
Alway P, Brooke-Wavell K, Langley B, King M, Peirce N. Incidence and prevalence of lumbar stress fracture in English County Cricket fast bowlers, association with bowling workload and seasonal variation. BMJ Open Sport Exerc Med. 2019;5(1):e000529. https://doi.org/10.1136/bmjsem-2019-000529.
Kountouris A, Sims K, Beakley D, Saw AE, Orchard J, Rotstein A, Cook JL. MRI bone marrow oedema precedes lumbar bone stress injury diagnosis in junior elite cricket fast bowlers. Br J Sport Med. 2019;53(19):1236–9. https://doi.org/10.1136/bjsports-2017-097930.
Alway P, Felton P, Brooke-Wavell K, Peirce N, King M. Cricket fast bowling technique and lumbar bone stress injury. Med Sci Sport Exerc. 2021;53(3):581–9. https://doi.org/10.1249/MSS.0000000000002512.
Elliott BC, Hardcastle PH, Burnett AF, Foster DH. The influence of fast bowling and physical factors on radiologic features in high performance young fast bowlers. Res Sport Med Int J. 1992;3(2):113–30. https://doi.org/10.1080/15438629209517008.
Hardcastle P, Annear P, Foster D, Chakera T, McCormick C, Khangure M, Burnett A. Spinal abnormalities in young fast bowlers. J Bone Jt Surg. 1992;74(3):421–5. https://doi.org/10.1302/0301-620X.74B3.1587894.
Elliott BC, Davis JW, Khangure MS, Hardcastle P, Foster D. Disc degeneration and the young fast bowler in cricket. Clin Biomech. 1993;8(5):227–34. https://doi.org/10.1016/0268-0033(93)90030-L.
Stuelcken MC, Ginn KA, Sinclair PJ. Musculoskeletal profile of the lumbar spine and hip regions in cricket fast bowlers. Phys Ther Sport. 2008;9(2):82–8. https://doi.org/10.1016/j.ptsp.2008.02.002.
Stuelcken MC, Ferdinands RE, Sinclair PJ. Three-dimensional trunk kinematics and low back pain in elite female fast bowlers. J Appl Biomech. 2010;26(1):52–61. https://doi.org/10.1123/jab.26.1.52.
Sims K, Saw R, Saw AE, Kountouris A, Orchard JW. Multiple risk factors associated with lumbar bone stress injury in youth cricket fast bowlers. J Sp Exerc Sci. 2021;5(2):92–100. https://doi.org/10.36905/jses.2021.02.01.
Portus MR, Mason BR, Elliot BC, Pfitzner MC, Done RP. Technique factors related to ball release speed and trunk injuries in high performance cricket fast bowlers. Sport Biomech. 2004;3(2):263–83. https://doi.org/10.1080/14763140408522845.
Senington B, Lee RY, Williams JM. Biomechanical risk factors of lower back pain in cricket fast bowlers using inertial measurement units: a prospective and retrospective investigation. BMJ Open Sport Exerc Med. 2020;6(1):e000818. https://doi.org/10.1136/bmjsem-2020-000818.
Gray J, Aginsky KD, Derman W, Vaughan CL, Hodges PW. Symmetry, not asymmetry, of abdominal muscle morphology is associated with low back pain in cricket fast bowlers. J Sci Med Sport. 2016;19(3):222–6. https://doi.org/10.1016/j.jsams.2015.04.009.
Alway P, Peirce N, King M, Jardine A, Brooke-Wavell K. Lumbar bone mineral asymmetry in elite cricket fast bowlers. Bone. 2019;127:537–43. https://doi.org/10.1016/j.bone.2019.07.030.
Taylor J, Saw AE, Saw R, Sims K, Kountouris A. Presence of bone marrow oedema in asymptomatic elite fast bowlers: implications for management. Bone. 2021;143:115626. https://doi.org/10.1016/j.bone.2020.115626.
Elliott B, Khangure M. Disk degeneration and fast bowling in cricket: an intervention study. Med Sci Sport Exerc. 2002;34(11):1714–8. https://doi.org/10.1097/00005768-200211000-0000466.
Satoh M. Bone age: assessment methods and clinical applications. Clin Ped Endoc. 2015;24(4):143–52. https://doi.org/10.1297/cpe.24.14367.
Tripepi G, Jager KJ, Dekker FW, Zoccali C. Selection bias and information bias in clinical research. Nephron Clin Pract. 2010;115(2):c94–9. https://doi.org/10.1159/000312871.
Axén I, Brämberg EB, Bakken AG, Kwak L. Recruiting in intervention studies: challenges and solutions. BMJ Open. 2021;11(1):e044702. https://doi.org/10.1136/bmjopen-2020-044702.
Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiol. 2004;14:615–25. https://doi.org/10.1097/01.ede.0000135174.63482.43.
Abt G, Boreham C, Davison G, Jackson R, Nevill A, Wallace E, Williams M. Power, precision, and sample size estimation in sport and exercise science research. J Sport Sci. 2020;38(17):1933–5. https://doi.org/10.1080/02640414.2020.1776002.
Bullock GS, Mylott J, Hughes T, Nicholson KF, Riley RD, Collins GS. Just how confident can we be in predicting sports injuries? A systematic review of the methodological conduct and performance of existing musculoskeletal injury prediction models in sport. Sport Med. 2022;11:1–14. https://doi.org/10.1007/s40279-022-01698-9.
Barry AE. How attrition impacts the internal and external validity of longitudinal research. J Sch Health. 2005;75(7):267–70. https://doi.org/10.1111/j.1746-1561.2005.00035.x.
Grashow RG, Roberts AL, Zafonte R, Pascual-Leone A, Taylor H, Baggish A, Nadler L, Courtney TK, Connor A, Weisskopf MG. Defining exposures in professional football: professional American-style football players as an occupational cohort. Orthop J Sport Med. 2019;7(2):2325967119829212. https://doi.org/10.1177/2325967119829212.
Teague S, Youssef GJ, Macdonald JA, Sciberras E, Shatte A, Fuller-Tyszkiewicz M, Greenwood C, McIntosh J, Olsson CA, Hutchinson D. Retention strategies in longitudinal cohort studies: a systematic review and meta-analysis. BMC Med Res Methodol. 2018;18(1):1–22. https://doi.org/10.1186/s12874-018-0586-7.
Forrester SE. Selecting the number of trials in experimental biomechanics studies. Int Biomech. 2015;2(1):62–72. https://doi.org/10.1080/23335432.2015.1049296.
Perrett C, Bussey MD, Lamb PF. Movement variability in the spinal kinematics of fast bowlers. ISBS Proc Arch. 2020;38(1):284.
Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med. 2006;25(1):127–41. https://doi.org/10.1002/sim.2331.
Carey DL, Crossley KM, Whiteley R, Mosler A, Ong KL, Crow J, Morris ME. Modeling training loads and injuries: the dangers of discretization. Med Sci Sport Exerc. 2018;50(11):2267–76. https://doi.org/10.1249/MSS.0000000000001685.
Sims K, Kountouris A, Stegeman JR, Rotstein AH, Beakley D, Saw AE, Cook JL. MRI bone marrow edema signal intensity: a reliable and valid measure of lumbar bone stress injury in elite junior fast bowlers. Spine. 2020;45(18):E1166–71. https://doi.org/10.1097/BRS.0000000000003277.
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL. GRADE guidelines: 4. Rating the quality of evidence-study limitations (risk of bias). J Clin Epidemiol. 2011;64(4):407–15. https://doi.org/10.1016/j.jclinepi.2010.07.017.
Ang EC, Robertson AF, Malara FA, O’Shea T, Roebert JK, Schneider ME, Rotstein AH. Diagnostic accuracy of 3-T magnetic resonance imaging with 3D T1 VIBE versus computer tomography in pars stress fracture of the lumbar spine. Skelet Radiol. 2016;45(11):1533–40. https://doi.org/10.1007/s00256-016-2475-7.
Millson HB, Gray J, Stretch RA, Lambert MI. Dissociation between back pain and bone stress reaction as measured by CT scan in young cricket fast bowlers. Br J Sport Med. 2004;38(5):586–91. https://doi.org/10.1136/bjsm.2003.006585.
Kalkhoven J, Watsford M, Impellizzeri FM. A conceptual model and detailed framework for stress-related, strain-related, and overuse athletic injury. J Sci Med Sport. 2020;23(8):726–34. https://doi.org/10.1016/j.jsams.2020.02.002.
Nielsen RØ, Shrier I, Casals M, Nettel-Aguirre A, Møller M, Bolling C, Bittencourt NF, Clarsen B, Wedderkopp N, Soligard T, Timpka T. Statement on methods in sport injury research from the first methods matter meeting, Copenhagen, 2019. J Orthop Sport Phys Ther. 2020;50(5):226–33. https://doi.org/10.2519/jospt.2020.9876.
Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8(1):1–5. https://doi.org/10.1186/1471-2288-8-70.
Mansournia MA, Etminan M, Danaei G, Kaufman JS, Collins G. Handling time varying confounding in observational research. BMJ. 2017;359:j4587. https://doi.org/10.1136/bmj.j4587.
Nielsen RO, Bertelsen ML, Ramskov D, Møller M, Hulme A, Theisen D, Finch CF, Fortington LV, Mansournia MA, Parner ET. Time-to-event analysis for sports injury research part 1: time-varying exposures. Br J Sport Med. 2019;53(1):61–8. https://doi.org/10.1136/bjsports-2018-099408.
Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. Am Stat. 2016;70(2):129–33. https://doi.org/10.1080/00031305.2016.1154108.
Hoenig JM, Heisey DM. The abuse of power: the pervasive fallacy of power calculations for data analysis. Am Stat. 2001;55(1):19–24. https://doi.org/10.1198/000313001300339897.
Mansournia MA, Collins GS, Nielsen RO, Nazemipour M, Jewell NP, Altman DG, Campbell MJ. A CHecklist for statistical Assessment of Medical Papers (the CHAMP statement): explanation and elaboration. Br J Sport Med. 2021;55(18):1009–17. https://doi.org/10.1136/bjsports-2020-103652.
Nielsen RO, Bertelsen ML, Verhagen E, Mansournia MA, Hulme A, Møller M, Casals M. When is a study result important for athletes, clinicians and team coaches/staff? Br J Sport Med. 2017;51(20):1454–5. https://doi.org/10.1136/bjsports-2017-097759.
Stretch RA. Cricket injuries: a longitudinal study of the nature of injuries to South African cricketers. Br J Sport Med. 2003;37(3):250–3. https://doi.org/10.1136/bjsm.37.3.250.
Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Mineral Res. 2011;26(8):1729–39. https://doi.org/10.1002/jbmr.412.
Walsh JS, Henry YM, Fatayerji D, Eastell R. Lumbar spine peak bone mass and bone turnover in men and women: a longitudinal study. Osteoporos Int. 2009;20(3):355–62. https://doi.org/10.1007/s00198-008-0672-5.
Xue S, Kemal O, Lu M, Lix LM, Leslie WD, Yang S. Age at attainment of peak bone mineral density and its associated factors: the National Health and Nutrition Examination Survey 2005–2014. Bone. 2020;131:115163. https://doi.org/10.1016/j.bone.2019.115163.
Cardoso HFV, Rios L. Age estimation from stages of epiphyseal union in the presacral vertebrae. Am J Phys Anthropol. 2011;144(2):238–47. https://doi.org/10.1002/ajpa.21394.
Faizan A, Sairyo K, Goel VK, Biyani A, Ebraheim N. Biomechanical rationale of ossification of the secondary ossification center on apophyseal bony ring fracture: a biomechanical study. Clin Biomech. 2007;22(10):1063–7. https://doi.org/10.1016/j.clinbiomech.2007.04.012.
Uraoka H, Higashino K, Morimoto M, Yamashita K, Tezuka F, Takata Y, Sakai T, Nagamachi A, Murase M, Sairyo K. Study of lesions of the lumbar endplate based on the stage of maturation of the lumbar vertebral body: the relationship between skeletal maturity and chronological age. Eur J Orthop Surg Traumatol. 2018;28:183–7. https://doi.org/10.1007/s00590-017-2032-7.
Albert M, Mulhern D, Torpey MA, Boone E. Age estimation using thoracic and first two lumbar vertebral ring epiphyseal union. J Forensic Sci. 2010;55:287–94. https://doi.org/10.1111/j.1556-4029.2009.01307.x.
Been E, Shefi S, Kalichman L, Bailey JF, Soudack M. Cross-sectional area of lumbar spinal muscles and vertebral endplates: a secondary analysis of 91 computed tomography images of children aged 2–20. J Anat. 2018;233(3):358–69.
Kim HJ, Green DW. Spondylolysis in the adolescent athlete. Curr Opin Pediatr. 2011;23:68–72. https://doi.org/10.1097/MOP.0b013e32834255c2.
Tumkur Anil Kumar N, Oliver JL, Lloyd RS, Pedley JS, Radnor JM. The influence of growth, maturation and resistance training on muscle-tendon and neuromuscular adaptations: a narrative review. Sports. 2021;9(5):59. https://doi.org/10.3390/sports9050059.
Lloyd RS, Oliver JL. The youth physical development model: a new approach to long-term athletic development. Strength Cond J. 2012;34(3):61–72. https://doi.org/10.1519/SSC.0b013e31825760ea.
Cameron C. Can maturity indicators be used to estimate chronological age in children? Ann Hum Biol. 2015;42(4):302–7. https://doi.org/10.3109/03014460.2015.1032349.
Alway P, Peirce N, Johnson W, King M, Kerslake R, Brooke-Wavell K. Activity specific areal bone mineral density is reduced in athletes with stress fracture and requires profound recovery time: a study of elite cricket fast bowlers. J Sci Med Sport. 2022. https://doi.org/10.1016/j.jsams.2022.08.006106.
Wall J, Meehan WP 3rd, Trompeter K, Gissane C, Mockler D, van Dyk N, et al. Incidence, prevalence and risk factors for low back pain in adolescent athletes: a systematic review and meta-analysis. Br J Sport Med. 2022;56(22):1299–306. https://doi.org/10.1136/bjsports-2021-104749.
Varley I, Hughes DC, Greeves JP, Stellingwerff T, Ranson C, Fraser WD, Sale C. The association of novel polymorphisms with stress fracture injury in elite athletes: further insights from the SFEA cohort. J Sci Med Sport. 2018;21(6):564–8. https://doi.org/10.23736/S00224707.21.11871-7.
Ehresman J, Schilling A, Yang X, Pennington Z, Ahmed AK, Cottrill E, Lubelski D, Khan M, Moseley KF, Sciubba DM. Vertebral bone quality score predicts fragility fractures independently of bone mineral density. Spine J. 2021;21(1):20–7. https://doi.org/10.1016/j.spinee.2020.05.202.
Phillips S, Mercer S, Bogduk N. Anatomy and biomechanics of quadratus lumborum. Proc Inst Mech Eng H. 2008;222(2):151–9. https://doi.org/10.1243/09544119JEIM266.
Crewe H, Campbell A, Elliott B, Alderson J. Lumbo-pelvic biomechanics and quadratus lumborum asymmetry in cricket fast bowlers. Med Sci Sport Exerc. 2013;45(4):778–83. https://doi.org/10.1249/MSS.0b013e31827973d1.
de Visser H, Adam CJ, Crozier S, Pearcy MJ. The role of quadratus lumborum asymmetry in the occurrence of lesions in the lumbar vertebrae of cricket fast bowlers. Med Eng Phys. 2007;29(8):877–85. https://doi.org/10.1016/j.medengphy.2006.09.010.
Olivier B, Stewart AV, McKinon W. Side-to-side asymmetry in absolute and relative muscle thickness of the lateral abdominal wall in cricket pace bowlers. S Afr J Sport Med. 2013;25(3):81–6. https://doi.org/10.17159/2413-3108/2013/v25i3a364.
Hildebrandt M, Fankhauser G, Meichtry A, Luomajoki H. Correlation between lumbar dysfunction and fat infiltration in lumbar multifidus muscles in patients with low back pain. BMC Musculoskelet Disord. 2017;18(1):1–9. https://doi.org/10.1186/s12891-016-1376-1.
Panjabi M. The stabilization system of the spine. Part 2: neutral zone and instability hypothesis. J Spinal Disord. 1992;5:390–7. https://doi.org/10.1097/00002517-199212000-00002.
Cholewicki J, Van Vliet JJ. Relative contribution of trunk muscles to the stability of the lumbar spine during isometric exertions. Clin Biomech. 2002;17:99–105. https://doi.org/10.1016/S0268-0033(01)00118-8.
Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. 2005;13:316–25. https://doi.org/10.5435/00124635-200509000-00005.
Warden SJ, Burr DB, Brukner PD. Stress fractures: pathophysiology, epidemiology, and risk factors. Curr Osteoporos Rep. 2006;4:103–9. https://doi.org/10.1007/s11914-996-0029-y.
Chepurin D, Chamoli U, Diwan AD. Bony stress and its association with intervertebral disc degeneration in the lumbar spine: a systematic review of clinical and basic science studies. Glob Spine J. 2022;12(5):964–79. https://doi.org/10.1177/21925682211008837.
Plomp KA, Dobney K, Collard M. Spondylolysis and spinal adaptations for bipedalism: the overshoot hypothesis. Evol Med Public Health. 2020;2020(1):35–44. https://doi.org/10.1093/emph/eoaa003.
Thakar S, Sivaraju L, Aryan S, Mohan D, Sai Kiran NA, Hegde AS. Lumbar paraspinal muscle morphometry and its correlations with demographic and radiological factors in adult isthmic spondylolisthesis: a retrospective review of 120 surgically managed cases. J Neurosurg Spine. 2016;24(5):679–85. https://doi.org/10.3171/2015.9.SPINE15705.
Don AS, Robertson PA. Facet joint orientation in spondylolysis and isthmic spondylolisthesis. Clin Spine Surg. 2008;21(2):112–5. https://doi.org/10.1097/BSD.0b013e3180600902.
Kim MW, Lee KY, Lee S. Factors associated with the symptoms of young adults with L5 Spondylolysis. Asian Spine J. 2018;12(3):476–83. https://doi.org/10.4184/asj.2018.12.3.476.
Forrest MR, Hebert JJ, Scott BR, Dempsey AR. Modifying bowling kinematics in cricket pace bowlers with exercise-based injury prevention: a cluster-randomised controlled trial. J Sci Med Sport. 2020;23(12):1172–7. https://doi.org/10.1016/j.jsams.2020.06.014.
Ranson C, King M, Burnett A, Worthington P, Shine K. The effect of coaching intervention on elite fast bowling technique over a two year period. Sport Biomech. 2009;8(4):261–74. https://doi.org/10.1080/14763140903469908.
Hodges PW, Tucker K. Moving differently in pain: a new theory to explain the adaptation to pain. Pain. 2011;152(3):S90–8. https://doi.org/10.1016/j.pain.2010.10.020.
Sayers MGL, Bachem C, Schütz P, Taylor WR, List R, Lorenzetti S, Hosseini Nasab SH. The effect of elevating the heels on spinal kinematics and kinetics during the back squat in trained and novice weight trainers. J Sport Sci. 2020;38(9):1000–8. https://doi.org/10.1080/02640414.2020.1738675.
Glazier PS, Wheat JS. An integrated approach to the biomechanics and motor control of cricket fast bowling techniques. Sport Med. 2013;44(1):25–36. https://doi.org/10.1007/s40279-013-0098-x.
Seay JF, Van Emmerik REA, Hamill J. Trunk bend and twist coordination is affected by low back pain status during running. Eur J Sport Sci. 2014;14(6):563–8. https://doi.org/10.1080/17461391.2013.866167.
Papi E, Bull AM, McGregor AH. Alteration of movement patterns in low back pain assessed by statistical parametric map**. J Biomech. 2020;100:109597. https://doi.org/10.1016/j.jbiomech.2019.109597130.
Ranson CA, Burnett A, King M, Patel N, O’Sullivan PB. The relationship between bowling action classification and three-dimensional lower trunk motion in fast bowlers in cricket. J Sport Sci. 2008;26:267–76. https://doi.org/10.1080/02640410701501671.
Senington B, Lee RY, Williams JM. Are shoulder counter rotation and hip shoulder separation angle representative metrics of three-dimensional spinal kinematics in cricket fast bowling? J Sport Sci. 2018;36(15):1763–7. https://doi.org/10.1080/02640414.2017.1416734.
Al-Eisa E, Egan D, Deluzio K, Wassersug R. Effects of pelvic skeletal asymmetry on trunk movement: three-dimensional analysis in healthy individuals versus patients with mechanical low back pain. Spine. 2006;31(3):E71–9. https://doi.org/10.1097/01.brs.0000197665.93559.04.
Papi E, Bull AMJ, McGregor AH. Spinal segments do not move together predictably during daily activities. Gait Posture. 2019;67:277–83. https://doi.org/10.1016/j.gaitpost.2018.10.031.
Kiapour A, Terai T, Goel VJ, Nagamachi A, Sairyo K. Biomechanical effects of spinal flexibility and rigidity on lumbar spine loading: a finite element analysis study. EC Orthop. 2016;3:351–8.
Bogduk N. Clinical anatomy of the lumbar spine and sacrum. 4th ed. New York: Churchill Livingstone; 2005.
Mitchell B, Colson E, Chandramohan T. Lumbopelvic mechanics. Br J Sport Med. 2003;37(3):279–80. https://doi.org/10.1136/bjsm.37.3.279-a.
Ferdinands RE, Sinclair PJ, Stuelcken MC, Greene A. Rear leg kinematics and kinetics in cricket fast bowling. Sport Technol. 2014;7(1–2):52–61. https://doi.org/10.1080/19346182.2014.893352.
Olivier B, Stewart AV, Green AC, McKinon W. Cricket pace bowling: The trade-off between optimising knee angle for performance advantages v. injury prevention. S Afr J Sport Med. 2015;27(3):76–81. https://doi.org/10.7196/SAJSM.8111.
King MA, Worthington PJ, Ranson CA. Does maximising ball speed in cricket fast bowling necessitate higher ground reaction forces? J Sport Sci. 2016;34(8):707–12. https://doi.org/10.1080/02640414.2015.1069375.
Worthington P, King M, Ranson C. The influence of cricket fast bowlers’ front leg technique on peak ground reaction forces. J Sport Sci. 2013;31(4):434–41. https://doi.org/10.1080/02640414.2012.736628.
Greig M, Child B. Submaximal cricket fast bowling offers a disproportionate reduction in loading versus performance: an alternative workload intervention. J Sport Rehabil. 2020;29:483–7. https://doi.org/10.1123/jsr.2018-0266.
Senington B, Lee RY, Williams JM. Validity and reliability of innovative field measurements of tibial accelerations and spinal kinematics during cricket fast bowling. Med Biol Eng Comput. 2021;59(7–8):1475–84. https://doi.org/10.1007/s11517-021-02381-3.
Movahed M, Salavati M, Sheikhhoseini R, Arab AM, O’Sullivan K. Single leg landing kinematics in volleyball athletes: a comparison between athletes with and without active extension low back pain. J Bodyw Mov Ther. 2019;23(4):924–9. https://doi.org/10.1016/j.jbmt.2019.01.012.
Sutherlin MA, Colby Mangum L, Russell S, Saliba S, Hertel J, Hart JM. Landing stiffness between individuals with and without a history of low back pain. J Sport Rehabil. 2020;29:28–36. https://doi.org/10.1123/jsr.2017-0081.
Hetsroni I, Wiener Y, Ben-Sira D, Iacono AD, Marom N, van Stee M, Ayalon M. Symmetries in muscle torque and landing kinematics are associated with maintenance of sports participation at 5 to 10 years after ACL reconstruction in young men. Orthop J Sport Med. 2020;8(6):2325967120923267. https://doi.org/10.1177/2325967120923267.
Fong CM, Blackburn JT, Norcross MF, McGrath M, Padua D. Ankle-dorsiflexion range of motion and landing biomechanics. J Athl Train. 2011;46(1):5–10. https://doi.org/10.4085/1062-6050-46.1.5.
Mason-Mackay AR, Whatman C, Reid B. The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: a systematic review. J Sci Med Sport. 2017;20:451–8. https://doi.org/10.1016/j.jsams.2015.06.006.
Hamill J, Moses M, Seay J. Lower extremity joint stiffness in runners with low back pain. Res Sport Med. 2009;17(4):260–73. https://doi.org/10.1080/15438620903352057.
Pickering Rodriguez EC, Watsford ML, Bower RG. The relationship between lower body stiffness and injury incidence in female netballers. Sport Biomech. 2017;16(3):361–73. https://doi.org/10.1080/14763141.2017.1319970.
Zhang Y, Ma Y, Liu G. Lumbar spinal loading during bowling in cricket: a kinetic analysis using a musculoskeletal modelling approach. J Sport Sci. 2016;34(11):1030–5. https://doi.org/10.1080/02640414.2015.1086014.
Christophy M, Faruk Senan NA, Lotz JC, O’Reilly OM. A musculoskeletal model for the lumbar spine. Biomech Model Mechanobiol. 2012;11:19–34. https://doi.org/10.1007/s10237-011-0290-6152.
Felton PJ, Lister SL, Worthington PJ, King MA. Comparison of biomechanical characteristics between male and female elite fast bowlers. J Sport Sci. 2019;37(6):665–70. https://doi.org/10.1080/02640414.2018.1522700.
Márquez G, Alegre LM, Jaén D, Martin-Casado L, Aguado X. Sex differences in kinetic and neuromuscular control during jum** and landing. J Musculoskelet Neuronal Interact. 2017;17(1):409 PMID: 28250245 PMCID: PMC5383769.
Forrest MRL, Scott BR, Hebert JJ, Dempsey AR. Injury prevention strategies for adolescent cricket pace bowlers. Sport Med. 2018;48(11):2449–61. https://doi.org/10.1007/s40279-018-0981-6.
Forrest MRL, Hebert JJ, Scott BR, Dempsey AR. Exercise-based injury prevention for community-level adolescent cricket pace bowlers: a cluster-randomised controlled trial. J Sci Med Sport. 2020;23(5):475–80. https://doi.org/10.1016/j.jsams.2019.12.009.
Dennis RJ, Finch CF, Elliott BC, Farhart PJ. The reliability of musculoskeletal screening tests used in cricket. Phys Ther Sport. 2008;9(1):25–33. https://doi.org/10.1016/j.ptsp.2007.09.004.
Sahrmann S. Diagnosis and treatment of movement impairment syndromes. 1st ed. St. Louis: Mosby; 2001.
Chan EW, Hamid MS, Nadzalan AM, Hafiz E. Abdominal muscle activation: an EMG study of the Sahrmann five-level core stability test. Hong Kong Physiother J. 2020;40(02):89–97. https://doi.org/10.1142/S1013702520500080.
Dekart KQ. Test-re-test reliability of Sahrmann lower abdominal core stability test for DII baseball athletes. West Virginia University; 2014.
Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sport Med. 2006;36(3):189–98. https://doi.org/10.2165/00007256-200636030-00001.
Perrott MA, Pizzari T, Opar M, Cook J. Development of clinical rating criteria for tests of lumbopelvic stability. Rehabil Res Pract. 2012;2012. https://doi.org/10.1155/2012/803637.
Freke MD, Crossley K, Russell T, Sims KJ, Semciw A. Changes in knee and trunk alignment in people with hip pain and healthy controls when using a decline board during single-leg squat. J Sport Rehabil. 2019;29(7):886–96. https://doi.org/10.1123/jsr.2019-0097.
Kongsgaard M, Aagaard P, Roikjaer S, et al. Decline eccentric squats increases patellar tendon loading compared to standard eccentric squats. Clin Biomech. 2006;21(7):748–54. https://doi.org/10.1016/j.clinbiomech.2006.03.004.
Zwerver J, Bredeweg SW, Hof AL, Purdam C. Biomechanical analysis of the single-leg decline squat. Br J Sport Med. 2007;41(4):264–8. https://doi.org/10.1136/bjsm.2006.032482.
Grimaldi A. Assessing lateral stability of the hip and pelvis. Man Ther. 2011;16(1):26–32. https://doi.org/10.1016/j.math.2010.08.005.
O’Sullivan PB, Burnett A, Floyd AN, Gadsdon K, Logiudice J, Miller D, Quirke H. Lumbar repositioning deficit in a specific low back pain population. Spine. 2003;28(10):1074–9. https://doi.org/10.1097/01.BRS.0000061990.56113.6F.
Meakin JR, Aspden RM. Modeling the effect of variation in sagittal curvature on the force required to produce a follower load in the lumbar spine. J Mech Med Biol. 2012;12:1–10. https://doi.org/10.1142/S0219519412004466.
Meakin JR, Fulford J, Seymour R, Welsman JR, Knapp KM. The relationship between sagittal curvature and extensor muscle volume in the lumbar spine. J Anat. 2013;222:608–14. https://doi.org/10.1111/joa.12047.
Acknowledgements
The authors thank Franco Impellizzeri for his contributions to the manuscript.
Funding
No sources of funding were used to assist in the preparation of this article.
Author information
Authors and Affiliations
Contributions
PF, MW and AD conceived the idea for the article. PF, MW and AD were involved in design and planning of the systematic review. PF and DB completed the screening and extraction of all data within this manuscript. PF wrote the first draft of the manuscript and all versions thereafter. All authors critically revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Presents a detailed search strategy for each database.
Additional file 2.
Presents detailed and defined criteria for the rating of studies using the Quality in Prognostic Studies (QUIPS) tool.
Additional file 3.
Presents detailed information regarding individual Risk of Bias assessments for each of the Quality in Prognostic Studies (QUIPS) domains of each included study.
Additional file 4.
Presents definitions for intrinsic variables that have been associated with low back pain and lumbar spine injury in fast bowlers.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farhart, P., Beakley, D., Diwan, A. et al. Intrinsic variables associated with low back pain and lumbar spine injury in fast bowlers in cricket: a systematic review. BMC Sports Sci Med Rehabil 15, 114 (2023). https://doi.org/10.1186/s13102-023-00732-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-023-00732-1