Abstract
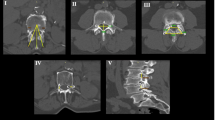
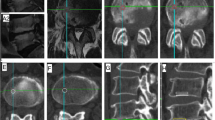
The lesion of the lumbar endplate is sometimes identified in the vertebrae of children and adolescents. The purpose of this study is to compare between skeletal maturity and chronological age. The second purpose of this study is to clarify the lesions of the lumbar endplate based on the maturation of the lumbar vertebral body. Six hundred and thirty-two (485 men and 147 women) consecutive patients were included. The mean age at the first medical examination was 13.8 years. Their skeletal maturity was evaluated based on the appearances of the secondary ossification center of L3. The area of the endplate lesions was classified into five types. The apophyseal stage was observed from 10 years old to 18 years old, and the apophyseal stage was shown the peak at 14 years old. The appearance of the apophyseal ring was observed earlier in female patients than in male patients. For the concave type, the lesion at upper level vertebra was more prevalent. The anterior and middle type of the lesion at upper level vertebra was more prevalent. For the posterior type, the lesion of the inferior rim of L4 and the lesion of the rim of L5 were more prevalent. This study emerged after comparing skeletal maturity based on the maturation of the lumbar vertebral body with the chronological age of a large number of patients and examining the lesions of the lumbar endplate based on the stage of maturation of the lumbar vertebral body.





Similar content being viewed by others
References
Ahlqwist A, Hagman M, Kjellby-Wendt G, Beckung E (2008) Physical therapy treatment of back complaints on children and adolescents. Spine (1976) 33:E721–E727
Edelson JG, Nathan H (1988) Stages in the natural history of the vertebral end-plates. Spine 13:21–26
Higashino K, Hamasaki T, Kim JH, Okada M, Yoon ST, Boden SD et al (2010) Do the adjacent level intervertebral discs degenerate after a lumbar spinal fusion? An experimental study using a rabbit model. Spine (Phila Pa 1976) 35:E1144–E1152
Higashino K, Sairyo K, Katoh S, Takao S, Kosaka H, Yasui N (2012) Long-term outcomes of lumbar posterior apophyseal end-plate lesions in children and adolescents. J Bone Joint Surg Am 94:e74
Higashino K, Sairyo K, Sakamaki T, Komatsubara S, Yukata K, Hibino N et al (2007) Vertebral rounding deformity in pediatric spondylolisthesis occurs due to deficient of endochondral ossification of the growth plate: radiological, histological and immunohistochemical analysis of a rat spondylolisthesis model. Spine (Phila Pa 1976) 32:2839–2845
Ikata T, Miyake R, Katoh S, Morita T, Murase M (1996) Pathogenesis of sports-related spondylolisthesis in adolescents. Radiographic and magnetic resonance imaging study. Am J Sports Med 24:94–98
Ikata T, Morita T, Katoh S, Tachibana K, Maoka H (1995) Lesions of the lumbar posterior end plate in children and adolescents. An MRI study. J Bone Joint Surg Br 77:951–955
Laredo JD, Bard M, Chretien J, Kahn MF (1986) Lumbar posterior marginal intra-osseous cartilaginous node. Skeletal Radiol 15:201–208
Sairyo K, Goel VK, Masuda A, Vishnubhotla S, Faizan A, Biyani A et al (2006) Three-dimensional finite element analysis of the pediatric lumbar spine. Part I: pathomechanism of apophyseal bony ring fracture. Eur Spine J 15:923–929
Sairyo K, Katoh S, Ikata T, Fujii K, Kajiura K, Goel VK (2001) Development of spondylolytic olisthesis in adolescents. Spine J 1:171–175
Sairyo K, Kawamura T, Mase Y, Hada Y, Sakai T, Hasebe K et al (2013) Jack-knife stretching promotes flexibility of tight hamstrings after 4 weeks: a pilot study. Eur J Orthop Surg Traumatol 23:657–663
Siffert RS (1981) Classification of the osteochondroses. Clin Orthop Relat Res 158:10–18
Takata K, Inoue S, Takahashi K, Ohtsuka Y (1988) Fracture of the posterior margin of a lumbar vertebral body. J Bone Joint Surg Am 70(4):589–94
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
For all authors, there is no conflict of interest in this study.
Rights and permissions
About this article
Cite this article
Uraoka, H., Higashino, K., Morimoto, M. et al. Study of lesions of the lumbar endplate based on the stage of maturation of the lumbar vertebral body: the relationship between skeletal maturity and chronological age. Eur J Orthop Surg Traumatol 28, 183–187 (2018). https://doi.org/10.1007/s00590-017-2032-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-017-2032-7