Abstract
Objective
To investigate the therapeutic efficacy of total flavonoids of Rhizoma Drynariae (TFRD) in conjunction with a calcium phosphate/collagen scaffold for the repair of cranial defects in rats.
Methods
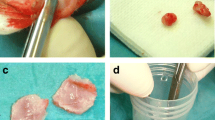
The subjects, rats, were segregated into four groups: Control, TFRD, Scaffold, and TFRD + Scaffold. Cranial critical bone defects, 5 mm in diameter, were artificially induced through precise drilling. Post-surgery, at intervals of 2, 4, and 8 weeks, micro-CT scans were conducted to evaluate the progress of skull repair. Hematoxylin–eosin and Masson staining techniques were applied to discern morphological disparities, and immunohistochemical staining was utilized to ascertain the expression levels of local osteogenic active factors, such as bone morphogenetic protein 2 (BMP-2) and osteocalcin (OCN).
Results
Upon examination at the 8-week mark, cranial defects in the Scaffold and TFRD + Scaffold cohorts manifested significant repair, with the latter group displaying only negligible foramina. Micro-CT examination unveiled relative to its counterparts, and the TFRD + Scaffold groups exhibited marked bone regeneration at the 4- and 8-week intervals. Notably, the TFRD + Scaffold group exhibited substantial bone defect repair compared to the TFRD and Scaffold groups throughout the entire observation period, while histomorphological assessment demonstrated a significantly higher collagen fiber content than the other groups after 2 weeks. Immunohistochemical analysis further substantiated that the TFRD + Scaffold had augmented expression of BMP-2 at 2, 4 weeks and OCN at 2 weeks relative to other groups.
Conclusions
The synergistic application of TFRD and calcium phosphate/collagen scaffold has been shown to enhance bone mineralization, bone plasticity, and bone histomorphology especially during initial osteogenesis phases.
Similar content being viewed by others
Bone defect, a multifaceted pathology prevalent in medical science, can emanate from a multitude of sources such as trauma, inflammation of bone tissue, tumor excision, or congenital malformations [1, 2]. This condition profoundly affects patients’ quality of life, necessitating comprehensive treatment approaches. Presently, bone grafting, which can be either autogenous or allogeneic (originating from a different individual), stands as the conventional method for addressing bone anomalies [3]. However, both techniques present unique challenges. Allograft transplantation may encounter rejection and obstacles in revascularization, while autogenous bone transplantation may give rise to pain at the donor site and complexities in achieving congruence with the recipient bone structure [4].
Calcium phosphate (CP), as the primary inorganic constituent, along with collagen and water as the principal organic components, constitutes the structural matrix of bone tissue [5]. CP and collagen scaffolds, being the two most prominent components, have been shown exceptional biocompatibility, osteoconductivity, and osteoinductivity for bone critical-size defect repair [6, 7]. Critical-size defect (CSD) is the smallest in diameter bone defect that does not heal spontaneously [8]. The research conducted by Kim et al. substantiates that hydroxyapatite demonstrates notable osteocompatibility, effectively facilitating new bone ingrowth [9]. Furthermore, the application of medical-grade polycaprolactone/tricalcium phosphate (mPCL-TCP) combined with collagen scaffold and rhBMP-2 has been observed to enhance bone quality significantly in the treatment of critical bone defects [10]. Additionally, the study by Chatzipetros E et al. reveals that the incorporation of nano-hydroxyapatite/chitosan scaffolds plays a pivotal role in new bone formation in rat calvarial CSD, as evidenced by histomorphometric analysis and cone beam computed tomography (CBCT) measurements [8, 11].
Nevertheless, when bone defects reach critical-size, patients may be confronted with extended recovery durations, subsequently amplifying the risk of treatment-associated complications such as infection and bone malformation [12, 13]. Future inquiries must concentrate on expediting bone regeneration, curtailing the temporal scope of treatment, and obviating the emergence of complications.
Traditional Chinese Medicine (TCM) offers an expansive repository of therapeutic modalities, amenable to enhancement through integration with contemporary medical doctrines [14]. Such fusion may foster the inception of novel solutions and strategies for recalcitrant clinical conundrums. Additionally, this amalgamation aids in deciphering the underlying mechanisms by which TCM manifests its therapeutic impact, thereby consolidating a scientific framework for its clinical translation [15,5c). Collagen fiber content and neonatal bone tissue decreased, and mature bone tissue increased as time progressed. Consequently, the Masson staining underscored the propitious role of TFRD in augmenting early bone regeneration, and concurrently highlighted that the TFRD + Scaffold conglomerate boasted more advanced bone tissues within the bone defect location.
Immunohistochemical evaluation
The immunohistochemical (IHC) analysis probed the expression of OCN and BMP-2 antibodies at the cranial defect perimeters. OCN-expressing osteoblasts and BMP-2, which is discernible in pluripotent mesenchymal cells, osteoblasts, bone matrices, and associated tissues, both were marked by a brown or yellowish-brown cytoplasmic coloration (Fig. 6A and B). Our results clearly showed that both OCN and BMP-2 have high expression in the TFRD treated groups compared to the control group at the two-week juncture. Furthermore, The TFRD + Scaffold group demonstrated significant elevations in BMP-2 and OCN levels in comparison with the Scaffold alone group from two weeks to eight weeks (Fig. 6C and D). These observations lend credence to the proposition that TFRD catalyzes the release of osteogenesis-associated proteins, partially through the potentiation of the BMP-smad signaling conduit in osteoblasts, thereby fortifying osteogenesis. This further insinuates potential osteogenic synergism attributable to TFRD.
Representative images of IHC staining A IHC staining of OCN at the cranial defect perimeters. B IHC staining of BMP-2 at the cranial defect perimeters. Images were captured at 10× microscopy, with a scale bar shown at 100 μm. C Bar charts show OCN positive area (%) calculated by densitometry of IHC images. D Bar charts show BMP-2 positive area (%) calculated by densitometry of IHC images. TFRD versus control group and TFRD + Scaffold versus Scaffold, (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001)
Discussion
Despite the commendable success rate achieved with calcium phosphate/collagen scaffolds in clinical applications, the quest for expedited bone regeneration and abbreviated treatment durations persist as pivotal frontiers in osteogenesis research [24]. In this context, Traditional Chinese Medicine (TCM) presents a compelling adjunct to surgical interventions. Our present investigation elucidated that the bone healing proficiency of the TFRD cohort markedly surpassed that of the control group. Notably, this enhancement in bone regenerative capability was conspicuously amplified when TFRD was amalgamated with scaffolding substrates, especially during the incipient stages of osteogenesis.
A plethora of empirical endeavors have underscored the salutary influences of both TFRD and calcium phosphate/collagen scaffold in bolstering bone reparative capabilities. To meticulously discern the potential synergistic ramifications of these two entities, we meticulously curated two-by-two comparative matrices within our experimental blueprint: juxtaposing the Control group against the TFRD cohort, and the Scaffold assembly against the TFRD + Scaffold ensemble. Subsequent evaluations spanned imaging diagnostics, histological analyses, and immunohistochemical assessments.
Guo Ying et al. elucidated that TFRD facilitates the osteogenic differentiation of rat bone marrow stem cells (BMSCs), amplifying the expression of pivotal factors such as β-catenin, lymphoid enhancer factor I (LEF-l), and cyclin D mRNA during the nascent phases of differentiation. Intriguingly, TFRD attenuates the expression of these factors as differentiation matures. This observation underscores the hypothesis that TFRD’s primary contribution to osteoblast differentiation predominantly occurs during the early differentiation phases [25]. Jiang Ziwei et al. delved into the temporal effects of TFRD on osteogenesis efficacy, utilizing tibia distraction osteogenesis in rats as a model system. The empirical findings elucidated that the group treated with the flavonoids throughout the entire experimental period exhibited notably superior results in terms of X-ray scores and bone mineral density when juxtaposed with groups receiving interventions during the distraction phase alone or both the distraction and mineralization phases. In summation, an early and consistent administration of TFRD can significantly augment the quality of bone formation in the distraction osteogenic region of rats [26]. Our results are in line with the literatures. The micro-CT BMD analysis showed that the TFRD + Scaffold assembly showcased a superior trajectory and velocity of bone density amplification in contrast to the sole scaffold group during the initial two and four-week periods, which demonstrated TFRD may have favorable consequences concerning precocious osteogenesis.
Collagen fibers within the bone tissue matrix are crucial for osteoblast maturation and matrix mineralization. Type I collagen, a primary component of the bone matrix, facilitates the expression of osteoadhesins, osteocalcin, and bridging proteins, thereby enhancing matrix mineralization during the mineralization phase [27]. In vivo studies at the 2-week mark revealed that the collagen content in the TFRD + Scaffold group was significantly higher than that in the Scaffold group alone. However, there was a gradual decrease in collagen content in the TFRD + Scaffold group at weeks 4 and 8. These observations indicate that TFRD integrated with calcium phosphate/collagen scaffolds may induce early osteogenesis and expedite matrix mineralization.
The principal exhibition of TCM’s facilitation in osteogenic repair can be elucidated in the following dimensions: Initially, promoting blood circulation to dredge collaterals, thereby the prevention and elimination of blood clots mitigate aseptic inflammation and trauma to soft tissues [28]. Subsequently, the enhancement of blood circulation, vascular wall permeability, ion exchange, local deposition of trace elements such as zinc, iron, copper, manganese, and calcium salts occurs [29]. Further, there is stimulation of local collagen synthesis at the fracture terminus within the bone matrix, and the secretion and synthesis of bone growth factors such as BMPs, VEGF and OCN.
The therapeutic efficacy of TFRD in fracture recuperation and osteoporosis management is elucidated through its intricate modulation of two distinct molecular signaling pathways. Firstly, TFRD facilitates the activation of osteogenesis-associated signaling cascades within bone marrow stem cells (BMSCs) and osteoblasts [30]. Notably, pathways such as Wnt/β-catenin, MAPK, and Smad are intricately linked to bone synthesis [31]. Conversely, TFRD mitigates osteoporosis by impeding bone resorption and attenuating bone loss. The critical pathways orchestrating this inhibitory action on bone resorption encompass CTSK and OPG/RANKL/RANK [18, 32]. It is noteworthy that while the majority of therapeutic agents typically target either bone resorption or synthesis singularly, TFRD exhibits a dual modulatory influence on both these processes [33, 34].
As an integral component of the BMPs family, BMP-2 assumes an osteogenic mantle by orchestrating the transcription of genes germane to osteogenesis and by catalyzing the Smads protein signaling mechanism. [35] BMP-2 exerts considerable osteoinductive activity, signifying its capability to directly increase cell augment cellular calcification and instigate new bone formation in conjunction with osteoblast maturation [15, 20]. Data from our investigation delineate that the expression of BMP-2 across all experimental cohorts reached zenithal levels two weeks post-gavage, subsequently waning thereafter. However, consistently across all evaluated intervals, the TFRD + Scaffold group exhibited superior BMP-2 expression compared to the Scaffold group, and the TFRD group surpassed the Control group. These findings are congruent with extant literature, illustrating that TFRD elevates BMP-2 expression, thus favoring bone production and differentiation.
Osteoblasts proceed through four sequential stages during bone formation: proliferation, extracellular matrix maturation, extracellular matrix mineralization, and apoptosis. [36] Accordingly, the investigative approach to augment the pace of induced bone healing encompasses the stimulation of osteoblast proliferation, differentiation, mineralization, and the release of augmented osteogenic-related proteins. Osteocalcin (OCN), a ubiquitous non-collagenous protein in bone tissue synthesized by osteoblasts and marked by a swift turnover rate, functions as a precise and unerring indicator of osteoblast activity [37]. The results manifested that the group receiving scaffold combined with TFRD gavage displayed increased bone growth and mineralization in both the central and peripheral regions of the bone defect area, culminating in the upregulation of osteogenic-associated factors such as OCN. The escalated OCN positive expression in the TFRD-Scaffold group surpassed that achieved by scaffold alone, corroborating the enhancement of osteoblasts’ bone formation functionality and the remodeling process facilitated by TFRD.
Through rigorous animal-based experimentation, our study culminates in the conclusive assertion that the confluence of TFRD and calcium phosphate/collagen scaffolds exudes a distinct synergistic efficacy. TFRD amplifies bone repair capabilities, primarily by galvanizing the expression of osteogenesis-associated proteins like BMP-2 and OCN, especially during the nascent stages of bone regeneration. This intricate tapestry of actions provides clarity on the synergistic potential when TFRD is integrated with calcium phosphate/collagen scaffolds. Such findings bolster the proposition for TFRD’s incorporation as a potent herbal therapeutic for addressing bone defects.