Abstract
Diabetes mellitus is a significant global public health challenge, with a rising prevalence and associated morbidity and mortality. Cell therapy has evolved over time and holds great potential in diabetes treatment. In the present review, we discussed the recent progresses in cell-based therapies for diabetes that provides an overview of islet and stem cell transplantation technologies used in clinical settings, highlighting their strengths and limitations. We also discussed immunomodulatory strategies employed in cell therapies. Therefore, this review highlights key progresses that pave the way to design transformative treatments to improve the life quality among diabetic patients.
Similar content being viewed by others
Background
Diabetes mellitus poses a formidable global public health challenge due to its rapid growing prevalence and associated morbidity, disability, and mortality [1]. According to the International Diabetes Federation, over 537 million adults aged 20–79 had diabetes worldwide in 2021 that is expected to rise to around 783 million cases by 2045 [2]. Obesity, unhealthy diets, physical inactivity as well as genetic and epigenetic predispositions are important risk factors of diabetes [3,4,5]. Diabetes is typically classified into type 1 diabetes mellitus (T1DM), gestational diabetes mellitus (GDM), and type 2 diabetes mellitus (T2DM) [2]. T1DM primarily arises from autoimmune-related damage of insulin-secreting beta cells, resulting in severe hyperglycemia and ketoacidosis [6]. In contrast, T2DM generally has a more gradual onset characterized by insulin resistance along with diminished compensatory insulin secretion from pancreatic beta cell dysfunction [7]. Diabetes is associated with macrovascular complications such as heart disease and stroke, as well as microvascular issues in eyes, kidneys, and nervous system [8]. Cancer is also a leading cause of diabetes-related death, and dementia-associated mortality has risen in recent decades [9,10,11,12]. Cell therapy involves transferring autologous or allogenic cellular material into patients [13]. The global market size of cell therapy is estimated to grow from $9.5 billion in 2021 to $23 billion by 2028 [14]. It combines stem and non-stem cell therapies consisting of unicellular or multicellular preparations. Cell therapies typically use autologous or allogenic cells via injection and infusion [15]. In the present review, we discussed the recent advances in cell-based therapy of diabetes, from foundational islet transplantation to regenerative strategies to highlight key developments that improve the effective treatments for diabetic patients.
Cell replacement therapy for diabetes
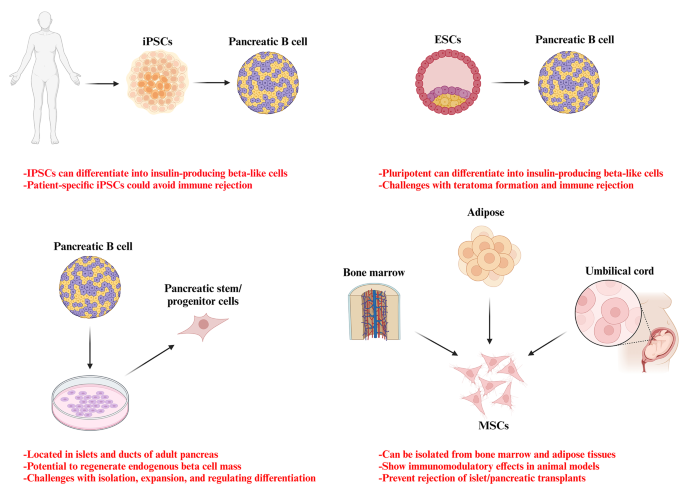
Pancreatic transplantation was firstly used in 1966 to treat type 1 diabetes using whole organ transplants. During the 1970s–80s, segmental pancreatic grafts were combined with techniques to divert digestive secretions away from transplanted cells. Three main techniques emerged; simultaneous pancreas-kidney transplants, pancreas transplants following kidney transplants, and pancreatic transplants. International collaboration on tracking outcomes began in 1980 with the formation of several pancreatic transplant registries and associations. However, whole organ transplantation was faced with several challenges including organ rejection, vascular complications, limited organ availability, and the effects of lifelong immunosuppression [16, 17]. Islet cell transplantation was explored as an alternative, however isolating and transplanting pancreatic islets proved difficult due to donor availability, rejection, and immunosuppression side effects. Recent research has focused on stem cell sources that could reconstitute immune tolerance and preserve beta cell function such as mesenchymal stem cells, bone marrow cells, and embryonic stem cells [18]. A novel stem cell therapy called VX-880 was developed using proprietary technology to grow insulin-producing beta cells from allogeneic stem cells. Clinical trials began in 2021 after FDA approval to deliver the cells intrahepatically under immune suppression. A second approach called VX-264 encapsulates the same cells, avoiding immunosuppression but requiring surgical implantation [17]. In 2023, FDA approved the first allogeneic pancreatic islet cell therapy called Lantidra for adults with type 1 diabetes experiencing severe hypoglycemia. Approval was based on two studies where 21–30% of participants no longer required insulin one year post-treatment, with benefits lasting over five years in some cases. However, this treatment have mild and serious adverse events that are associated with treatment dose and the methods of islet cell infusion [19, 20].
Emerging strategies for cell delivery via microencapsulation and biological devices in clinical trials
Alginate capsules as cell delivery systems
A seminal investigation conducted in 1994 demonstrated the successful transplantation of alginate-encapsulated islets into the peritoneum of kidney transplant patients who were receiving immunosuppression therapy. Remarkably, these patients achieved insulin independence for up to nine months [21]. However, subsequent trials conducted without immunosuppression yielded inconsistent outcomes. In a study conducted in 2006, islets were encapsulated in triple-layer alginate capsules and implanted intraperitoneally in type 1 diabetes (T1D) patients. There was a positive correlation between the encapsulation and insulin production that reduced exogenous insulin requirements during one year. Despite this progress, the entry of cytokines remained a potential concern [22]. Another study employed the single-layer barium-alginate capsules that sustained insulin production for up to 2.5 years [23]. It has been reported that the microneedle, comprising a calcium alginate frame with polydopamine-coated poly-lactic-co-glycolic acid microspheres encapsulating insulin, enables light-triggered insulin release. Microneedle provided a suitable insulin dose to maintain blood glucose levels in line with daily fluctuations. These results established the efficacy and safety of the developed microneedle for diabetes treatment [24]. Another therapeutic approach explored the encapsulation of pancreatic islets with mesenchymal stem cells (MSCs) and decellularized pancreatic extracellular matrix (ECM). ECM derived from the pancreas supported islet cell growth and maintenance to enhance insulin expression [25]. Sodium alginate and hyaluronic acid were incorporated due to their roles in collagen production, wound healing, and physical crosslinking. The 3D porous membranes allowed optimal water and oxygen transfer while diverting excess exudate from diabetic wounds. Hydrogel accelerated re-epithelization, while decreased inflammation, indicating potential as the diabetic wound dressings [26]. Additionally, the incorporation of specific ECM components, such as collagen IV and RGD, into alginate-based microcapsules significantly improved the survival, insulin secretion, and longevity of microencapsulated islets [27].
Encaptra® device from ViaCyte
In contrast to microencapsulation techniques, ViaCyte developed a semipermeable pouch method named Encaptra, which contains pancreatic precursor cells derived from the embryonic stem cells [28]. In the initial trial conducted in 2014, the “VC-01” device was implanted in T1D individuals without the use of immunosuppression [29]. The trial confirmed the safety of the device; however, the occurrence of hypoxia induced cellular necrosis [30]. The device was modified as “VC-02” with larger pores, and two trials (NCT03162926, NCT03163511) demonstrated promising outcomes, including increased fasting C-peptide levels and a 20% reduction in insulin requirements during one year in the majority of participants [31]. In order to eliminate the necessity for immunosuppressants, ViaCyte collaborated with Gore to develop an expanded polytetrafluoroethylene (ePTFE) device with both immuno-isolating and pro-angiogenic properties [32]. This device (NCT04678557) aimed to prevent immune cell attachment and T-cell activation [33]. Additionally, ViaCyte is exploring the integration of CRISPR technology to modify stem cells, specifically by eliminating β2-microglobulin expression and PD-L1 up regulation. It is hypothesized that these genetic modifications will further hinder immune cell attachment and T-cell activation [30, 34].
Semipermeable device from Semma therapeutics
Semma Therapeutics, which has been acquired by Vertex, pioneered the utilization of differentiated stem cell-derived islet cell clusters in clinical trials. Semma houses these cells between two semipermeable polyvinylidene fluoride membranes and is designed for subcutaneous implantation (NCT04786262) [31, 35]. Vertex reported a significant breakthrough by infusing differentiated beta cells via the portal vein in a participant who was receiving immunosuppressants. This approach led to substantial C-peptide production and improved glycemic control during 90 days [36].
βAir device from Beta O2
Beta O2’s innovative βAir device utilizes an alginate-PTFE membrane complex to encapsulate islets, providing partial immunoisolation while ensuring a continuous supply of oxygen, which is crucial for optimal islet function [37, 38]. The βAir device that was seeded with human islets was subcutaneously implanted in T1D individuals (NCT02064309). Although, low insulin levels were produced for up to eight weeks, there was not any reduction in the required exogenous insulin [37]. While, increasing the number of islets could potentially enhance their function, it is important to note that the continuous reliance on oxygen poses a risk of infection, despite efforts to optimize the survival of encapsulated islets [39, 40].
Cell pouch™ device from Sernova
Sernova has developed the Cell Pouch device, which offers pre-vascularized polypropylene chambers for islet transplantation without the need for immunoprotection. The device consists of multiple cylindrical chambers that are prefilled with PTFE plugs, which are then removed after implantation to create the empty space [41]. In a 2012 trial (NCT01652911), islets were placed in the vascularized pouches of three recipients who were also receiving immunosuppression that resulted in a transient increase in C-peptide levels [41]. In a 2018 trial (NCT03513939), immunosuppression was administered after implantation and islet introduction. This trial reported sustained C-peptide production for up to nine months in two recipients, along with improved glycemic control [42]. Regarding the limitations of immunosuppression, Sernova is exploring the possibility of encapsulating islets in hydrogel as an alternative approach [43].
Shielded living therapeutics™ from Sigilon Therapeutics
Sigilon has developed the Shielded Living Therapeutics sphere, which consists of cell clusters enclosed within an alginate-TMTD coating [44]. Preclinical studies demonstrated that murine islet transplants encapsulated within these spheres maintained normoglycemia for a period of six months [45]. In a 2020 trial conducted for hemophilia (NCT04541628), the spheres were evaluated for their ability to express Factor VIII [46]. However, the trial was paused due to the development of antibodies in the third recipient receiving the highest cell doses. While, preclinical studies have shown promising efficacy, there are safety concerns regarding the TMTD coating that need to be addressed before these spheres can be used for human islet transplantation as a treatment for diabetes [31]. Emerging technologies have been investigated in clinical trials for delivering insulin-producing islets or stem cell-derived beta cells via microencapsulation or use of implantable biological devices (Table 1). Optimizing encapsulation and develo** alternative implantable devices moves the field toward delivering safe and effective islet replacement without chronic immunosuppression dependency that represented an important new frontier for the cell-based treatment of diabetes. However, continued refining will be required to fully realize this promising vision and using these preclinical concepts in clinic.
Immunoengineering strategies: biomaterials for modulating immune responses
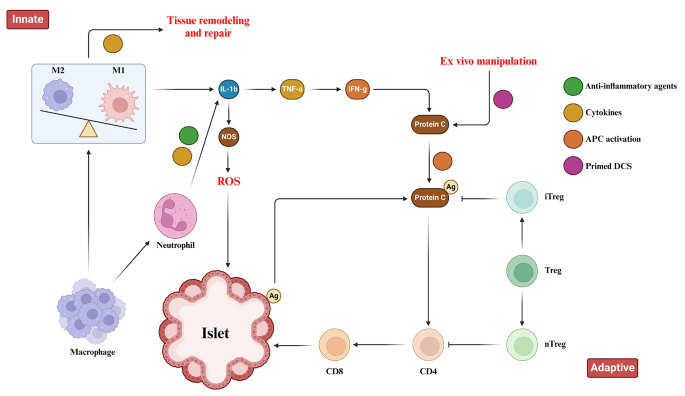
Islet encapsulation aims to prevent immune responses toward transplant antigens. However, foreign body response (FBR) against biomaterials induces inflammation around encapsulated islets that obstructs oxygen/nutrient access and causes graft failure [31]. Extensive research revealed biomaterial properties profoundly influence FBR severity, with high purity/biocompatibility moderating inflammation [47]. Deeper understanding of biomaterial immunobiology enabled develo** immune-modulating constructs to steer host interactions. By altering topology/chemistry to hinder nonspecific binding and cell adhesion, these “immune-evasive biomaterials” intended to attenuate xenograft rejection at inception [44]. Both innate and adaptive immune responses have crucial roles in the context of pancreatic islet transplantation. These responses encompass the activation of tissue macrophages and neutrophils following injury, leading to the release of inflammatory cytokines that subsequently activate antigen-presenting cells (APCs), CD8 + T cells, CD4 + T cells, and cytotoxic T lymphocytes (Fig. 1). Zwitterionic polymers conferred anti-fouling attributes but crosslinking limitations constrained their application [99]. Research on vascularization of islets via additive manufacturing techniques has primarily focused on the fundamental discoveries. In one study, engineered pseudo islets (EPIs) were created by combining the mouse insulin-secreting beta cells with rat heart microvascular endothelial cells. EPIs demonstrated extensive outgrowth of capillaries into the surrounding matrix. Although, EPIs containing both cell types that underwent capillarization maintained viability and function over time in culture, non-vascularized EPIs lacking endothelial cells could not sustain viability or functionality long-term. This supported the potential for inducing angiogenesis within bioengineered islet constructs. Future work may combine patient-specific stem cell-derived human beta cells with endothelial cells using this approach to promote long-term graft survival for treating type 1 diabetes [98]. While, large-scale 3D printed vascularized structures are currently limited for the islet transplantation, advancements in leveraging additive manufacturing for the optimization vascularization conditions through the pore sizes and material choices, may facilitate translation to β-cell therapy in type 1 diabetes.
Precision placement of cells and matrix for enhanced control
Beyond distributing biomaterials, additive manufacturing enables micro-level cell and protein control. For islet transplantation, optimal cellular distribution and supportive extracellular matrix niche reduce rapid dysfunction and apoptosis [100,101,102]. Traditional techniques heterogeneously load cells after fabrication or struggle with incomplete encapsulation [103, 104]. Bioprinting allows in situ encapsulation and printing of multiple cell types and matrix components while dictating 3D placement and dimensions [105, 106]. Islet transplant research prints hydrogel-encapsulated clusters surrounded by supportive cells and doped with immune modulators to improve the transplant environment [107]. Progress in bioprinting offers consistency and defines physical/chemical graft properties beyond traditional fabrication.
Achieving controlled integration of therapeutic agents for enhanced efficacy
In addition to the cell and matrix placement, additive manufacturing enables precision therapeutic integration. Incorporating therapeutics aims to recapitulate the in vivo environment through angiogenesis, islet health promotion, and immunomodulation [67, 108]. Growth factors promote vessel formation and insulin secretion while decrease apoptosis [108,109,110,111]. Local immunomodulators regulate the immune system in a specific site of the body. They decrease inflammation and promote the successful integration of transplanted cells or tissues by minimizing the need for widespread immune suppression in whole body [67]. Traditional homogeneous delivery methods restrict the ability to customize the spatial distribution of substances and pose a risk of harmful effects on transplants or hosts [112]. The use of discreet gradients in bioprinting can offer precise physiological signals. By combining traditional drug release methods with AM, it becomes possible to create tissues that exhibit distinct therapeutic localization. Bioprinted composites have the ability to release factors with gradients throughout the entire construct that enables a more comprehensive and targeted approach in tissue engineering [112,113,114].
Cell based gene therapy
Gene therapy holds great promise for diabetes management, offering innovative approaches to deliver and manipulate the insulin gene in various tissues. Viral methods, such as lentivirus, adenovirus, and adeno-associated virus (AAV), along with non-viral techniques like liposomes and naked DNA, have been utilized to deliver the insulin gene to target tissues [115]. This section aims to provide an overview of important studies in the field of gene therapy for diabetes management, emphasizing advancements in insulin gene delivery and manipulation (Table 3).
Enteroendocrine K-cells and pancreatic β-cells
Enteroendocrine K-cells in the intestines and pancreatic β-cells share similarities in their production of glucose-dependent insulinotropic polypeptide (GIP) and their regulatory mechanisms. Understanding these similarities offers insights into T2D management and improving glucose homeostasis. However, attempts to reverse diabetes effectively through K-cell transplantation have been unsuccessful. Nevertheless, research on gene editing techniques has shown promising results in management of the diabetes mellitus [116, 117]. AAV vectors have been employed to co-express insulin and glucokinase genes in skeletal muscles, demonstrating long-term effectiveness in achieving normo-glycemia without exogenous insulin [118, 119].
Gene editing techniques
Gene editing techniques using AAV vectors effectively improved normo-glycemia in animal models. Co-expression of insulin and glucokinase in transgenic mice increased glucose absorption and regulated insulin production. Duodenal homeobox 1 (PDX1) gene transfer via AAV2 in a humanized liver mouse model also led to insulin secretion and glycemic control [153, 154]. Xenotransplantation using gene-edited porcine islets remains an exciting avenue of research given advances to improve engraftment and reduce immunogenicity in preclinical studies [155]. Novel approaches continue to emerge as well, such as decellularization techniques, 3D bioprinting of tissue constructs, and creating interspecies chimeras. Rapid evolution of cell-based therapies across both academic and commercial sectors is promising to restore normoglycemic control in diabetic cases. Refinement of existing methods and development of new strategies hold potential to perform a safe and effective cell replacement without reliance on systemic immunosuppression. Stem cell and regenerative therapies may ultimately manage diabetes through restored endogenous insulin production [156]. Recently a meta analysis evaluated the safety and efficacy of MSC-based therapy for diabetes in humans. This comprehensive analysis was conducted on 262 patients across six trials that met the inclusion criteria within the last five years. The results reveal that treatment with MSCs significantly reduced the dosage of anti-diabetic drugs over a 12-months. Following treatment, HbAc1 levels decreased by an average of 32%, fasting blood glucose levels decreased by an average of 45%, and C-peptide levels showed a decrease of 38% in two trials and an increase of 36% in four trials. Notably, no severe adverse events were reported across all trials. Therefore, it can be concluded that MSC therapy for type 2 diabetes is safe and effective [157].
Advances in islet transplantation and stem cell-derived Beta cells
Limited number of the islet transplantation donors highlights the importance of cell therapy in diabetes. Although, higher islet numbers from multiple donors increase the success, limited pancreas availability restricts widespread use [158]. Using multiple donors also increases rejection risk, while isolation of the islets can cause tissue damage [159]. To overcome these challenges, researchers have explored the differentiation of stem cells into beta cells in vitro to generate an unlimited supply of insulin-producing cells with standardized and characterized products. Genetic engineering techniques have also been investigated to confer advantages such as stress resistance or immune evasion [158]. ViaCyte has developed a stem cell-derived pancreatic progenitor called PEC-01, which has the ability to mature into endocrine cells in rodent models. To protect the transplanted cells from immune response, retrieval encapsulation devices were also created [160,161,162]. In an initial human clinical trial conducted in 2014 (NCT02239354), the Encaptra device was utilized with the aim of providing complete immunoprotection of transplanted cells through the use of a cell-impermeable membrane. Although, the PEC-Encap product showed reliable tolerance and minimal adverse effects, the trial was stopped due to the inadequate engraftment of functional products. While, a few endocrine cells were observed, fibrosis around the capsule led to graft loss and supression of the insulin secretion. To address this challenge, a more recent development called the PEC-Direct device was introduced, which featured openings in the membrane to facilitate vascularization, thereby improving nutrient exchange and supporting cell viability. However, since host cells could infiltrate the device, immunosuppression was necessary following the transplantation [163,164,165]. Protocols were developed to generate clusters of stem cell-derived beta cells that secreted glucose-responsive insulin. These clusters, referred to SC-islets, also contained other endocrine cells, including glucagon-producing cells. SC-islets improved glycemic control in diabetic mice and nonhuman primates [146, 166,167,168]. In a trial conducted in 2017 (NCT03163511), the transplantation of progenitor cells resulted in the maturation of endocrine cells, and glucose-responsive C-peptide secretion was observed 6–9 months post-transplantation. Notably, the majority of these mature endocrine cells exhibited glucagon-positive characteristics. The porous regions housing the endocrine cells allowed for the infiltration of host vessels to facilitate vascularization. However, non-cellular regions were isolated by the presence of fibrosis [164, 165]. Although, there was not a sufficient levels of circulating C-peptide in these trials, the findings underscored the significance of promoting vascularization and minimizing fibrotic reactions [164, 169]. Vertex conducted a human trial in 2021 (NCT04786262) involving the transplantation of half-dose VX-880 cells (SC-islets) without a device to avoid previous problems, which necessitated immunosuppression. Preliminary results reported improved glycemic control, although it took longer to achieve the same outcome compared to rodent models [158]. Overall, progresses in islet transplantation and stem cell-derived beta cells pave the way for overcoming the limitations of traditional approaches. Further research and refinements are also required to achieve consistent and clinically significant outcomes in the treatment of diabetes.
Chalenges and limitations
Cell-based therapies have been significantly progressed for diabetes; however, there are still several challenges that need to be overcome. Clinical trials investigating encapsulation devices and islet transplantation techniques have provided valuable insights but face several obstacles including oxygenation, host immune responses, and insufficient long-term engraftment success. Immunoengineering of biomaterials and additive manufacturing for the development of 3D islet structures aim to modulate inflammation and promote graft revascularization. Nevertheless, achieving consistent normalization of blood glucose levels without exogenous insulin remains a challenge in human studies. In the field of gene therapy and stem cell differentiation, research focuses on genetically-modified or progenitor-derived insulin-secreting β-like cells to optimize protocols that ensure safety and functionality. The main challenge is to establish stable and functional cells capable of permanently restoring normoglycemia without the need for external intervention. One major barrier is the immune response, which targets allogeneic and xenogeneic islet grafts. Although, local immunotherapy minimizes the systemic effects, evading graft destruction through biomaterials without the requirement of immune suppression remains a significant challenge. The translation of precision 3D islet constructs and genetically reprogrammed cells also necessitates scalable manufacturing processes to ensure consistent function and long-term safety across batches. When critically appraising progress in the field of cell-based diabetes treatments, it is imperative to consider the regulatory, ethical, economic, and safety factors that shape translational applications. At the regulatory level, oversight bodies play a pivotal role in establishing standards to ensure patient welfare while enabling therapeutic innovation. FDA oversees clinical trials and product approvals in the United States (US), while in Europe the EMA provides parallel regulatory guidance. Within the US, organizations like the United Network for Organ Sharing (UNOS) and Organ Procurement and Transplantation Network (OPTN) govern organ and cell allocation protocols [17, 170]. However, as regenerative approaches diverge from traditional organ transplantation, regulatory pathways require ongoing harmonization between the agencies and jurisdictions. Continual dialogue between researchers, oversight boards, and policymakers will be crucial to streamline guidelines in a patient-centric manner that balances safety, efficacy, and timely access to cutting-edge therapies. For instance, as stem cell-derived beta cells and 3D bioprinted tissue constructs emerge, traditional drug and device frameworks may not adequately address product characterization and manufacturing complexities for these advanced therapeutic products [67]. Within clinics, maintaining compliance with evolving regulations impacts research directives and ultimately patients’ access to the novel treatments. Addressing informed consent, clinical trial design, and privacy protections for sensitive health data are also paramount from an ethical perspective [128, 129]. Autonomy and agency of research participants in decision-making related to experimental therapies demand prudency. Equitable accessibility of new treatment options also warrants attention to avoid certain populations facing undue barriers. Cell sourcing presents ethical issues depending on derivation from embryonic, fetal or adult tissues. Logistical matters like ship** and processing stem cell-derived islets prior to transplantation necessitate scrutiny. Tumorigenic potential of the undifferentiated pluripotent stem cells should be optimized through rigorous preclinical testing. Transitioning therapies between animal and early human investigations necessitates well-characterized cellular products showing consistent safety and glucose-responsive insulin secretion profiles comparable to pancreatic islets. Long-term animal model data substantiating lack of malignant transformation following transplantation aids allaying ethical safety concerns as the therapies progress clinically. Researchers carefully screen new concepts to prevent side effects in participants while pursuing curative goals. In terms of economic costs, islet and stem cell transplant procedures remain prohibitively expensive for broad applicability despite promising clinical signals. The field requires sustained study to validate techniques, track long-term outcomes, assess healthcare costs offsets from mitigating diabetes’ debilitating complications, and establish cost-benefit ratios for national reimbursement paradigms. Public-private partnerships may accelerate large, interventional trials and longitudinal research to precisely quantify the cellular therapies’ safety profiles and real-world efficacies compared to intensive management versus costs of intensive diabetes care. Ongoing developments like 3D bioprinting offer catalytic manufacturing potential fundamentally recalibrating economics by enhancing yields, standardizing procedures, and reducing costs through scale. By thoroughly and sensitively examining regulatory frameworks, informed consent processes, risks and benefits, as well as financial considerations at both micro and macro levels, researchers, oversight boards and broader stakeholder networks can advance cell-based therapies towards delivering life-changing benefits for all communities. A multidisciplinary, conscientious approach balances progress against patient welfare. A combination of multiple strategies may help to overcome these limitations. For instance, gene-modified islets integrated within vascularized biomaterial implants or sequenced therapies have promising results to prime grafts in pro-regenerative environments before transplantation. Collaboration across disciplines offers hope that refined individualized therapies may eventually achieve durable insulin independence through functional pancreatic cell or tissue engraftment, not only for diabetes but also for chronic pancreatitis. Regarding, ongoing progresses in unraveling these barriers, cell replacement approaches have the potential to improve diabetes management.
Conclusions
This review provides a comprehensive overview of the advances, challenges, and future directions in various cell-based therapeutic approaches for the treatment of diabetes. Significant progresses have been achieved in microencapsulation design, immunomodulation, tissue constructs, genetic and cellular reprogramming techniques, as well as initial clinical translation. However, the complete restoration of normoglycemia without the need for lifelong immunosuppression is still considered as a significant therapeutic challenge. Therefore, addressing the transplant environment of the hostile nature, develo** minimally invasive delivery methods, and overcoming limitations in engraftment efficiency and longevity are crucial issues for the future researches. Through the sustained multidisciplinary efforts for the improvement of existing strategies and establishing novel paradigms, achieving durable insulin independence can be a realistic goal for all diabetic cases through the personalized cell replacement or regeneration.
Immune Responses toward pancreatic islets following transplantation. This figure illustrates the immune responses, including the innate and adaptive immunity that are triggered upon pancreatic islet transplantation. Immune response begins with the activation of tissue macrophages and neutrophils in response to injury. Subsequent, release of inflammatory cytokines stimulates antigen-presenting cells (APCs), CD4 + T cells, CD8 + T cells, and cytotoxic T lymphocytes to orchestrate the immune response
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABS:
-
Acrylonitrile butadiene styrene
- APCs:
-
Activate antigen-presenting cells
- AAV:
-
Adeno-associated virus
- PDX1:
-
Duodenal homeobox 1
- EPIs:
-
Engineered pseudo islets
- ePTFE:
-
Expanded polytetrafluoroethylene
- ECM:
-
Extracellular matrix
- FBR:
-
Foreign body response
- FFF:
-
Fused filament fabrication
- GDM:
-
Gestational diabetes mellitus
- G6Pase:
-
Glucose 6-phosphatase
- IGFBP-1:
-
Insulin-like growth factor binding protein-1
- MSCs:
-
Mesenchymal stem cells
- NGN3:
-
Neurogenin 3
- OPTN:
-
Organ Procurement and Transplantation Network
- PEPCK:
-
Phosphoenolpyruvate carboxykinase
- PAEK:
-
Polyaryletherketone
- PCL:
-
Polycaprolactone
- PC:
-
Polycarbonate
- PEEK:
-
Polyetheretherketone
- PEI:
-
Polyetherimide
- PLA:
-
Poly-lactic acid
- PS:
-
Polystyrene
- SLA:
-
Stereolithography
- TPU:
-
Thermoplastic polyurethane
- T1D:
-
Type 1 diabetes
- T1DM:
-
Type 1 diabetes mellitus
- T2DM:
-
Type 2 diabetes mellitus
- UNOS:
-
United Network for Organ Sharing
- US:
-
United States
- VEGF:
-
Vascular endothelial growth factor
References
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Cho NH, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Moghbeli M, Naghibzadeh B, Ghahraman M, Fatemi S, Taghavi M, Vakili R, et al. Mutations in HNF1A gene are not a Common cause of familial young-onset diabetes in Iran. Indian J Clin Biochem. 2018;33(1):91–5.
Akhlaghipour I, Bina AR, Mogharrabi MR, Fanoodi A, Ebrahimian AR, Khojasteh Kaffash S, et al. Single-nucleotide polymorphisms as important risk factors of diabetes among Middle East population. Hum Genomics. 2022;16(1):11.
Moghbeli M, Khedmatgozar H, Yadegari M, Avan A, Ferns GA, Ghayour Mobarhan M. Cytokines and the immune response in obesity-related disorders. Adv Clin Chem. 2021;101:135–68.
Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Reviews Endocrinol. 2020;16(7):349–62.
Siqueira ISLd, Alves Guimarães R, Mamed SN, Santos TAP, Rocha SD, Pagotto V, et al. Prevalence and risk factors for self-report diabetes mellitus: a population-based study. Int J Environ Res Public Health. 2020;17(18):6497.
Free radical research.
Zhu B, Qu S. The relationship between diabetes mellitus and cancers and its underlying mechanisms. Front Endocrinol. 2022;13:800995.
Mojarrad M, Moghbeli M. Genetic and molecular biology of bladder cancer among Iranian patients. Mol Genet Genomic Med. 2020;8(6):e1233.
Moghbeli M. Genetic and molecular biology of breast cancer among Iranian patients. J Transl Med. 2019;17(1):218.
Abbaszadegan MR, Moghbeli M. Genetic and molecular origins of colorectal Cancer among the iranians: an update. Diagn Pathol. 2018;13(1):97.
Kim I. A brief overview of cell therapy and its product. J Korean Association Oral Maxillofacial Surg. 2013;39(5):201.
Mount NM, Ward SJ, Kefalas P, Hyllner J. Cell-based therapy technology classifications and translational challenges. Philosophical Trans Royal Soc B: Biol Sci. 2015;370(1680):20150017.
El-Kadiry AE-H, Rafei M, Shammaa R. Cell therapy: types, regulation, and clinical benefits. Front Med. 2021;8:756029.
Squifflet J-P, Gruessner R, Sutherland D. The history of pancreas transplantation: past, present and future. Acta Chir Belg. 2008;108(3):367–78.
Parums DV. First Regulatory approval for allogeneic pancreatic islet Beta cell infusion for adult patients with type 1 diabetes Mellitus. Med Sci Monitor: Int Med J Experimental Clin Res. 2023;29:e941918–1.
Yang L, Hu Z-M, Jiang F-X, Wang W. Stem cell therapy for insulin-dependent diabetes: are we still on the road? World J Stem Cells. 2022;14(7):503.
Affan M, Dar MS. Donislecel-the first approved pancreatic islet cell therapy medication for type 1 diabetes: a letter to the editor. Ir J Med Sci (1971-). 2023:1–2.
Harris E. FDA greenlights first cell therapy for adults with type 1 diabetes. JAMA. 2023.
Soon-Shiong P, Heintz R, Merideth N, Yao Q, Yao Z, Zheng T, et al. Insulin independence in a type 1 diabetic patient after encapsulated islet transplantation. Lancet (London England). 1994;343(8903):950–1.
Calafiore R, Basta G, Luca G, Lemmi A, Montanucci MP, Calabrese G, et al. Microencapsulated pancreatic islet allografts into nonimmunosuppressed patients with type 1 diabetes: first two cases. Diabetes Care. 2006;29(1):137–8.
Tuch BE, Keogh GW, Williams LJ, Wu W, Foster JL, Vaithilingam V, et al. Safety and viability of microencapsulated human islets transplanted into diabetic humans. Diabetes Care. 2009;32(10):1887–9.
Weng L, Wang X, Liu H, Yu Z, Liu S. Light-responsive microneedle array with tunable insulin release function for painless and on-demand anti-diabetic therapy. Mater Lett. 2023:135684.
Okcu A, Yazir Y, Şimşek T, Mert S, Duruksu G, Öztürk A, et al. Investigation of the effect of pancreatic decellularized matrix on encapsulated islets of Langerhans with mesenchymal stem cells. Tissue Cell. 2023;82:102110.
Khaliq T, Sohail M, Minhas MU, Mahmood A, Munir A, Qalawlus AHM, et al. Hyaluronic acid/alginate-based biomimetic hydrogel membranes for accelerated diabetic wound repair. Int J Pharm. 2023;643:123244.
Kuwabara R, Qin T, Llacua LA, Hu S, Boekschoten MV, de Haan BJ, et al. Extracellular matrix inclusion in immunoisolating alginate-based microcapsules promotes longevity, reduces fibrosis, and supports function of islet allografts in vivo. Acta Biomater. 2023;158:151–62.
Kirk K, Hao E, Lahmy R, Itkin-Ansari P. Human embryonic stem cell derived islet progenitors mature inside an encapsulation device without evidence of increased biomass or cell escape. Stem cell Res. 2014;12(3):807–14.
Dufrane D, van Steenberghe M, Goebbels R-M, Saliez A, Guiot Y, Gianello P. The influence of implantation site on the biocompatibility and survival of alginate encapsulated pig islets in rats. Biomaterials. 2006;27(17):3201–8.
Pullen LC. Stem cell–derived pancreatic progenitor cells have now been transplanted into patients: report from IPITA 2018. Wiley Online Library; 2018. pp. 1581–2.
Dang HP, Chen H, Dargaville TR, Tuch BE. Cell delivery systems: toward the next generation of cell therapies for type 1 diabetes. J Cell Mol Med. 2022;26(18):4756–67.
Viacyte. ViaCyte and gore enter clinical phase agreement based on novel membrane technology for PEC-encap product candidate. 2020.
Viacyte. viacyte announces initiation of phase 2 study of encapsulated cell therapy for type 1 diabetes patients 2021 2021. https://viacyte.com/press-releases/viacyte‐announces‐initiation‐of‐phase‐2‐study‐of‐encapsulated‐cell‐ther‐apy‐for‐type‐1‐diabetes‐patients/.
Hodgson J. Drug pipeline 3Q23—ERT, bispecifics and CRISPR in sickle cell disease. Nat Biotechnol. 2023;41(11):1498–500.
Pagliuca F. Pre-clinical proof-of-Concept in two lead programs in type 1 diabetes. International Socety for Stem Cell Research; 2019.
Jones PM, Persaud SJ. β-cell replacement therapy for type 1 diabetes: closer and closer. Diabet Med. 2022;39(6).
Carlsson P-O, Espes D, Sedigh A, Rotem A, Zimerman B, Grinberg H, et al. Transplantation of macroencapsulated human islets within the bioartificial pancreas βAir to patients with type 1 diabetes mellitus. Am J Transplant. 2018;18(7):1735–44.
Ludwig B, Zimerman B, Steffen A, Yavriants K, Azarov D, Reichel A, et al. A novel device for islet transplantation providing immune protection and oxygen supply. Horm Metab Res. 2010;42(13):918–22.
Evron Y, Colton CK, Ludwig B, Weir GC, Zimermann B, Maimon S, et al. Long-term viability and function of transplanted islets macroencapsulated at high density are achieved by enhanced oxygen supply. Sci Rep. 2018;8(1):6508.
Cao R, Avgoustiniatos E, Papas K, de Vos P, Lakey JR. Mathematical predictions of oxygen availability in micro-and macro‐encapsulated human and porcine pancreatic islets. J Biomedical Mater Res Part B: Appl Biomaterials. 2020;108(2):343–52.
Gala-Lopez B, Pepper A, Dinyari P, Malcolm A, Kin T, Pawlick L, et al. Subcutaneous clinical islet transplantation in a prevascularized subcutaneous pouch–preliminary experience. CellR4. 2016;4(5):e2132.
Sernova Corp Presents Positive Preliminary. Safety and Efficacy Data in its Phase I/II Clinical Trial for Type-1 Diabetes: Biospace. https://www.biospace.com/article/sernova‐corp‐presents‐positive‐preliminary‐safety‐and‐efficacy‐data‐in‐its‐phase‐i‐ii‐clinical‐trial‐for‐type‐1‐diabetes/.
Bachul PJ, Perez-Gutierrez A, Juengel B, Golab K, Basto L, Perea L et al. 306-OR: modified approach for improved isllotransplantation into prevascularized sernova cell pouch device: preliminary results of the phase i/ii clinical trial at University of Chicago. Diabetes. 2022;71(Supplement_1).
Vegas AJ, Veiseh O, Doloff JC, Ma M, Tam HH, Bratlie K, et al. Combinatorial hydrogel library enables identification of materials that mitigate the foreign body response in primates. Nat Biotechnol. 2016;34(3):345–52.
Vegas AJ, Veiseh O, Gürtler M, Millman JR, Pagliuca FW, Bader AR, et al. Long-term glycemic control using polymer-encapsulated human stem cell–derived beta cells in immune-competent mice. Nat Med. 2016;22(3):306–11.
Shapiro AD, Konkle BA, Croteau SE, Miesbach WA, Hay CRM, Kazmi R, et al. First-in-human phase 1/2 clinical trial of SIG-001, an innovative shielded cell therapy platform, for hemophilia Α. Blood. 2020;136:8.
Taraballi F, Sushnitha M, Tsao C, Bauza G, Liverani C, Shi A, et al. Biomimetic tissue engineering: tuning the immune and inflammatory response to implantable biomaterials. Adv Healthc Mater. 2018;7(17):1800490.
Yesilyurt V, Veiseh O, Doloff JC, Li J, Bose S, **e X, et al. A facile and versatile method to endow biomaterial devices with zwitterionic surface coatings. Adv Healthc Mater. 2017;6(4):1601091.
Liu Q, Chiu A, Wang L-H, An D, Zhong M, Smink AM, et al. Zwitterionically modified alginates mitigate cellular overgrowth for cell encapsulation. Nat Commun. 2019;10(1):5262.
Noverraz F, Montanari E, Pimenta J, Szabó L, Ortiz D, Gonelle-Gispert C, et al. Antifibrotic effect of ketoprofen-grafted alginate microcapsules in the transplantation of insulin producing cells. Bioconjug Chem. 2018;29(6):1932–41.
Jeon SI, Jeong J-H, Kim JE, Haque MR, Kim J, Byun Y, et al. Synthesis of PEG-dendron for surface modification of pancreatic islets and suppression of the immune response. J Mater Chem B. 2021;9(11):2631–40.
Derakhshankhah H, Sajadimajd S, Jahanshahi F, Samsonchi Z, Karimi H, Hajizadeh-Saffar E, et al. Immunoengineering Biomaterials in Cell-based therapy for type 1 diabetes. Tissue Eng Part B: Reviews. 2022;28(5):1053–66.
Piemonti L, Maffi P, Nano R, Bertuzzi F, Melzi R, Mercalli A, et al. Treating diabetes with islet transplantation: lessons from the Milan experience. Transplantation, Bioengineering, and regeneration of the endocrine pancreas. Elsevier; 2020. pp. 645–58.
Azzi J, Tang L, Moore R, Tong R, El Haddad N, Akiyoshi T, et al. Polylactide-cyclosporin A nanoparticles for targeted immunosuppression. FASEB J. 2010;24(10):3927.
Chen X, Liu H, Li H, Cheng Y, Yang L, Liu Y. In vitro expansion and differentiation of rat pancreatic duct-derived stem cells into insulin secreting cells using a dynamic three-dimensional cell culture system. Genet Mol Res. 2016;15(2).
Becker MW, Simonovich JA, Phelps EA. Engineered microenvironments and microdevices for modeling the pathophysiology of type 1 diabetes. Biomaterials. 2019;198:49–62.
Graham JG, Zhang X, Goodman A, Pothoven K, Houlihan J, Wang S, et al. PLG scaffold delivered antigen-specific regulatory T cells induce systemic tolerance in autoimmune diabetes. Tissue Eng Part A. 2013;19(11–12):1465–75.
Izadi Z, Hajizadeh-Saffar E, Hadjati J, Habibi-Anbouhi M, Ghanian MH, Sadeghi-Abandansari H, et al. Tolerance induction by surface immobilization of Jagged-1 for immunoprotection of pancreatic islets. Biomaterials. 2018;182:191–201.
McHugh MD, Park J, Uhrich R, Gao W, Horwitz DA, Fahmy TM. Paracrine co-delivery of TGF-β and IL-2 using CD4-targeted nanoparticles for induction and maintenance of regulatory T cells. Biomaterials. 2015;59:172–81.
Chen H, Teramura Y, Iwata H. Co-immobilization of urokinase and thrombomodulin on islet surfaces by poly (ethylene glycol)-conjugated phospholipid. J Controlled Release. 2011;150(2):229–34.
Su J, Hu B-H, Lowe WL Jr, Kaufman DB, Messersmith PB. Anti-inflammatory peptide-functionalized hydrogels for insulin-secreting cell encapsulation. Biomaterials. 2010;31(2):308–14.
Dong H, Fahmy TM, Metcalfe SM, Morton SL, Dong X, Inverardi L, et al. Immuno-isolation of pancreatic islet allografts using pegylated nanotherapy leads to long-term normoglycemia in full MHC mismatch recipient mice. PLoS ONE. 2012;7(12):e50265.
Kumar M, Nandi SK, Kaplan DL, Mandal BB. Localized immunomodulatory silk macrocapsules for islet-like spheroid formation and sustained insulin production. ACS Biomaterials Sci Eng. 2017;3(10):2443–56.
Hotaling NA, Tang L, Irvine DJ, Babensee JE. Biomaterial Strategies for Immunomodulation. Annu Rev Biomed Eng. 2015;17:317–49.
Shi Y, Zhao YZ, Jiang Z, Wang Z, Wang Q, Kou L, et al. Immune-Protective formulations and process strategies for improved survival and function of transplanted islets. Front Immunol. 2022;13:923241.
Zhang S, Yang H, Wang M, Mantovani D, Yang K, Witte F, et al. Immunomodulatory biomaterials against bacterial infections: Progress, challenges, and future perspectives. Innovation. 2023;4(6):100503.
Accolla RP, Simmons AM, Stabler CL. Integrating Additive Manufacturing techniques to improve cell-based implants for the treatment of type 1 diabetes. Adv Healthc Mater. 2022;11(13):e2200243.
Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. ACS; 2014.
Bol RJ, Šavija B. Micromechanical models for FDM 3D-Printed polymers: a review. Polymers. 2023;15(23):4497.
Paul S. Finite element analysis in fused deposition modeling research: a literature review. Measurement. 2021;178:109320.
Monaldo E, Ricci M, Marfia S. Mechanical properties of 3D printed polylactic acid elements: experimental and numerical insights. Mech Mater. 2023;177:104551.
Anoop M, Senthil P. Microscale representative volume element based numerical analysis on mechanical properties of fused deposition modelling components. Materials Today: Proceedings. 2021;39:563 – 71.
McGuigan AP, Sefton MV. Vascularized organoid engineered by modular assembly enables blood perfusion. Proceedings of the National Academy of Sciences. 2006;103(31):11461-6.
Pedraza E, Coronel MM, Fraker CA, Ricordi C, Stabler CL. Preventing hypoxia-induced cell death in beta cells and islets via hydrolytically activated, oxygen-generating biomaterials. Proceedings of the National Academy of Sciences. 2012;109(11):4245-50.
Espona-Noguera A, Ciriza J, Cañibano-Hernández A, Orive G, Hernández RM, del Saenz L, et al. Review of advanced hydrogel-based cell encapsulation systems for insulin delivery in type 1 diabetes mellitus. Pharmaceutics. 2019;11(11):597.
Dimitrioglou N, Kanelli M, Papageorgiou E, Karatzas T, Hatziavramidis D. Paving the way for successful islet encapsulation. Drug Discovery Today. 2019;24(3):737–48.
Omer A, Duvivier-Kali V, Fernandes J, Tchipashvili V, Colton CK, Weir GC. Long-term normoglycemia in rats receiving transplants with encapsulated islets. Transplantation. 2005;79(1):52–8.
Song S, Roy S. Progress and challenges in macroencapsulation approaches for type 1 diabetes (T1D) treatment: cells, biomaterials, and devices. Biotechnol Bioeng. 2016;113(7):1381–402.
Zhi ZL, Kerby A, King AJF, Jones PM, Pickup JC. Nano-scale encapsulation enhances allograft survival and function of islets transplanted in a mouse model of diabetes. Diabetologia. 2012;55(4):1081–90.
Farina M, Chua CYX, Ballerini A, Thekkedath U, Alexander JF, Rhudy JR, et al. Transcutaneously refillable, 3D-printed biopolymeric encapsulation system for the transplantation of endocrine cells. Biomaterials. 2018;177:125–38.
Farina M, Ballerini A, Fraga DW, Nicolov E, Hogan M, Demarchi D et al. 3D printed vascularized device for Subcutaneous Transplantation of Human islets. Biotechnol J. 2017;12(9).
Lei D, Yang Y, Liu Z, Yang B, Gong W, Chen S, et al. 3D printing of biomimetic vasculature for tissue regeneration. Mater Horiz. 2019;6(6):1197–206.
Melchels FP, Domingos MA, Klein TJ, Malda J, Bartolo PJ, Hutmacher DW. Additive manufacturing of tissues and organs. Prog Polym Sci. 2012;37(8):1079–104.
Ernst AU, Wang LH, Ma M. Interconnected toroidal hydrogels for islet encapsulation. Adv Healthc Mater. 2019;8(12):1900423.
Liang J-P, Accolla RP, Jiang K, Li Y, Stabler CL. Controlled release of anti-inflammatory and proangiogenic factors from macroporous scaffolds. Tissue Eng Part A. 2021;27(19–20):1275–89.
Pedraza E, Brady A-C, Fraker CA, Molano RD, Sukert S, Berman DM, et al. Macroporous three-dimensional PDMS scaffolds for extrahepatic islet transplantation. Cell Transplant. 2013;22(7):1123–35.
Chiu Y-C, Cheng M-H, Engel H, Kao S-W, Larson JC, Gupta S, et al. The role of pore size on vascularization and tissue remodeling in PEG hydrogels. Biomaterials. 2011;32(26):6045–51.
Kuss MA, Wu S, Wang Y, Untrauer JB, Li W, Lim JY, et al. Prevascularization of 3D printed bone scaffolds by bioactive hydrogels and cell co-culture. J Biomedical Mater Res Part B: Appl Biomaterials. 2018;106(5):1788–98.
Liu X, Jakus AE, Kural M, Qian H, Engler A, Ghaedi M, et al. Vascularization of natural and synthetic bone scaffolds. Cell Transplant. 2018;27(8):1269–80.
Costa-Almeida R, Gomez-Lazaro M, Ramalho C, Granja PL, Soares R, Guerreiro SG. Fibroblast-endothelial partners for vascularization strategies in tissue engineering. Tissue Eng Part A. 2015;21(5–6):1055–65.
Newman AC, Nakatsu MN, Chou W, Gershon PD, Hughes CC. The requirement for fibroblasts in angiogenesis: fibroblast-derived matrix proteins are essential for endothelial cell lumen formation. Mol Biol Cell. 2011;22(20):3791–800.
Vlahos AE, Cober N, Sefton MV. Modular tissue engineering for the vascularization of subcutaneously transplanted pancreatic islets. Proceedings of the National Academy of Sciences. 2017;114(35):9337-42.
Farina M, Ballerini A, Fraga DW, Nicolov E, Hogan M, Demarchi D, et al. 3D printed vascularized device for subcutaneous transplantation of human islets. Biotechnol J. 2017;12(9):1700169.
Bertassoni LE, Cecconi M, Manoharan V, Nikkhah M, Hjortnaes J, Cristino AL, et al. Hydrogel bioprinted microchannel networks for vascularization of tissue engineering constructs. Lab Chip. 2014;14(13):2202–11.
Jia W, Gungor-Ozkerim PS, Zhang YS, Yue K, Zhu K, Liu W, et al. Direct 3D bioprinting of perfusable vascular constructs using a blend bioink. Biomaterials. 2016;106:58–68.
Gao Q, Liu Z, Lin Z, Qiu J, Liu Y, Liu A, et al. 3D bioprinting of vessel-like structures with multilevel fluidic channels. ACS Biomaterials Sci Eng. 2017;3(3):399–408.
Noor N, Shapira A, Edri R, Gal I, Wertheim L, Dvir T. 3D printing of personalized thick and perfusable cardiac patches and hearts. Adv Sci. 2019;6(11):1900344.
Hospodiuk M, Dey M, Ayan B, Sosnoski D, Moncal KK, Wu Y, et al. Sprouting angiogenesis in engineered pseudo islets. Biofabrication. 2018;10(3):035003.
Marchioli G, Luca AD, de Koning E, Engelse M, Van Blitterswijk CA, Karperien M, et al. Hybrid polycaprolactone/alginate scaffolds functionalized with VEGF to promote de novo vessel formation for the transplantation of islets of Langerhans. Adv Healthc Mater. 2016;5(13):1606–16.
Dionne KE, Colton CK, Lyarmush M. Effect of hypoxia on insulin secretion by isolated rat and canine islets of Langerhans. Diabetes. 1993;42(1):12–21.
de Groot M, Schuurs TA, Keizer PP, Fekken S, Leuvenink HG, Van Schilfgaarde R. Response of encapsulated rat pancreatic islets to hypoxia. Cell Transplant. 2003;12(8):867–75.
Thomas F, Wu J, Contreras JL, Smyth C, Bilbao G, He J, et al. A tripartite anoikis-like mechanism causes early isolated islet apoptosis. Surgery. 2001;130(2):333–8.
Barkai U, Rotem A, de Vos P. Survival of encapsulated islets: more than a membrane story. World J Transplantation. 2016;6(1):69.
Jiang K, Chaimov D, Patel SN, Liang JP, Wiggins SC, Samojlik MM, et al. 3-D physiomimetic extracellular matrix hydrogels provide a supportive microenvironment for rodent and human islet culture. Biomaterials. 2019;198:37–48.
Pati F, Jang J, Ha D, Won Kim S, Rhie J, Shim J, et al. Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat Commun. 2014;5:3935.
Kim BS, Kwon YW, Kong J-S, Park GT, Gao G, Han W, et al. 3D cell printing of in vitro stabilized skin model and in vivo pre-vascularized skin patch using tissue-specific extracellular matrix bioink: a step towards advanced skin tissue engineering. Biomaterials. 2018;168:38–53.
Hu S, Martinez-Garcia FD, Moeun BN, Burgess JK, Harmsen MC, Hoesli C, et al. An immune regulatory 3D-printed alginate-pectin construct for immunoisolation of insulin producing β-cells. Mater Sci Engineering: C. 2021;123:112009.
Phelps EA, Templeman KL, Thulé PM, García AJ. Engineered VEGF-releasing PEG–MAL hydrogel for pancreatic islet vascularization. Drug Delivery Translational Res. 2015;5:125–36.
Kooptiwut S, Kaewin S, Semprasert N, Sujjitjoon J, Junking M, Suksri K, et al. Estradiol prevents high glucose-induced β-cell apoptosis by decreased BTG2 expression. Sci Rep. 2018;8(1):12256.
Dang TT, Thai AV, Cohen J, Slosberg JE, Siniakowicz K, Doloff JC, et al. Enhanced function of immuno-isolated islets in diabetes therapy by co-encapsulation with an anti-inflammatory drug. Biomaterials. 2013;34(23):5792–801.
Wang Y, He D, Ni C, Zhou H, Wu S, Xue Z, et al. Vitamin D induces autophagy of pancreatic β-cells and enhances insulin secretion. Mol Med Rep. 2016;14(3):2644–50.
Tarafder S, Koch A, Jun Y, Chou C, Awadallah MR, Lee CH. Micro-precise spatiotemporal delivery system embedded in 3D printing for complex tissue regeneration. Biofabrication. 2016;8(2):025003.
Liu YY, Yu HC, Liu Y, Liang G, Zhang T, Hu QX. Dual drug spatiotemporal release from functional gradient scaffolds prepared using 3 D bioprinting and electrospinning. Polym Eng Sci. 2016;56(2):170–7.
Freeman FE, Pitacco P, van Dommelen LH, Nulty J, Browe DC, Shin J-Y, et al. 3D bioprinting spatiotemporally defined patterns of growth factors to tightly control tissue regeneration. Sci Adv. 2020;6(33):eabb5093.
Wong MS, Hawthorne WJ, Manolios N. Gene therapy in diabetes. Self Nonself. 2010;1(3):165.
Ahmad Z, Rasouli M, Azman AZF, Omar AR. Evaluation of insulin expression and secretion in genetically engineered gut K and L-cells. BMC Biotechnol. 2012;12:1–9.
Tudurí E, Bruin JE, Kieffer TJ. Restoring insulin production for type 1 diabetes. J Diabetes. 2012;4(4):319–31.
Romer AI, Sussel L. Pancreatic islet cell development and regeneration. Current opinion in endocrinology, diabetes, and obesity. 2015;22(4):255.
Jaén ML, Vilà L, Elias I, Jimenez V, Rodó J, Maggioni L, et al. Long-term efficacy and safety of insulin and glucokinase gene therapy for diabetes: 8-year follow-up in dogs. Mol therapy-methods Clin Dev. 2017;6:1–7.
Li H, Li X, Lam KS, Tam S, **ao W, Xu R. Adeno-associated virus-mediated pancreatic and duodenal homeobox gene-1 expression enhanced differentiation of hepatic oval stem cells to insulin-producing cells in diabetic rats. J Biomed Sci. 2008;15:487–97.
Schwitzgebel VM, Scheel DW, Conners JR, Kalamaras J, Lee JE, Anderson DJ, et al. Expression of neurogenin3 reveals an islet cell precursor population in the pancreas. Development. 2000;127(16):3533–42.
Abed A, Critchlow C, Flatt PR, McClenaghan NH, Kelly C. Directed differentiation of progenitor cells towards an islet-cell phenotype. Am J Stem Cells. 2012;1(3):196.
Zhao M, Amiel SA, Ajami S, Jiang J, Rela M, Heaton N, et al. Amelioration of streptozotocin-induced diabetes in mice with cells derived from human marrow stromal cells. PLoS ONE. 2008;3(7):e2666.
Handorf AM, Sollinger HW, Alam T. Genetic engineering of surrogate β cells for treatment of type 1 diabetes mellitus. J Diabetes Mellitus. 2015;5(04):295–312.
Grant MB, Adu-Agyeiwaah Y, Vieira CP, Asare-Bediako B, Hammer SS, Calzi SL, et al. Intravitreal administration of AAV2-SIRT1 reverses diabetic retinopathy (DR) in a murine model of type 2 diabetes (T2D). Investig Ophthalmol Vis Sci. 2022;63(7):2310.
Yoon J-W, Jun H-S. Recent advances in insulin gene therapy for type 1 diabetes. Trends Mol Med. 2002;8(2):62–8.
Hou W-R, **e S-N, Wang H-J, Su Y-Y, Lu J-L, Li L-L, et al. Intramuscular delivery of a naked DNA plasmid encoding proinsulin and pancreatic regenerating III protein ameliorates type 1 diabetes mellitus. Pharmacol Res. 2011;63(4):320–7.
Joo WS, Jeong JH, Nam K, Blevins KS, Salama ME, Kim SW. Polymeric delivery of therapeutic RAE-1 plasmid to the pancreatic islets for the prevention of type 1 diabetes. J Controlled Release. 2012;162(3):606–11.
Dezashibi HM, Shabani A. A Mini-review of Current Treatment approaches and Gene Therapy as potential interventions for diabetes Mellitus types 1. Adv Biomed Res. 2023;12:219.
Vantyghem M-C, de Koning EJ, Pattou F, Rickels MR. Advances in β-cell replacement therapy for the treatment of type 1 diabetes. Lancet. 2019;394(10205):1274–85.
Hudson A, Bradbury L, Johnson R, Fuggle S, Shaw J, Casey J, et al. The UK pancreas allocation scheme for whole organ and islet transplantation. Am J Transplant. 2015;15(9):2443–55.
Cornateanu SM, O’Neill S, Dholakia S, Counter CJ, Sherif AE, Casey JJ, et al. Pancreas utilization rates in the UK–an 11-year analysis. Transpl Int. 2021;34(7):1306–18.
Nordheim E, Lindahl JP, Carlsen RK, Åsberg A, Birkeland KI, Horneland R, et al. Patient selection for islet or solid organ pancreas transplantation: experiences from a multidisciplinary outpatient-clinic approach. Endocr Connections. 2021;10(2):230–9.
Arifin DR, Bulte JW. In vivo imaging of pancreatic islet grafts in diabetes treatment. Front Endocrinol. 2021;12:640117.
Murakami T, Fujimoto H, Inagaki N. Non-invasive beta-cell imaging: visualization, quantification, and beyond. Front Endocrinol. 2021;12:714348.
Piemonti L, Everly MJ, Maffi P, Scavini M, Poli F, Nano R, et al. Alloantibody and autoantibody monitoring predicts islet transplantation outcome in human type 1 diabetes. Diabetes. 2013;62(5):1656–64.
Anteby R, Lucander A, Bachul PJ, Pyda J, Grybowski D, Basto L, et al. Evaluating the prognostic value of islet autoantibody monitoring in islet transplant recipients with long-standing type 1 diabetes mellitus. J Clin Med. 2021;10(12):2708.
Buron F, Reffet S, Badet L, Morelon E, Thaunat O. Immunological monitoring in beta cell replacement: towards a pathophysiology-guided implementation of biomarkers. Curr Diab Rep. 2021;21:1–11.
Cantarelli E, Piemonti L. Alternative transplantation sites for pancreatic islet grafts. Curr Diab Rep. 2011;11:364–74.
Tremmel DM, Odorico JS. Rebuilding a better home for transplanted islets. Organogenesis. 2018;14(4):163–8.
Citro A, Moser PT, Dugnani E, Rajab TK, Ren X, Evangelista-Leite D, et al. Biofabrication of a vascularized islet organ for type 1 diabetes. Biomaterials. 2019;199:40–51.
Basta G, Montanucci P, Calafiore R. Microencapsulation of cells and molecular therapy of type 1 diabetes mellitus: the actual state and future perspectives between promise and progress. J Diabetes Invest. 2021;12(3):301–9.
Samojlik MM, Stabler CL. Designing biomaterials for the modulation of allogeneic and autoimmune responses to cellular implants in type 1 diabetes. Acta Biomater. 2021;133:87–101.
Carlsson P-O, Schwarcz E, Korsgren O, Le Blanc K. Preserved β-cell function in type 1 diabetes by mesenchymal stromal cells. Diabetes. 2015;64(2):587–92.
Madani S, Setudeh A, Aghayan HR, Alavi-Moghadam S, Rouhifard M, Rezaei N, et al. Placenta derived mesenchymal stem cells transplantation in type 1 diabetes: preliminary report of phase 1 clinical trial. J Diabetes Metabolic Disorders. 2021;20:1179–89.
Pagliuca FW, Millman JR, Gürtler M, Segel M, Van Dervort A, Ryu JH, et al. Generation of functional human pancreatic β cells in vitro. Cell. 2014;159(2):428–39.
Russ HA, Parent AV, Ringler JJ, Hennings TG, Nair GG, Shveygert M, et al. Controlled induction of human pancreatic progenitors produces functional beta-like cells in vitro. EMBO J. 2015;34(13):1759–72.
Sambathkumar R, Migliorini A, Nostro MC. Pluripotent stem cell-derived pancreatic progenitors and β-like cells for type 1 diabetes treatment. Physiology. 2018;33(6):394–402.
Sordi V, Monaco L, Piemonti L. Cell therapy for type 1 diabetes: from islet transplantation to stem cells. Hormone Res Paediatrics. 2022;96(6):658–69.
Henry RR, Pettus J, Wilensky J, SHAPIRO AJ, Senior PA, Roep B et al. Initial clinical evaluation of VC-01TM combination product—a stem cell–derived islet replacement for type 1 diabetes (T1D). Diabetes. 2018;67(Supplement_1).
Shapiro A, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus JH et al. Insulin expression and glucose-responsive circulating C-peptide in type 1 diabetes patients implanted subcutaneously with pluripotent stem cell-derived pancreatic endoderm cells in a macro-device. David and Donner, Thomas W and Bellin, Melena D and Hsueh, Willa and Pettus, Jeremy H and Wilensky, Jon S and Daniels, Mark and Wang, Richard M and Kroon, Evert J and Brandon, Eugene Paul and D’Amour, Kevin A and Foyt, Howard, Insulin Expression and Glucose-Responsive Circulating C-Peptide in Type. 2019;1.
Keymeulen B, Jacobs-Tulleneers-Thevissen D, Kroon EJ, Jaiman MS, Daniels M, Wang R et al. 196-LB: stem cell–derived islet replacement therapy (VC-02) demonstrates production of C-peptide in patients with type 1 diabetes (T1D) and hypoglycemia unawareness. Diabetes. 2021;70(Supplement_1).
Piemonti L. Felix dies natalis, insulin… ceterum autem censeo beta is better. Acta Diabetol. 2021;58(10):1287–306.
Sordi V, Pellegrini S, Piemonti L. Immunological issues after stem cell-based β cell replacement. Curr Diab Rep. 2017;17:1–8.
Coe TM, Markmann JF, Rickert CG. Current status of porcine islet xenotransplantation. Curr Opin Organ Transpl. 2020;25(5):449–56.
Edgar L, Pu T, Porter B, Aziz J, La Pointe C, Asthana A, et al. Regenerative medicine, organ bioengineering and transplantation. J Br Surg. 2020;107(7):793–800.
Mathur A, Taurin S, Alshammary S. The safety and efficacy of mesenchymal stem cells in the treatment of type 2 Diabetes- A literature review. Diabetes Metab Syndr Obes. 2023;16:769–77.
Hogrebe NJ, Ishahak M, Millman JR. Developments in stem cell-derived islet replacement therapy for treating type 1 diabetes. Cell Stem Cell. 2023;30(5):530–48.
Paraskevas S, Maysinger D, Wang R, Duguid WP, Rosenberg L. Cell loss in isolated human islets occurs by apoptosis. Pancreas. 2000;20(3):270–6.
Kelly OG, Chan MY, Martinson LA, Kadoya K, Ostertag TM, Ross KG, et al. Cell-surface markers for the isolation of pancreatic cell types derived from human embryonic stem cells. Nat Biotechnol. 2011;29(8):750–6.
Rezania A, Bruin JE, Riedel MJ, Mojibian M, Asadi A, Xu J, et al. Maturation of human embryonic stem cell–derived pancreatic progenitors into functional islets capable of treating pre-existing diabetes in mice. Diabetes. 2012;61(8):2016–29.
Kroon E, Martinson LA, Kadoya K, Bang AG, Kelly OG, Eliazer S, et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26(4):443–52.
Agulnick AD, Ambruzs DM, Moorman MA, Bhoumik A, Cesario RM, Payne JK, et al. Insulin-producing endocrine cells differentiated in vitro from human embryonic stem cells function in macroencapsulation devices in vivo. Stem Cells Translational Med. 2015;4(10):1214–22.
Ramzy A, Thompson DM, Ward-Hartstonge KA, Ivison S, Cook L, Garcia RV, et al. Implanted pluripotent stem-cell-derived pancreatic endoderm cells secrete glucose-responsive C-peptide in patients with type 1 diabetes. Cell Stem Cell. 2021;28(12):2047–61. e5.
Dolgin E, Diabetes. Encapsulating the problem. Nature. 2016;540(7632):S60–2.
Rezania A, Bruin JE, Arora P, Rubin A, Batushansky I, Asadi A, et al. Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells. Nat Biotechnol. 2014;32(11):1121–33.
Hogrebe NJ, Augsornworawat P, Maxwell KG, Velazco-Cruz L, Millman JR. Targeting the cytoskeleton to direct pancreatic differentiation of human pluripotent stem cells. Nat Biotechnol. 2020;38(4):460–70.
Nair GG, Liu JS, Russ HA, Tran S, Saxton MS, Chen R, et al. Recapitulating endocrine cell clustering in culture promotes maturation of human stem-cell-derived β cells. Nat Cell Biol. 2019;21(2):263–74.
Shapiro AJ, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus J et al. Insulin expression and C-peptide in type 1 diabetes subjects implanted with stem cell-derived pancreatic endoderm cells in an encapsulation device. Cell Rep Med. 2021;2(12).
Witkowski P, Anteby R, Olaitan OK, Forbes RC, Niederhaus S, Ricordi C, et al. Pancreatic islets Quality and Potency cannot be verified as required for drugs: reflection on the FDA Review of a biological license application for human islets. Transplantation. 2021;105(12):e409–10.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
RR, HRR, and ES were involved in search strategy and drafting. MM revised, designed, and supervised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Raoufinia, R., Rahimi, H.R., Saburi, E. et al. Advances and challenges of the cell-based therapies among diabetic patients. J Transl Med 22, 435 (2024). https://doi.org/10.1186/s12967-024-05226-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-024-05226-3