Abstract
Purpose
This study aimed to assess the feasibility and transferability of skills acquired using the Advanced Training in Laparoscopic Suturing (ATLAS) curriculum for novice trainees.
Methods
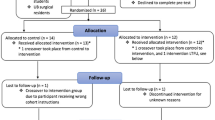
First-year medical students (n = 20) pre-tested on Fundamentals of Laparoscopic Surgery (FLS), ATLAS, and a Porcine Laparoscopic Nissen (PLN) model and were subsequently randomized into training and control groups. The training group trained to proficiency on FLS followed by post-test 1 (FLS/ATLAS/PLN), followed by proficiency-based ATLAS training and post-test 2 (FLS/ATLAS/PLN). The control group received no training and post-tested concurrently. Data are reported as median [interquartile range].
Results
There were nine dropouts; data were analyzed for training (n = 6) and control (n = 5) participants who completed the study. There were no significant differences between groups at baseline for overall pre-test and each subcomponent (p > 0.05). FLS training took 9.6 [7.6–11.6] hours, and ATLAS training 15.9 [13.9–25.8] hours. FLS training resulted in significant performance improvements in the overall and FLS scores versus controls. After ATLAS training, there was significant improvement in performance for the overall, FLS, ATLAS, and PLN scores versus controls. Workload was significantly higher for ATLAS compared to FLS training; however, ratings for curriculum appropriateness were similar.
Conclusions
This study demonstrated that proficiency-based ATLAS training was feasible with all training group participants achieving proficiency after a reasonable amount of time. Importantly, ATLAS training was associated with significant performance improvement following FLS training as measured by a live porcine model. These findings support further investigations and more widespread ATLAS adoption.








Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mattar SG, Alseidi AA, Jones DB, Jeyarajah DR, Swanstrom LL, Aye RW, Wexner SD, Martinez JM, Ross SB, Awad MM, Franklin ME, Arregui ME, Schirmer BD, Minter RM. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440–9. https://doi.org/10.1097/SLA.0b013e3182a191ca.
Crochet P, Agostini A, Knight S, Resseguier N, Berdah S, Aggarwal R. The performance gap for residents in transfer of intracorporeal suturing skills from box trainer to operating room. J Surg Educ. 2017;74(6):1019–27. https://doi.org/10.1016/j.jsurg.2017.05.013.
Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ. Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg. 2005;201(1):23–9. https://doi.org/10.1016/j.jamcollsurg.2005.02.021.
Stefanidis D, Scerbo MW, Korndorffer JR Jr, Scott DJ. Redefining simulator proficiency using automaticity theory. Am J Surg. 2007;193(4):502–6. https://doi.org/10.1016/j.amjsurg.2006.11.010.
Martin JR, Anton N, Timsina L, Whiteside J, Myers E, Stefanidis D. Performance variability during training on simulators is associated with skill transfer. Surgery. 2019;165(6):1065–8. https://doi.org/10.1016/j.surg.2019.01.013.
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Heniford BT, Scott DJ. Closing the gap in operative performance between novices and experts: does harder mean better for laparoscopic simulator training? J Am Coll Surg. 2007;205(2):307–13. https://doi.org/10.1016/j.jamcollsurg.2007.02.080.
Nepomnayshy D, Alseidi AA, Fitzgibbons SC, Stefanidis D. Identifying the need for and content of an advanced laparoscopic skills curriculum: results of a national survey. Am J Surg. 2016;211(2):421–5. https://doi.org/10.1016/j.amjsurg.2015.10.009.
Enani G, Watanabe Y, McKendy KM, Bilgic E, Feldman LS, Fried GM, Vassiliou MC. What are the training gaps for acquiring laparoscopic suturing skills? J Surg Educ. 2017;74(4):656–62. https://doi.org/10.1016/j.jsurg.2016.12.004.
Nagaraj MB, Nepomnayshy D, Stefanidis D, Alseidi A, Gee D, Ghaderi I, Shim JK, Scott DJ. Advanced Techniques in Laparoscopic Suturing (ATLAS): Optimization for National Curriculum Launch. American College of Surgeons- Accredited Education Institutes, March 2022, Virtual ePoster.
Watanabe Y, McKendy KM, Bilgic E, Enani G, Madani A, Munshi A, Feldman LS, Fried GM, Vassiliou MC. New models for advanced laparoscopic suturing: taking it to the next level. Surg Endosc. 2016;30(2):581–7. https://doi.org/10.1007/s00464-015-4242-6.
Nepomnayshy D, Whitledge J, Birkett R, Delmonico T, Ruthazer R, Sillin L, Seymour NE. Evaluation of advanced laparoscopic skills tasks for validity evidence. Surg Endosc. 2015;29(2):349–54. https://doi.org/10.1007/s00464-014-3674-8.
Bilgic E, Watanabe Y, Nepomnayshy D, Gardner A, Fitzgibbons S, Ghaderi I, Alseidi A, Stefanidis D, Paige J, Seymour N, McKendy KM, Birkett R, Whitledge J, Kane E, Anton NE, Vassiliou MC. Simulation committee of the association for surgical education. Multicenter proficiency benchmarks for advanced laparoscopic suturing tasks. Am J Surg. 2017;213(2):217–21. https://doi.org/10.1016/j.amjsurg.2016.07.033.
McKendy KM, Watanabe Y, Bilgic E, Enani G, Munshi A, Lee L, Feldman LS, Fried GM, Vassiliou MC. Establishing meaningful benchmarks: the development of a formative feedback tool for advanced laparoscopic suturing. Surg Endosc. 2017;31(12):5057–65. https://doi.org/10.1007/s00464-017-5569-y.
Nepomnayshy D, Whitledge J, Fitzgibbons S, Nijjar B, Gardner A, Alseidi A, Birkett R, Deal S, Duvra RR, Anton N, Stefanidis D. Advanced laparoscopic skills: understanding the relationship between simulation-based practice and clinical performance. Am J Surg. 2019;218(3):527–32. https://doi.org/10.1016/j.amjsurg.2019.01.024.
Gabrysz-Forget F, Bonds M, Lovett M, Alseidi A, Ghaderi I, Nepomnayshy D. Practicing on the advanced training in laparoscopic suturing curriculum (ATLAS): is mastery learning in residency feasible to achieve expert-level performance in laparoscopic suturing? J Surg Educ. 2020;77(5):1138–45. https://doi.org/10.1016/j.jsurg.2020.02.026.
Athanasiadis DI, Anton NE, Karim A, Colgate CL, Stefanidis D. Does the advanced training in laparoscopic suturing enhance laparoscopic suturing skill beyond fundamentals of laparoscopic surgery? Surgery. 2021;170(4):1125–30. https://doi.org/10.1016/j.surg.2021.06.041.
Dreyfus SE. The five-stage model of adult skill acquisition. Bull Sci Technol Soc. 2016;24(3):177–81. https://doi.org/10.1177/0270467604264992.
Ritter EM, Scott DJ. Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic surgery. Surg Innov. 2007;14(2):107–12. https://doi.org/10.1177/1553350607302329.
Scott DJ, Ritter EM, Tesfay ST, Pimentel EA, Nagji A, Fried GM. Certification pass rate of 100% for fundamentals of laparoscopic surgery skills after proficiency-based training. Surg Endosc. 2008;22(8):1887–93. https://doi.org/10.1007/s00464-008-9745-y.
Scott DJ. Proficiency-based training for surgical skills. Semin Colon Rectal Surg. 2008;19(2):72–80. https://doi.org/10.1053/j.scrs.2008.02.003.
Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10 Suppl):S70-81. https://doi.org/10.1097/00001888-200410001-00022.
Sandra HG, Staveland LE. Development of NASA-TLX (Task Load Index): results of empirical and theoretical research. Adv Psychol. 1988;52:139–93.
Stefanidis D, Korndorffer JR Jr, Sierra R, Touchard C, Dunne JB, Scott DJ. Skill retention following proficiency-based laparoscopic simulator training. Surgery. 2005;138(2):165–70. https://doi.org/10.1016/j.surg.2005.06.002.
Stefanidis D, Korndorffer JR Jr, Black FW, Dunne JB, Sierra R, Touchard CL, Rice DA, Markert RJ, Kastl PR, Scott DJ. Psychomotor testing predicts rate of skill acquisition for proficiency-based laparoscopic skills training. Surgery. 2006;140(2):252–62. https://doi.org/10.1016/j.surg.2006.04.002.
Nagaraj MB, AbdelFattah KR, Scott DJ, Farr DE. Creating a proficiency-based remote laparoscopic skills curriculum for the COVID-19 era. J Surg Educ. 2022;79(1):229–36. https://doi.org/10.1016/j.jsurg.2021.06.020.
Acknowledgements
The authors gratefully acknowledge support provided by the UT Southwestern Simulation Center. We would also like to thank the medical students who volunteered their time to participate in this study.
Funding
No funding received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no financial conflicts of interest to disclose.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagaraj, M.B., Langston, K. & Scott, D.J. Advanced Training in Laparoscopic Suturing (ATLAS) is feasible and addresses the transferability gap. Global Surg Educ 2, 15 (2023). https://doi.org/10.1007/s44186-022-00072-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-022-00072-7