Abstract
Background
The fundamentals of laparoscopic surgery (FLS) program has been extensively validated for use as a high-stakes examination for certification purposes, but optimal methods for its use in skills training have not been described. This study aimed to investigate the feasibility of implementing a proficiency-based FLS skills training curriculum and to evaluate its effectiveness in preparing trainees for certification.
Methods
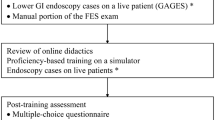
For this study, 21 novice medical students at two institutions viewed video tutorials, then performed one repetition of the five FLS tasks as a pretest. The pretests were scored using standard testing metrics. The trainees next practiced the tasks over a 2-month period until they achieved proficiency for all the tasks. A modified on-the-fly scoring system based on expert-derived performance was used. The trainees were posttested using the high-stakes examination format.
Results
No trainee passed the certification examination at pretesting. The trainees achieved proficiency for 96% of the five tasks during training, which required 9.7 ± 2.4 h (range, 6–14 h) and 119 ± 31 repetitions (range, 66–161 repetitions). The trainees rated the proficiency levels as “moderately difficult” (3.0 ± 0.7 on a 5-point scale) and “highly appropriate” (4.7 ± 0.1 on a 5-point scale). At posttesting, 100% of the trainees passed the certification examination and demonstrated significant improvement compared with pretesting for normalized score (468 ± 24 vs 126 ± 75; p < 0.001), self-rated laparoscopic comfort (89.4% vs 4.8%; p < 0.001), and skill level (3.6 ± 0.9 vs 1.2 ± 0.5; p < 0.001, 5-point scale).
Conclusions
This proficiency-based curriculum is feasible for training novices and uniformly allows sufficient skill acquisition for FLS certification. Endorsed by the Society of American Gastrointestinal Endoscopic Surgeons (SAGES), this curriculum is available for use as an optimal method for FLS skills training. More widespread adoption of this curriculum is encouraged.



Similar content being viewed by others
References
Fundamentals of Laparoscopic Surgery (FLS) program (2007) Society of American Gastrointestinal and Endoscopic Surgeons. Accessed on April 16, 2007 at http://www.flsprogram.org
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K, SAGES FLS Committee (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135:21–27
Derossis AM, Bothwell J, Sigman HH, Fried GM (1998) The effect of practice on performance in a laparoscopic simulator. Surg Endosc 12:1117–1120
Fried GM, Derossis AM, Bothwell J, Sigman HH (1999) Comparison of laparoscopic performance in vivo with performance measured in a laparoscopic simulator. Surg Endosc 13:1077–1081
Feldman LS, Sherman V, Fried GM (2004) Using simulators to assess laparoscopic competence: ready for widespread use? Surgery 135:28–42
Feldman LS, Hagarty SE, Ghitulescu G, Stanbridge D, Fried GM (2004) Relationship between objective assessment of technical skills and subjective in-training evaluations in surgical residents. J Am Coll Surg 198:105–110
Fried GM, Feldman LS, Vassiliou MC et al (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–525
Vassiliou M, Ghitulescu G, Feldman L et al (2006) The MISTELS program to measure technical skill in laparoscopic surgery: evidence for reliability. Surg Endosc 20:744–747
Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM (2003) Evaluating laparoscopic skills: setting the pass/fail score for the MISTELS system. Surg Endosc 17:964–967
Scott DJ (2006) Patient safety, competency, and the future of surgical simulation. Simul Healthcare 1:164–170
Seymour NE, Gallagher AG, Roman SA et al (2002) Virtual reality training improves OR performance: results of a randomized, double-blinded study. Ann Surg 236:458–463
Brunner WC, Korndorffer JR, Sierra R, Dunne JB, Yau CL, Corsetti RL, Slakey DP, Townsend MC, Scott DJ (2005) Determining standards for laparoscopic competency using virtual reality. Am Surg 71:1–5
Korndorffer JK, Scott DJ, Sierra R, Brunner WC, Dunne JB, Slakey DP, Townsend MC, Hewitt RL (2005) Develo** and testing competency levels for laparoscopic skills training. Arch Surg 140:80–84
Korndorffer JK, Hayes DJ, Dunne JB, Sierra R, Touchard TL, Markert RJ, Scott DJ (2005) Development and transferability of a cost-effective laparoscopic camera navigation simulator. Surg Endosc 19:161–167
Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the OR. J Am Coll Surg 201:23–29
Stefanidis D, Korndorffer JR Jr, Sierra R, Touchard C, Dunne JB, Scott DJ (2005) Skill retention following proficiency-based laparoscopic simulator training. Surgery 138:165–170
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372
Stefanidis D, Sierra R, Markley S, Korndorffer JR Jr, Scott DJ (2006) Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg 202:599–603
Aggarwal R, Grantcharov T, Moorthy K et al (2006) A competency-based virtual reality training curriculum for the acquisition of laparoscopic psychomotor skill. Am J Surg 191:128–133
Stefanidis D, Sierra R, Korndorffer JR Jr, Dunne JB, Markley S, Touchard C, Scott DJ (2006) Intensive CME course training on simulators results in proficiency for laparoscopic suturing. Am J Surg 191:23–27
Scott DJ, Goova MT, Tesfay ST (2007) A cost-effective proficiency-based knot-tying and suturing curriculum for residency programs. J Surg Res 141:7–15
Ritter EM, Scott DS (2007) Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic surgery. Surg Innov 14:107–112
Ericsson KA (2004) Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 79:S70–S81
Moulton CA, Dubrowski A, MacRae H, Graham B, Grober E, Reznick R (2006) Teaching surgical skills: what kind of practice makes perfect? A randomized, controlled trial. Ann Surg 244:400–409
Arthur W Jr, Bennet WJ, Stanush PL (1998) Factors that influence skill decay and retention: a quantitative review and analysis. Hum Perform 11:57–101
DaRosa DA, Bell RH, Dunnington GL (2003) Residency program models, implications, and evaluation: results of a think tank consortium on resident work hours. Surgery 133:13–23
Callery MP (2003) Expansion beyond compression. Surg Endosc 17:677–678
Valentine RJ, Rege RV (2004) Integrating technical competency into the surgical curriculum: doing more with less. Surg Clin North Am 84:1647–1667
Dunnington G (2006) Sim City: The APDS/ACS Surgical Skills Curriculum Committee. http://www.apds.org/Tucson%202006%20APDS%20PP.htm
Acknowledgments
We gratefully acknowledge the donated materials provided by the US Surgical Corporation, the guidance of the SAGES FLS Committee, and the invaluable assistance of Ms. Lisa Jukelevics.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Annual Meeting, Las Vegas, NV, 21 April 2007.
Rights and permissions
About this article
Cite this article
Scott, D.J., Ritter, E.M., Tesfay, S.T. et al. Certification pass rate of 100% for fundamentals of laparoscopic surgery skills after proficiency-based training. Surg Endosc 22, 1887–1893 (2008). https://doi.org/10.1007/s00464-008-9745-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9745-y