Abstract
Objective
This prospective, small sample study aims at exploring the potential of quantitative SUV analysis of dual-phase [99mTc]Tc-MIBI SPECT/CT for preoperative localization and differentiation of hyper-functioning parathyroid lesions (PL).
Materials and methods
40 hyperparathyroid patients (M: F; 12:28, Mean Age ± SD, 40.92 ± 13.48 years) underwent SPECT/CT scintigraphy with neck and mediastinum in field of view at early (90 min) and delayed (180 min) post injection (p.i.) of [99mTc] Tc-MIBI. Images were analyzed for PL localization. Maximum and mean SUV (SUVmax; SUVmean) at 90 and 180 min p.i. for PL as well as reference thyroid tissue were measured. PL classified as adenomas, carcinoma and hyperplasia on the basis of SUV were correlated with post-surgical histopathology. Statistical analysis with paired t-test was used to measure the significance of the difference in SUV values of adenoma and hyperplasia with reference thyroid tissue.
Results
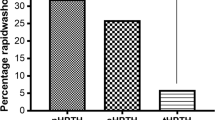
SPECT/CT identified PL in 25 out of 40 patients. Using SUVmax and SUVmean, PL were labeled as hyperplasia (02), adenomas (22), and carcinoma (01). Both SUV values showed a decline at 180 min p.i. as compared to 90 min p.i., but SUVmax was considered better for lesion characterization. SUVmax (g/mL) of carcinoma, adenomas, hyperplasia, and reference thyroid tissue were 16.656, 6.933 ± 2.037, 2.788 ± 0.279, and 1.117 ± 0.221 at 90 min p.i. Significant difference (P < 0.0001) of SUVmax between adenomas and reference thyroid tissue but no significant difference (P = 1.000) between hyperplasia and reference thyroid tissue at both time points was found. SUVmax at 90 min p.i. for carcinoma (16.656 g/ml) was also found higher than adenoma and hyperplasia. Parathyroid adenomas and carcinoma were confirmed on post-surgical histopathology of lesions in respective patients however two patients with hyperplasia could not undergo surgery.
Conclusion
SUVmax at 90 min p.i. of [99mTc]Tc-MIBI SPECT/CT was found to be a good quantitative parameter for PL localization and their noninvasive image-based classification.





Similar content being viewed by others
Data availability
Not applicable.
References
Listewnik MH, Piwowarska-Bilska H, Kurantowicz M et al (2017) Semi-quantitative method for the assessment of focal lesions in parathyroid scintigraphy with relation to histopathology: a prospective study. Nucl Med Rev 20:18–24
Fine EJ (1987) Parathyroid imaging: Its current status and future role. Semin Nucl Med 17:350–359
Morris MA, Saboury B, Ahlman M et al (2022) Parathyroid imaging: past, present, and future. Front Endocrinol (Lausanne). 12:1481
Lavely WC, Goetze S, Friedman KP et al (2007) Comparison of SPECT/CT, SPECT, and planar imaging with single- and dual-phase 99mTc-Sestamibi parathyroid scintigraphy. J Nucl Med 48:1084–1089
Lorberboym M, Minski I, Macadziob S et al (2003) Incremental diagnostic value of preoperative 99mTc-MIBI SPECT in patients with a parathyroid adenoma. J Nucl Med 44:904–908
Moka D, Voth E, Larena-Avellaneda A et al (1997) 99mTc-MIBI-SPECT for the location of small parathyroid adenoma. NuklearMedizin Schattauer GmbH 36:240–244
Zhao M, Li X, Huang J et al (2015) Value of single photon emission computed tomography/computerized tomography in the diagnosis of hyperparathyroidism and the comparative study with multiple imaging modality. J Central South Univ Med Sci 40:1016–1022
Özdemir E, Genç M, Aydos U et al (2020) Comparison of 99mTc-MIBI planar scintigraphy, SPET/CT and ultrasonography in detection of parathyroid adenoma in patients with primary hyperparathyroidism. Hell J Nucl Med 23:21–26
Quak E, Lasne Cardon A, Ciappuccini R et al (2021) Upfront F18-choline PET/CT versus 99mTc-sestaMIBI SPECT/CT guided surgery in primary hyperparathyroidism: the randomized phase III diagnostic trial APACH2. BMC Endocr Disord 21:1–7
Nichols KJ, Tomas MB, Tronco GG et al (2008) Preoperative parathyroid scintigraphic lesion localization: accuracy of various types of readings. Radiology 248:221–232
Qiu ZL, Wu B, Shen CT et al (2014) Dual-phase 99mTc-MIBI scintigraphy with delayed neck and thorax SPECT/CT and bone scintigraphy in patients with primary hyperparathyroidism: correlation with clinical or pathological variables. Ann Nucl Med 28:725–735
Israel O, Pellet O, Biassoni L et al (2019) Two decades of SPECT/CT – the coming of age of a technology: an updated review of literature evidence. Eur J Nucl Med Mol Imaging 46:1990–2012
Bailey DL, Willowson KP (2014) Quantitative SPECT/CT: SPECT joins PET as a quantitative imaging modality. Eur J Nucl Med Mol Imaging 41:17–25
Dickson J, Ross J, Vöö S (2019) Quantitative SPECT: the time is now. EJNMMI Phys 6:1–7
Nakahara T, Owaki Y, Shindou T et al (2019) Bone SPECT-based segmented attenuation correction for quantitative analysis of bone metastasis (B-SAC): comparison with CT-based attenuation correction. EJNMMI Res 9:1–10
Havel M, Dedek V, Kolacek M et al (2022) Quantitative analysis in parathyroid adenoma scintigraphy. Nucl Med Commun 43:1–7
Fraker DL, Harsono H, Lewis R (2009) Minimally invasive parathyroidectomy: benefits and requirements of localization, diagnosis, and intraoperative PTH monitoring long-term results. World J Surg 33:2256–2265
Suh HY, Na HY, Park SY et al (2020) The usefulness of maximum standardized uptake value at the delayed Phase of 99m Tc- sestamibi single-photon emission computed tomography/computed tomography for identification of parathyroid adenoma and hyperplasia. Medicine. https://doi.org/10.1097/MD.0000000000021176
Zhang M, Sun L, Rui W et al (2019) Semi-quantitative analysis of 99mTc-sestamibi retention level for preoperative differential diagnosis of parathyroid carcinoma. Quant Imaging Med Surg 9:1394–1401
Cheon M, Choi JY, Chung JH et al (2011) Differential findings of 99m Tc- Sestamibi dual-phase parathyroid scintigraphy between benign and malignant parathyroid lesions in patients with primary hyperparathyroidism. Nucl Med Mol Imaging 45:276
Acknowledgements
Authors acknowledge the contributions of technologists and radiochemist at the Department of Nuclear Medicine, AECH-NORI for their kind support in the execution and completion of the research study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Sidra Bashir, Shazia Fatima and Ambreen Khawar contributed in the design and execution of the study; All the authors contributed equally in drafting or revising of the manuscript critically for important intellectual content as well as final manuscript approval for submission and publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures were followed in accordance with the ethical standards of the institutional review board; Research Training and Monitoring Cell (RTMC) of NORI, in January 2022 and therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and all subsequent revisions.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for the publication of the images in Figs. 1, 2, 3, 4 and 5.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bashir, S., Fatima, S., Ammar, A. et al. Quantitative analysis in Parathyroid scintigraphy: [99mTc]Tc-MIBI SPECT/CT a tool for noninvasive characterization of parathyroid lesions. Clin Transl Imaging 12, 81–89 (2024). https://doi.org/10.1007/s40336-023-00590-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-023-00590-4