Abstract
Introduction
Pangenotypic direct-acting antivirals are expected to cure hepatitis C virus (HCV) in more than 95% of treated patients. However, data on the effectiveness and safety of sofosbuvir/velpatasvir (SOF/VEL) in Taiwan are limited. This study aims to characterize the patient population in the nationwide Taiwan Association for the Study of the Liver (TASL) HCV Registry and evaluate treatment outcome in Taiwanese patients receiving SOF/VEL.
Methods
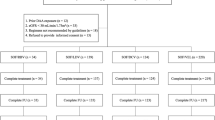
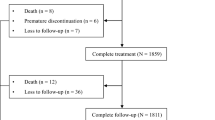
This study was a retrospective-prospective, observational, multicenter, real-world analysis. Adults with chronic hepatitis C were treated with SOF/VEL 400/100 mg ± ribavirin for 12 weeks. The primary outcome was sustained virologic response 12 weeks after end of therapy (SVR12). Factors associated with not achieving SVR12 were evaluated using logistic regression and covariate analysis. Safety was also assessed.
Results
In total, 3480 patients were included: 86.8% genotype 1/2, 2.8% genotype 3, 0.1% genotype 4/5, 9.6% genotype 6; unclassified, 0.8%; 12.2% compensated cirrhosis; 3.3% decompensated cirrhosis; and 15.8% chronic kidney disease. Overall SVR12 rate was 99.4% (genotype 1, 99.5%; genotype 2, 99.4%; genotype 3, 96.9%; genotype 4, 100%; genotype 6, 99.7%). SVR12 rates among patients with compensated cirrhosis, decompensated cirrhosis, and chronic kidney disease stages 4–5 were 99.5%, 100%, and 100%, respectively. There were 21 patients (0.6%) who did not achieve SVR12. Factors associated with failure were treatment adherence below 60%, high viral load, and genotype 3 (p < 0.001, p = 0.028, and p = 0.001, respectively). Adverse events occurred in 10% of patients; 0.6% were serious and one was related to treatment. Treatment discontinuation occurred in 0.3% of patients; none were treatment related. The estimated glomerular filtration rate remained stable throughout treatment and follow-up, regardless of baseline values and cirrhosis status.
Conclusion
SOF/VEL was highly effective and well tolerated in Taiwanese patients, irrespective of viral genotype, liver disease severity, and comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Data on hepatitis C virus (HCV) treatment in certain populations in Taiwan are limited. |
Data on HCV treatment with sofosbuvir/velpatasvir (SOF/VEL) from large-scale real-world settings in Taiwan are limited. |
Efficacy and safety of SOF/VEL was analyzed in 3480 patients using a nationwide HCV database. |
What was learned from this study? |
Overall, 99.4% of patients with HCV treated with SOF/VEL, with and without ribavirin, achieved cure, regardless of baseline characteristics and patient population. |
Treatment with SOF/VEL was well tolerated in those with severe liver disease and comorbidities. |
Treatment with SOF/VEL did not worsen kidney function in patients with HCV and chronic kidney disease. |
Introduction
Hepatitis C virus (HCV) is a global public health concern, with over 71 million people infected around the world. Chronic HCV is recognized as a common cause of cirrhosis, hepatocellular carcinoma (HCC), liver transplantation, and liver-related deaths [1]. Since the introduction of direct-acting antivirals (DAAs), the expectation is that 95% of treated patients will be cured of HCV—defined as a sustained virologic response 12 weeks after the end of therapy (SVR12) [2]. Achieving SVR12 is associated with a decreased risk of liver disease progression and its complications, including liver decompensation, portal hypertension, and death [3, 4].
Sofosbuvir/velpatasvir (SOF/VEL), a protease inhibitor (PI)-free 12-week regimen for patients with chronic HCV, has demonstrated SVR12 rates of 95–100% in over 1100 clinical trial patients with HCV genotypes 1–6 [5,6,7]. Efficacy in clinical trials has translated into effectiveness in clinical practice, evidenced through multiple real-world studies [8,9,10]. Clinical trials in an Asian population have shown similar results to those in western parts of the world [25].
HCV populations have more comorbidities that may aggravate the progression of fibrosis, such as obesity and insulin resistance and coinfection with HIV or HBV. The development of hepatic and extrahepatic diseases, such as circulatory disease and renal disease, can lead to increased mortality in patients with chronic HCV [26]. In Taiwan, the most common comorbidities are diseases of the digestive system (40.1%), circulatory system (38.7%), and endocrine/nutritional/metabolic diseases (35.2%). These diverse comorbidities in the Taiwanese population are reflected in this current cohort and it is encouraging that high SVR12 rates were achieved with SOF/VEL in persons who inject drugs (99.5%), patients with active HCC (98.5%), and those coinfected with HBV (98.8%) or HIV (96.9%). This suggests that SOF/VEL was well tolerated in patients with comorbidities and these rates of cure match or exceed those of previous clinical and real-world studies [27,28,29].
Currently, there is a large gap in data on the effectiveness and safety of SOF/VEL in patients with decompensated cirrhosis in Taiwan. As the use of PI-based regimens is contraindicated in patients with decompensated cirrhosis, such data are essential for guiding patients and physicians in treatment decision-making and advising healthcare policies on treatment coverage. To the best of our knowledge, this is the largest cohort study on the efficacy and safety of SOF/VEL treatment in patients with decompensated cirrhosis in Taiwan. The high SVR12 rates achieved in this patient group in this study (100% of 114 patients) demonstrate the high effectiveness and value of a PI-free regimen, such as SOF/VEL, in this patient group.
In patients who did not achieve SVR12, HCV RNA viral load over 6,000,000 IU/mL and HCV genotype 3 infection were the factors found to be significantly associated with the risk of not achieving SVR12. However, as only three patients with genotype 3 did not achieve SVR in the TACR cohort, and all patients with genotype 3 and high viral load achieved cure, this statistically significant difference is unlikely to have a clinical impact, especially given that the majority of the chronic HCV population in Taiwan is infected with genotype 1 or 2 (as also reflected in this cohort). Despite having a very low cutoff value for drug adherence (the SIMPLIFY study quantified low adherence as below 90% [30]), the majority of patients (5/9) with adherence below this 60% threshold achieved SVR12 with SOF/VEL. However, adherence is important to ensure treatment effectiveness.
As the metabolite of SOF is renally cleared, SOF-based regimens were previously not recommended in patients with severely impaired renal function (CKD stage 4 or 5, eGFR < 30 mL/min/1.73 m2). However, despite elevated plasma levels of sofosbuvir and its metabolite GS-331007 in patients with renal impairment, increasing evidence supports the safety and effectiveness of SOF-based regimens in this patient population [31, 32], including those with liver cirrhosis [32] and uremic patients on dialysis [33]. In November 2019, the US Food and Drug Administration (FDA) amended the package inserts for SOF-based regimens to allow use in patients with renal disease, including those with an eGFR < 30 mL/min/1.73 m2 and those on dialysis, and the Taiwan consensus statement on the management of hepatitis C recommends SOF/VEL as one of the treatment options for patients with stage 4 or 5 CKD [17]. This is supported by data from this cohort that demonstrated a lack of fluctuation in eGFR levels across some CKD stages and, notably, all patients with CKD stage 4 achieved SVR12. In patients with eGFR < 90 mL/min/1.73 m2 and cirrhosis, eGFR increased significantly, showing that not only could renal function deterioration be halted but it could also be improved in some patient groups typically seen as “difficult to cure”.
The majority of patients tolerated treatment well with only 10% of patients experiencing adverse events and 0.6% experiencing serious adverse events, the majority of which were experienced in the ribavirin-added group. Only three patients discontinued treatment as a result of adverse events and these were not considered to be related to SOF/VEL therapy. It should be noted that the adverse events observed could be due to ribavirin or the severity of disease. Although, with the high SVR12 rates achieved irrespective of ribavirin, it raises the question whether a simplified therapy without ribavirin would be more beneficial. This has been highlighted by a recent phase 3 trial from Japan that demonstrated SOF/VEL without ribavirin was highly effective and well tolerated in patients with decompensated cirrhosis. The study found the addition of ribavirin did not improve efficacy, but increased toxicity [34].
There were limitations identified in this cohort study. First, this was a retrospective-prospective study, where patients treated with SOF/VEL before February 2021 were eligible for inclusion. However, the data analyzed were obtained prospectively in accordance with the regulations of Taiwan’s Health Insurance Administration for DAA therapy. Second, as a result of limited numbers of certain types of patients, such as patients with HCV genotypes 4 and 5, the treatment outcomes for those patients may be lacking. Despite these limitations, the TACR includes data from patients treated at a range of settings across Taiwan, including medical centers, regional hospitals, and local clinics. Furthermore, as no specific exclusion criteria were applied to the study population, this is a true reflection of the real-world management of patients with chronic hepatitis C in this country.
Conclusion
A simple, pangenotypic, protease inhibitor-free treatment that results in high SVR12 rates with and without ribavirin, regardless of genotype, cirrhosis, severity of liver disease, and comorbidities is of value in Taiwan and across Asia. The confirmation of the high SVR12 rates with SOF/VEL with and without ribavirin supports use of this regimen in a more diverse population, including those with decompensated cirrhosis and CKD.
References
Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2:161–71.
European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: final update of the series. J Hepatol. 2020;73:1170–218.
Backus LI, Boothroyd DB, Phillips BR, Belperio P, Halloran J, Mole LA. A sustained virologic response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509–16.
van der Meer A, Veldt B, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584–93.
Feld J, Jacobson IM, Hézode C, et al. Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. N Engl J Med. 2015;373:2599–607.
Foster G, Afdhal N, Roberts S, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608–17.
Curry M, O’Leary J, Bzowej N, et al. Sofosbuvir and velpatasvir for HCV in patients with decompensated cirrhosis. N Engl J Med. 2015;373:2618–28.
Mangia A, Milligan S, Khalili M, et al. Global real-world evidence of sofosbuvir/velpatasvir as simple, effective HCV treatment: analysis of 5552 patients from 12 cohorts. Liver Int. 2020;40:1841–52.
Belperio P, Shahoumian T, Loomis T, Mole L, Backus L. Real-world effectiveness of daclatasvir plus sofosbuvir and velpatasvir/sofosbuvir in hepatitis C genotype 2 and 3. J Hepatol. 2019;70:15–23.
Buggisch P, Wursthorn K, Stehr A, et al. Real-world effectiveness and safety of sofosbuvir/velpatasvir and ledipasvir/sofosbuvir hepatitis C treatment in a single centre in Germany. PLoS ONE. 2019;14: e0214795.
Wei L, Lim SG, **e Q, et al. Sofosbuvir–velpatasvir for treatment of chronic hepatitis C virus infection in Asia: a single-arm, open-label, phase 3 trial. Lancet Gastroenterol Hepatol. 2019;4:127–34.
Yang J-F, Lin C-I, Huang J-F, et al. Viral hepatitis infections in southern Taiwan: a multicenter community-based study. Kaohsiung J Med Sci. 2010;26:461–9.
Yu M-L, Yeh M-L, Tsai P-C, et al. Huge gap between clinical efficacy and community effectiveness in the treatment of chronic hepatitis C: a nationwide survey in Taiwan. Medicine. 2015;94:e690.
Bennet H, Waser N, Johnston K, et al. A review of the burden of hepatitis C virus infection in China, Japan, South Korea and Taiwan. Hepatol Int. 2015;9:378–90.
Yu M-L, Chuang W-L. Treatment of chronic hepatitis C in Asia: when East meets West. Hepatology. 2009;24:336–45.
Lu M-Y, Chen C-T, Shih Y-L, et al. Changing epidemiology and viral interplay of hepatitis B, C and D among injecting drug user-dominant prisoners in Taiwan. Sci Rep. 2021;11:8554.
Yu M-L, Chen PJ, Dai CY, et al. 2020 Taiwan consensus statement on the management of hepatitis C: Part (II) special populations. J Formos Med Assoc. 2020;119:1135–57.
Chen CY, Huang CF, Cheng PN, et al. Factors associated with treatment failure of direct-acting antivirals for chronic hepatitis C: a real-world nationwide hepatitis C virus registry programme in Taiwan. Liver Int. 2021;41:1265–77.
Liu CH, Huang YJ, Yang SS, et al. Generic sofosbuvir-based interferon-free direct acting antiviral agents for patients with chronic hepatitis C virus infection: a real-world multicenter observational study. Sci Rep. 2018;8:13699.
Kowdley KV, Gordon SC, Reddy KR, et al. Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N Engl J Med. 2014;370:1879–88.
Liu CH, Chen PY, Chen JJ, et al. Sofosbuvir/velpatasvir for patients with chronic hepatitis C virus infection and compensated liver disease: real-world data in Taiwan. Hepatol Int. 2021;15:338–49.
Jacobson IM, Lawitz E, Gane EJ, et al. Efficacy of 8 weeks of sofosbuvir, velpatasvir and voxilaprevir in patients with chronic HCV infection: two phase 3 randomized trials. Gastroenterology. 2017;153:113–22.
Smith D, Magri A, Bonsall D, et al. Resistance analysis of genotype 3 hepatitis C virus indicates subtypes inherently resistant to nonstructural protein 5A inhibitors. Hepatology. 2019;69:1861–71.
Hsieh M-H, Tsai J-J, Hsieh M-Y, et al. Hepatitis C virus infection among injection drug users with and without human immunodeficiency virus co-infection. PLoS ONE. 2014;9(4): e94791.
Solomon S, Wagner-Cardoso S, Smeaton L, et al. The “keep it simple and safe” approach to HCV treatment: primary outcomes from the ACTG A5360 (MINMON) study. Presented at the AASLD 2020 Liver Meeting Digital Experience; November 11–16, 2020. Abstract LO7.
Yu M-L, Chen PJ, Dai CY, et al. 2020 Taiwan consensus statement on the management of hepatitis C: part (I) general population. J Formos Med Assoc. 2020;119:1019–40.
Wyles D, Bräu N, Kottilil S, et al. Sofosbuvir and velpatasvir for the treatment of hepatitis C virus in patients coinfected with human immunodeficiency virus type 1: an open-label, phase 3 study. Clin Infect Dis. 2017;65:6–12.
Yeh M-L, Huang C-F, Huang C-I, et al. Hepatitis B-related outcomes following direct-acting antiviral therapy in Taiwanese patients with chronic HBV/HCV co-infection. J Hepatol. 2020;71:62–71.
Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153–61.
Cunningham EB, Amin J, Feld J, et al. Adherence to sofosbuvir and velpatasvir among people with chronic HCV infection and recent injection drug use: the SIMPLIFY study. Int J Drug Policy. 2018;62:14–23.
Eletreby R, El-Serafy M, Anees M, et al. Sofosbuvir-containing regimens are safe and effective in the treatment of HCV patients with moderate to severe renal impairment. Liver Int. 2019;40:797–805.
Liu C-H, Chen C-H, Su W-W, et al. Sofosbuvir/velpatasvir with or without low-dose ribavirin for patients with chronic hepatitis C virus infection and severe renal impairment. Gut. 2022;71:176–84.
Yu M-L, Huang C-F, Wei Y-J, et al. Establishment of an outreach, grou** healthcare system to achieve microelimination of HCV for uremic patients in haemodialysis centres (ERASE-C). Gut. 2021;70:2349–58.
Takaoka Y, Miura K, Morimoto N, et al. Real-world efficacy and safety of 12-week sofosbuvir/velpatasvir treatment for patients with decompensated liver cirrhosis caused by hepatitis C virus infection. Hepatol Res. 2022;71:176–84.
Acknowledgements
Funding
The study was partly supported by grants from Kaohsiung Medical University (MOST 109-2314-B-037-044, KMU-K1110002, MOST 108-2314-B-037-066-MY3, KMU-TC108B06 [Center for Liquid Biopsy], KMU-TC108B07 & KMU-DK109002 [Cohort Research Center], 105KMUOR08 [Center for Cancer Research KMU Global Networking Talent Plan Grant], and KMU-TC109B05 [Center for Liquid Biopsy and Cohort Research]) and Kaohsiung Medical University Hospital (KMUH109-9R06, KMUH109-9R05, MOHW109-TDU-B-212-114006 and KMUH-IIT-109-2-05). The journal’s Rapid Service Fee is funded by Gilead Sciences Hong Kong Ltd.
Medical Writing Assistance
Medical writing assistance was provided by Ridda Jabbar and Julia Heagerty from Elements Communications Ltd, United Kingdom, funded by Gilead Sciences Hong Kong Ltd. Gilead had no control over the final content of this manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Ming-Lung Yu, Han-Chieh Lin and Pin-Nan Cheng were responsible for the study conception and design, all authors contributed to the study design and data collection, and analyses were performed by Ming-Lung Yu, Han-Chieh Lin and Pin-Nan Cheng. All authors reviewed early drafts of the manuscript and read and approved the final version for publication.
Prior Presentation
Part of this work was presented at the International Symposium on Viral Hepatitis and Liver Disease Global Hepatitis Summit held between June 17 and June 20, 2021, in Taipei, Taiwan. #P204.
Disclosures
Pin-Nan Cheng: Advisory board for AbbVie, Gilead Sciences, and Merck Sharp & Dohme. Speaker for Abbott, AbbVie, Gilead Sciences, and Merck Sharp & Dohme. Research grants from Gilead Sciences and Merck Sharp & Dohme. Jia-Horng Kao: Speaker, consultant and/or advisory board member for AbbVie, Arbutus Biopharma, Bristol Myers Squibb, Fujirebio, Gilead Sciences, Johnson & Johnson, MSD, Polaris, Sysmex and Roche. Ming-Lung Yu: Research support (grant) from Abbott, BMS, Gilead Sciences and Merck Sharp & Dohme. Consultant of AbbVie, Abbott, BMS, Gilead Sciences, Merck Sharp & Dohme, and Roche Diagnostics. Speaker for AbbVie, Abbott, BMS, Gilead Sciences, IPSEN, Merck Sharp & Dohme and Roche. Chung-Feng Huang: Speaker for AbbVie, BMS, Gilead Sciences, Merck Sharp & Dohme, and Roche. Chen-Hua Liu: Advisory board for AbbVie, Gilead Sciences, and Merck Sharp & Dohme. Speaker for Abbott, AbbVie, Gilead Sciences, and Merck Sharp & Dohme. Research grants from AbbVie, Gilead Sciences, and Merck Sharp & Dohme. All other authors (Lein-Ray Mo, Chun-Ting Chen, Chi-Yi Chen, Hsing-Tao Kuo, Ching-Chu Lo, Kuo-Chih Tseng, Yi-Hsiang Huang, Chi-Ming Tai, Cheng-Yuan Peng, Ming-Jong Bair, Chien-Hung Chen, Ming-Lun Yeh, Chih-Lang Lin, Chun-Yen Lin, Pei-Lun Lee, Lee-Won Chong, Chao-Hung Hung, Te Sheng Chang, Jee-Fu Huang, Chi-Chieh Yang, Jui-Ting Hu, Chih-Wen Lin, Chia-Chi Wang, Wei-Wen Su, Tsai-Yuan Hsieh, Chih-Lin Lin, Wei-Lun Tsai, Tzong-Hsi Lee, Guei-Ying Chen, Szu-Jen Wang, Chun-Chao Chang, Sheng-Shun Yang, Wen-Chih Wu, Chia-Sheng Huang, Kwok-Hsiung Chou, Chien-Neng Kao, Pei-Chien Tsai, Mei-Hsuan Lee, Chien-Yu Cheng, Ming-Chang Tsai, Chun-Jen Liu, Chia-Yen Dai, Han-Chieh Lin, Wan-Long Chuang): Nothing to disclose.
Compliance with Ethics Guidelines
Ethics approval was granted by Kaohsiung Medical University Chung-Ho Memorial Hospital (IRB number KMUHIRB-F(I)-20170053).
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Contributors
The authors would also like to thank the Taiwan Association for the Study of the Liver (TASL), the TASL Foundation, and Taiwan Liver Research Foundation for grant support and the TACR study group for data collection. We also thank the Center for Medical Informatics and Statistics of Kaohsiung Medical University for providing administrative and funding support.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cheng, PN., Mo, LR., Chen, CT. et al. Sofosbuvir/Velpatasvir for Hepatitis C Virus Infection: Real-World Effectiveness and Safety from a Nationwide Registry in Taiwan. Infect Dis Ther 11, 485–500 (2022). https://doi.org/10.1007/s40121-021-00576-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-021-00576-7