Abstract
Introduction
In vitro and pre-marketing clinical data have shown the healing properties of a postbiotic extract from Aquaphilus dolomiae (ADE-G2). The effectiveness and tolerability of an ADE-G2-based cream were therefore evaluated for the management of minor skin impairment and wound healing in a large population of subjects in routine clinical practice.
Methods
A real-world, international, pre-post comparative study was conducted in infants, children, and adults with various types of superficial skin impairment who used the study product daily for around 3 weeks according to their dermatologist’s advice. Immediate and follow-up changes in dermatologic signs and symptoms were assessed through clinical scoring. User satisfaction, overall product effectiveness, and tolerability were also evaluated. Analyses were performed in the whole study population and in subject subgroups according to skin impairment type and age.
Results
Overall, 1317 subjects (83.1% adults, 72.0% female) were included. Dermatologists reported effectiveness and “good” or “very good” tolerability of the cream in 93.8% (1221/1302) and 98.5% (1278/1297) of subjects, respectively. Immediate symptom relief after the first application was reported by 88.3% (849/962) of subjects. After several weeks of regular use (16.7 ± 11.6 days), dermatologic signs and symptoms significantly improved in the whole study population and in the subgroups, with mean decreases in severity scores ranging from –34.5% to –92.5% (p < 0.0001). The smallest improvements were found in subjects with oncologic treatment-related skin impairment. At study end, most users (> 95%) were “very satisfied” or “satisfied” with the cream and found that skin healing was rapid and of good quality.
Conclusion
The ADE-G2-based cream proved to be effective and well tolerated in real-life conditions for the management of minor skin impairment in a large and varied cohort of subjects. This product, used as a standalone or adjunctive regimen, can help accelerate the healing of various types of superficial skin impairment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Specific topical products are available to enhance healing of minor skin impairment, such as common types of dermatologic conditions and wound healing, and cutaneous impairment caused by dermatologic interventions or triggered by oncologic treatments |
This international, real-world, pre–post comparative study aimed to investigate the effectiveness and tolerability of a cream containing a postbiotic extract used in general practice in infants, children, and adults for improving skin healing |
What was learned from the study? |
This repairing cream significantly reduced the severity of dermatologic clinical signs (erythema, edema, oozing, and scabs) and symptoms (burning sensations, tingling, tightness, pruritus, and pain) in the whole study population after a mean daily use of around 17 days |
The product is safe to be used daily, as a standalone skin care regimen or as an adjunct to other medical treatments or dermocosmetics, to help improve skin healing and recovery in subjects of all ages |
Introduction
When the skin is irritated or has been injured, hel** the natural process of skin repair may be useful for optimizing wound healing and preventing complications. Several solutions are available for healing skin but most are based on mechanical approaches that involve protecting the damaged areas from irritation with dressings [1, 2]. Topical products containing healing and antibacterial ingredients can also be used during the early phase of wound healing, both to accelerate skin repair by attracting growth factors to the injured site and to prevent healing from being compromised by secondary infections [3, 4]. The development of topical skin repair products with enhanced properties is of great interest for offering safe and more effective solutions for management of wound healing or the most common types of minor dermatologic conditions that impair the skin barrier in a wide range of populations, including infants, children, adults, and older people.
Recent findings have highlighted the major role of the microbiota in the regeneration process of the intestinal epithelium [5, 6]. Indeed, a direct link has been identified between the various stimulatory molecules secreted by the gut bacteria and the constant process of intestinal epithelial cell renewal. Among these stimulatory factors, flagellin, the main structural protein of the bacterial flagellum, has been shown to bind to specific cell surface receptors (i.e., Toll-like receptor 5; TLR5), and activate signaling pathways involved in cell proliferation and migration [7,8,9]. TLR5-flagellin interactions have also been found to enhance the innate defense mechanism of the mucosa by stimulating the production of antimicrobial peptides (AMPs) [7]. AMPs also have the ability to directly stimulate the proliferation of epithelial cells and consequently promote wound healing [10]. These data therefore indicate that the flagellin-mediated mechanism is part of the healing process of the intestinal wall and thereby contributes to its homeostasis.
Based on this regulatory mechanism of the gut epithelium, a postbiotic extract enriched in flagellin has been produced from Aquaphilus dolomiae, a flagellated bacterium that is found specifically in Avène thermal spring water [11], to develop an innovative bioactive with healing potential, the ADE-G2 or C+-Restore™ extract (Avène Laboratories, France). This extract has demonstrated in vitro stimulatory effects on keratinocyte migration and fibroblast proliferation, as well as on the synthesis of AMPs, such as human beta-defensin-2 (hBD-2) [12]. The ADE-G2 extract has also been shown to significantly accelerate re-epithelization in an ex vivo wounded skin model, even at low concentrations. These results, supporting both the skin restorative and antimicrobial properties of the ADE-G2 extract, have led to the development of several topical formulations incorporating this active ingredient, along with other well-known antibacterial compounds (such as copper and zinc sulfate), for use as dermocosmetics with enhanced healing properties for a wide range of minor skin impairment and wound healing.
Pre-marketing clinical evaluations have provided excellent results concerning the beneficial effects and good tolerability of these ADE-G2-based products (unpublished observations). The aim of the current study was to assess the real-world effectiveness and tolerability of an ADE-G2-containing cream for the management of wound healing and minor dermatologic conditions that impact the skin barrier in a large international cohort of adult and pediatric subjects. This study evaluated the immediate and 3-week effects of the cream on various dermatologic clinical signs and symptoms in the whole study population, as well as in subpopulations of subjects grouped according to the type of skin impairment. Secondary analyses were performed in subgroups according to age category, frequency of product application, and type of regimen. Overall product effectiveness, tolerability, and user satisfaction were also assessed.
Methods
Study Design and Ethics
This real-world, prospective, observational, multicenter, pre-post comparative study was conducted from 15 September 2020 to 3 January 2023 in seven countries (France, the United States, Chile, Germany, Costa Rica, the Czech Republic, and Slovakia). The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments and complied with good clinical practice guidelines (CPMP/ICH/135/95, https://www.ema.europa.eu) and the current legislation for clinical trials with cosmetics in the countries where the study was conducted [Regulation (EC) No. 1223/2009 of the European Commission for the European countries]. This noninterventional study evaluated a cosmetic product administered as part of the usual practice of the physicians and involved no constraints or invasive examinations. Therefore, approval of the protocol by an ethics committee or an institutional review board was not required in the countries participating in the study, in accordance with their current legislation in 2020. The included subjects, or their parents or guardians for subjects < 18 years old, received a leaflet in their native language containing details about the study and their rights, including the processing of their personal data and their right to access and modify their personal data, in accordance with Regulation (EU) No. 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons. All included subjects, or their parents or guardians, provided oral or written consent to take part in the study.
Study Product
The study product was a commercially available dermocosmetic, the Cicalfate+® skin repairing protective cream (Avène, France) containing the postbiotic extract ADE-G2 (C+-Restore™) as the main active ingredient and Avène thermal spring water (Avène aqua), caprylic/capric triglyceride, mineral oil (paraffinum liquidum), glycerin, hydrogenated vegetable oil, zinc oxide, propylene, glycol, polyglyceryl-2 sesquiisostearate, PEG-22/dodecyl glycol copolymer, aluminum stearate, arginine, beeswax (cera alba), copper sulfate, magnesium stearate, magnesium sulfate, microcrystalline wax (cera microcristallina), tromethamine, and zinc sulfate.
Participants
Dermatologists or onco-dermatologists were invited by the sponsor to participate in the study. Those agreeing to participate were asked to recruit at least five subjects (infants, children, or adults) for whom use of the study product was advised according to the product leaflet. Pregnant or breastfeeding women, subjects with known sensitivity to one of the ingredients of the study cream, subjects with another condition that might interfere with assessment of the clinical outcomes, or those participating or having participated in an interventional clinical study in the past month were not included.
Study Procedure
The study involved two visits: an inclusion visit (Visit 1) and a follow-up visit (Visit 2) after about 3 weeks of product use. These visits were part of the routine follow-up of the subjects by their dermatologist. At inclusion, dermatologists collected demographic and clinical data from the subjects, including the type(s) and the location(s) of the skin impairment, and concomitant treatments. Instructions for use of the study cream were provided by the dermatologist to the subjects according to their usual practice, without any specific recommendations from the sponsor. The participating subjects, or their parents or guardians, were asked to apply the cream at Visit 1 (first application) and then at home in compliance with the dermatologist’s advice, i.e., once, twice, or three times daily to the area concerned for about 3 weeks. This regimen could be added to a medical treatment (antiseptic, antibiotic, or antifungal products) or other dermocosmetic products (antibacterial cleansers or sunscreens) when appropriate.
Evaluation Criteria
The main evaluation criterion was the effectiveness of the study product on objective dermatologic clinical signs, as assessed by the dermatologist at follow-up. The secondary criterion was the effectiveness of the study product on subjective dermatologic clinical symptoms, assessed by the subjects, or their parents or guardians, immediately after product use and at follow-up. Additional outcomes included assessment of which symptoms the subjects perceived to have improved or not, the mean time to any subject-perceived improvements in symptoms, user satisfaction, and product tolerability. These criteria were analyzed in the whole study population and in subpopulations of subjects grouped according to the type of skin impairment (see Table 1). The two main criteria and product tolerability were also analyzed in subgroups according to age category, frequency of product application, and regimen type.
Assessment Methods
Clinical Signs
The dermatologist assessed the severity of clinical signs related to skin impairment at baseline (Visit 1) and at follow-up (Visit 2) using a 4-point visual analog scale (VAS) from 0 (none) to 3 (severe) on four items (erythema, edema, oozing, and scabs), and the sum of the four individual scores was used to obtain the total severity score (maximum score: 12) for each subject. The physician also assessed the global effectiveness of the product using a single-item questionnaire comprising four possible answers: very effective, effective, moderately effective, and not effective at all.
Clinical Symptoms
The subjects, or their parents or guardians, assessed the severity of dermatologic clinical symptoms at baseline, after the first product application (Visit 1) and at follow-up (Visit 2) using a 4-point VAS from 0 (none) to 3 (severe) on five items (burning sensations, tingling, tightness, pruritus, and pain). The total severity score was calculated as the sum of the five individual scores, with a maximum possible score of 15. At Visit 2, the subjects, or their parents or guardians, were also asked to indicate which symptoms they considered to have improved or not (scabs, redness, itching, tightness, burning sensation, tingling, swelling, pain, and oozing) and to estimate the mean time to any improvements.
User Satisfaction
As part of the follow-up questionnaire, the subjects, or their parents or guardians, were asked to assess their global satisfaction with the product and to evaluate its cosmetic properties according to four parameters (ease and comfort of application, speed and quality of repair/healing) by choosing one answer among four propositions: very satisfied, satisfied, not satisfied, and not at all satisfied.
Tolerability
Tolerability was rated by the dermatologist at Visit 2 using a 4-point scale from very good to poor tolerance. The subjects also reported any acceptability issues they encountered when using the study cream.
Statistical Analyses
Quantitative variables were expressed as the mean, standard deviation (SD), and range (min-max), and qualitative variables were described as numbers and percentages (N and %) for the different categories. Between-visit differences in the means were expressed as absolute changes (initial value – final value) and relative changes (initial value – final value/initial value × 100). Changes in score from baseline were analyzed in the whole study population and in the different subgroups of subjects using the nonparametric paired Wilcoxon test. Inter-group comparisons were performed with the Kruskall-Wallis or Wilcoxon test. A p value < 0.05 was considered statistically significant. All statistical analyses were carried out using SAS®, version 9.4.
Results
Participants and Baseline Characteristics
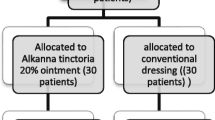
Of the 1889 subjects recruited by 186 dermatologists or oncologists, 1317 subjects with dermocosmetic indications could be included and thus constituted the whole study population (Fig. 1). Subjects with medical indications were excluded because of the dermocosmetic status of the study product. Baseline demographic and clinical characteristics of the included subjects are presented in Table 1: 83.1% were adults and 72.0% were female. Their age ranged from 0 to 91 years (median of 44 years). The most common location of the skin impairment was on the face (49.6% of the subjects). Other sites reported in > 5% of subjects included the torso, genital areas, the neckline, hands, upper limbs, and lower limbs. Mean severity scores for clinical objective signs (3.8/12) and subjective symptoms (5.7/15) indicated mild to moderate skin impairment at baseline.
For the main analysis, three subject subgroups were defined according to the type of skin impairment (Table 1): subjects with common types of dermatologic conditions or wound healing (43.1%), e.g., perioral dermatitis, angular cheilitis, non-oozing diaper rash, or superficial wounds or burns; those with cutaneous impairment due to previous surgery or dermatologic procedures (42.5%); and those with skin impairment due to oncologic treatments (14.4%). Details of the types of skin impairment in each subgroup are provided in Table S1. For secondary analyses, we also defined four subgroups according to age (Table 1): infants (0–23 months) and children (2–17 years), who mostly had common types of dermatologic conditions or wound healing (97.4% and 86.1%, respectively), mainly non-oozing diaper rash and perioral dermatitis, and adults (18–64 years) and seniors (≥ 65 years), who mostly had skin impairment due to previous surgery or dermatologic procedures (49.0% and 50.7%, respectively) (Table S3).
Study Product Use
Almost all subjects (99.2%, 1300/1311) received advice on the frequency of use of the study product from their dermatologist and used the study product accordingly: 13.0% of subjects (168/1290) reported that they applied the ADE-G2-based cream once a day, 60.5% (780/1290) twice a day, and 26.5% (342/1290) three or more times a day. Based on the self-evaluation performed by 1258 subjects, the mean duration of product use was 16.7 ± 11.6 days. The study product was used in combination with other products in 36.1% (475/1317) of subjects (Table 1): medical treatments in 20.4% of subjects (269/1317) and dermocosmetics in 24.4% of subjects (322/1317). Considering the different conditions of product use, we performed additional secondary analyses of the main criteria in subgroups according to the frequency of product application (once, twice, and three or more times daily) and the type of regimen (study product used alone or in combination).
Product Effectiveness on Objective Clinical Signs
In the whole study population, statistically significant decreases between baseline and follow-up were observed in the mean total (– 79.0% decrease, p < 0.0001; Fig. 2a) and individual sign severity scores (Table 2). Moreover, overall improvement in objective clinical signs was reported in 83.5% of subjects (982/1176). Significant decreases in mean severity scores were also found in the three subgroups according to skin impairment type (p < 0.0001, Table 2), but subjects with skin impairment due to oncologic treatments reported the smallest decrease (– 39.1% vs – 79.5% to – 81.1%, between-group comparison p < 0.0001). This subgroup also had the lowest total and individual severity scores at baseline and the lowest percentage of subjects with an improved total score (52.0% vs 83.2% to 93.3%, p < 0.0001, Table 2). Improvement in clinical signs was also observed in all subgroups according to the frequency of product application (p < 0.0001), although a slightly lower rate of improvement was found in the once-daily application subgroup (75.7% vs 81.7% to 85.8%, p < 0.0001, Table S6). Otherwise, the rate of improvement in subjects was high in all age categories (Table S4) and regimen types (Table S7), with values ranging from 81.3% to 95.4%.
Effectiveness of the ADE-G2-based cream on objective dermatologic clinical signs and overall product effectiveness. a Changes in mean total severity score (scale from 0 to 12) and percentage differences in this score between baseline and follow-up in the whole study population (all types) and in the three subgroups according to the type of skin impairment. The mean score significantly decreased between baseline and follow-up in all groups. **p < 0.0001 (paired Wilcoxon test). b Overall product effectiveness at follow-up in the whole study population (all types) and in the three subgroups according to the type of skin impairment. The cumulated percentage of subjects who rated the study product as “very effective” or “effective” is indicated for each group
At study end, the dermatologists reported good product effectiveness in 93.8% of subjects (1221/1302; Fig. 2b and Table S2). The effectiveness rate was similar regardless of the type of skin impairment: the cumulated percentage of subjects with a study product rating of “very effective” or “effective” ranged from 91.7% to 96.4% across the skin impairment type subgroups. In addition, there were no major differences in overall effectiveness according to age category (Table S5), frequency of product application (Table S6), or regimen type (Table S7), with the cream being rated as effective in 84.4% to 94.5% of subjects across all subgroups.
Product Effectiveness on Subjective Clinical Symptoms
The first application of the ADE-G2-based cream had an immediate relieving effect in 88.3% of subjects (849/962, Table 2). Significant decreases from baseline were also found in mean subjective clinical symptom scores, with decreases in total severity score of –49.1% at the first product application and of – 84.2% at follow-up in the whole study population (p < 0.0001, Fig. 3a and Table 2). At follow-up, improvements in subjective clinical symptoms were also reported in 85.8% of subjects (993/1157). Similar results were found in the skin impairment type subgroups (Fig. 3a), with smaller decreases in severity scores and a lower percentage of subjects with an improved score in the group with skin impairment due to oncologic treatments than in the other two subgroups (55.6% vs 89.0% to 90.7%, between-group comparison p < 0.0001, Table 2). Improvement rates were high in all age subgroups (Table S4) and regimen types (Table S7), with values between 73.2% and 89.8%. The rate of improvement was slightly lower in the subgroup with once daily application compared to twice and more daily applications (71.5% vs 88.1% and 87.0%, p < 0.0001, Table S6).
Effectiveness of the ADE-G2-based cream on subjective dermatologic clinical symptoms and overall user satisfaction. a Changes in mean total severity score (scale from 0 to 15) and percentage differences in this score between baseline and the first product application or follow-up in the whole study population (all types) and in the three subgroups according to the type of skin impairment. The mean score significantly decreased in all groups and at both time points. **p < 0.0001 (paired Wilcoxon test). b Overall user satisfaction at follow-up in the whole study population (all types) and in the three subgroups according to the type of skin impairment. The cumulated percentage of subjects who reported being “very satisfied” or “satisfied” is indicated for each group
Overall, the subjects reported that their symptoms started to improve after a mean time of product use of 6.1 ± 5.0 days (based on data from 1178 subjects), and at study end the vast majority of subjects (90.8%, 1173/1292) reported that the regular use of the ADE-G2-based cream markedly improved all assessed symptoms.
User Satisfaction
Most users (96.6%, 1246/1289) were overall “very satisfied” or “satisfied” with the product (Fig. 3b and Table S2). The satisfaction rate was also high in all the skin impairment type subgroups, with values ranging from 95.5% to 98.0%. Moreover, most subjects found that the cream was easy (97.9%) and agreeable (96.2%) to apply and that the repairing or healing effect was rapid (95.8%) and of good quality (95.9%) (Table S2).
Tolerability
At study end, product tolerability was rated by the dermatologists as “very good” or “good” in 98.5% (1278/1297) of all subjects; this percentage ranged from 97.9% to 99.3% across the skin impairment type subgroups (Table S2). Tolerability did not change according to age category (Table S5), frequency of product application (Table S6), or regimen type (Table S7). Side effects were reported in a small percentage of subjects during product use: between 1.1% (13/1237) and 4.9% (62/1278) according to the dermatologist and self-reported assessments, respectively. The main side effects included redness, tingling, and itching. Some users also found that the cream was too thick and gave the skin a whitish appearance.
Discussion
This multicenter, pre-post comparative study conducted in a very large cohort of subjects with various types of minor skin impairment or wound healing demonstrated that the daily use of the ADE-G2-based cream for around 2–3 weeks in real-life conditions allowed marked improvements in signs and symptoms of most types of skin impairment. The smallest improvements were reported by subjects with skin impairment due to oncologic treatments. According to the users, or their parents or guardians, the effects started to be visible after only 6 days of product use. The frequency of product application of at least twice daily, as recommended in the product leaflet, also appears important to obtain better improvement as subjects with once daily application had significantly lower score decreases and improvement rates. Furthermore, overall effectiveness and good tolerability of the cream were reported in most subjects with no differences according to the type of skin impairment, age category, frequency of product application, or regimen type. The study product was effective when used alone, and its global effectiveness and tolerability were not impacted by the concomitant use of other medical treatments or dermocosmetics. The vast majority of subjects were satisfied with the product and found that the cream was agreeable to apply and allowed a good and rapid recovery. The good cosmetic acceptability of the cream is important for encouraging regular use, thus facilitating better and faster skin healing.
Various types of emollients or topical moisturizers are available for accelerating skin healing. Medical device repairing emollient creams have significant beneficial effects on wound healing, as shown in clinical or real-world studies [13,14,15]. They may help the physiologic healing process at different stages: during the first inflammatory stage by decreasing proinflammatory factors and by preventing secondary infections; during tissue repair by stimulating skin cell proliferation and differentiation, neocollagenesis, and re-epithelialization of the wound; and in the last maturation stage of scar tissue formation by promoting extracellular matrix remodeling and restoring skin hydration. Other skin repairing topical products, containing postbiotics or bacterial lysates with various properties (e.g., anti-inflammatory, antimicrobial, immunomodulatory, or skin regenerative activities), have recently emerged to provide non-medicated dermocosmetic solutions for hel** skin healing [16,17,18,19]. Postbiotics are attractive, naturally derived ingredients, which can be easily formulated as topical products and combined with other actives. Contrary to probiotics, which are live microorganisms, postbiotics present no risks of bacteremia or fungemia and can be used in immunocompromised subjects. Although only a few studies have been conducted so far to evaluate this new class of bioactives in wound healing [20,21,22,23], the increasing number of patents concerning postbiotics being filed by companies, and the rise in the number of commercialized postbiotic-based dermocosmetic products with claims of effectiveness for skin repair or epidermal renewal, as well as other activities, provide a strong indication of the therapeutic potential of these compounds [16, 18].
The bacterium Aquaphilus dolomiae is specifically present in Avène thermal spring water [11]. This low-mineral spring water has demonstrated in vitro antiradical and anti-inflammatory properties and has been shown to improve skin repair and skin barrier function [24,25,26]. This novel bacterial strain therefore represents a source of innovative bioactives that have multiple potential applications for skin care. Several extracts have been produced from cultures of these bacteria and have been shown to have properties relevant to the fields of dermatology and dermocosmetics. A first extract, named ADE-G1, has demonstrated in vitro and in vivo immunomodulatory and anti-inflammatory activities [27, 28], and products containing this postbiotic have been shown to be effective for reducing the severity of xerosis due to atopic dermatosis [29, 30] or anti-cancer therapies [31]. Another extract from Aquaphilus dolomiae, the postbiotic ADE-G3, has been demonstrated to modulate neuro-inflammation in in vitro models [32] and has been shown to help relieve cutaneous symptoms in subjects with sensitive facial skin when used in topical formulations [33]. The flagellin-enriched ADE-G2 postbiotic has also shown interesting properties for skin care applications, with in vitro studies demonstrating its stimulatory effects on skin cells and investigations in ex vivo models of injured skin showing its repairing activities [12]. This bioactive with the ability to accelerate wound re-epithelialization and enhance skin barrier function has been incorporated into formulations of Cicalfate® soothing products to enhance their healing properties. These skin care products containing copper/zinc salts have proven effectiveness and are indicated for use in patients with various conditions, including radiation dermatitis [34] and hand eczema [25]. The enhanced Cicalfate+ cream containing the ADE-G2 postbiotic widens the potential dermatologic applications of this panel of soothing and repairing products. In the present study, the real-life use of the ADE-G2-based cream provided immediate relief from skin discomfort and led to improvements in a range of dermatologic objective signs (erythema, edema, oozing, and scabs) and subjective symptoms (burning sensations, tingling, tightness, pruritus, and pain), all of which may delay the healing process and impact wellbeing. The combined effects of the cream are particularly important for limiting the risk of wound superinfection and for preventing healing complications. Importantly, improvements were also observed without the use of concomitant prescription therapies or other dermocosmetics, thus supporting the effectiveness of the postbiotic-based cream as a standalone skin care regimen. The cream was also effective regardless of the age of the user and was overall well tolerated.
The results of our pre-post analysis provided clear and valuable insights into the significant benefits of the soothing cream for the management of minor skin impairment or wound healing in dermocosmetic indications. Although the study design had some inherent limitations and did not allow a comparison of these effects with a control vehicle or another soothing product, the real-world approach provided highly generalizable results. In addition, the presence of reporting bias cannot be excluded, in particular because some subjects were excluded because of medical indications, and the study product use was self-assessed. Despite these limitations, the multicenter nature of the study allowed the effectiveness and tolerability of the ADE-G2-based cream to be investigated in general practice in a very large number of subjects, across a wide range of ages, and on various types of superficial skin impairment. The analysis was also based on the pre-post evaluation of objective and subjective criteria that provided concordant findings.
Conclusion
This real-world international study demonstrated that the soothing cream containing the ADE-G2 postbiotic with healing properties can assist in the treatment of superficial skin impairment or wound healing, decreasing the risk of infection and accelerating the healing process. The product was well tolerated and appreciated by most subjects. The data also support the recommended twice-daily application of the product. Posbiotics are emerging bioactives with multiple potential beneficial effects on the skin and a wide range of possible uses in the dermatology and dermocosmetic fields. Although their mechanisms of action are not fully understood and may be highly diverse, postbiotics could be used more widely to improve various skin conditions with limited side effects.
Data Availability
All data generated or analyzed during this study are included within this article or as supplementary information files.
Change history
03 June 2024
A Correction to this paper has been published: https://doi.org/10.1007/s13555-024-01167-3
References
Dreifke MB, Jayasuriya AA, Jayasuriya AC. Current wound healing procedures and potential care. Mater Sci Eng C Mater Biol Appl. 2015;48:651–62. https://doi.org/10.1016/j.msec.2014.12.068.
Korting HC, Schollmann C, White RJ. Management of minor acute cutaneous wounds: importance of wound healing in a moist environment. J Eur Acad Dermatol Venereol. 2011;25:130–7. https://doi.org/10.1111/j.1468-3083.2010.03775.x.
Bradley M, Cullum N, Nelson EA, et al. Systematic reviews of wound care management: (2). Dressings and topical agents used in the healing of chronic wounds. Health Technol Assess. 1999;3:1–35.
Kolimi P, Narala S, Nyavanandi D, Youssef AAA, Dudhipala N. Innovative treatment strategies to accelerate wound healing: trajectory and recent advancements. Cells. 2022. https://doi.org/10.3390/cells11152439.
Parker A, Lawson MAE, Vaux L, Pin C. Host-microbe interaction in the gastrointestinal tract. Environ Microbiol. 2018;20:2337–53. https://doi.org/10.1111/1462-2920.13926.
Stedman A, Nigro G, Sansonetti PJ. Microbiota-intestinal stem cells dialog: a key element for intestinal regeneration. Med Sci (Paris). 2016;32:983–90. https://doi.org/10.1051/medsci/20163211014.
Gao N, Kumar A, Jyot J, Yu FS. Flagellin-induced corneal antimicrobial peptide production and wound repair involve a novel NF-kappaB-independent and EGFR-dependent pathway. PLoS ONE. 2010;5: e9351. https://doi.org/10.1371/journal.pone.0009351.
Kondo Y, Higa-Nakamine S, Maeda N, et al. Stimulation of cell migration by Flagellin through the p38 MAP kinase pathway in cultured intestinal epithelial cells. J Cell Biochem. 2016;117:247–58. https://doi.org/10.1002/jcb.25272.
Shaykhiev R, Behr J, Bals R. Microbial patterns signaling via toll-like receptors 2 and 5 contribute to epithelial repair, growth and survival. PLoS ONE. 2008;3: e1393. https://doi.org/10.1371/journal.pone.0001393.
Mangoni ML, McDermott AM, Zasloff M. Antimicrobial peptides and wound healing: biological and therapeutic considerations. Exp Dermatol. 2016;25:167–73. https://doi.org/10.1111/exd.12929.
Bourrain M, Villette C, Nguyen T, Lebaron P. Aquaphilus dolomiae gen. nov., sp. nov., isolated from a deep aquifer. Vie et Milieu. 2012;62:191–5.
Noizet M, Bianchi P, Galliano MF, et al. Broad spectrum repairing properties of an extract of Aquaphilus dolomiae on in vitro and ex vivo models of injured skin. J Eur Acad Dermatol Venereol. 2020;34(Suppl 5):37–42. https://doi.org/10.1111/jdv.16477.
Brocario A, Maurel S, Kapoor K, Lauze C, Favrel S. Assessment of wound healing efficacy and tolerability using CicatrylTM cream based on a suction blister model in healthy subjects. Eur J Dermatol. 2022;32:762–9. https://doi.org/10.1684/ejd.2022.4355.
Pinter A, Thouvenin MD, Bacquey A, Rossi AB, Nocera T. Tolerability and efficacy of a medical device repairing emollient cream in children and adults with mild to moderate atopic dermatitis. Dermatol Ther (Heidelb). 2019;9:309–19. https://doi.org/10.1007/s13555-019-0295-0.
Thouvenin MD, Bacquey A, Nocera T, Rossi AB. Tolerability and efficacy of a medical device repairing emollient cream in adults with chronic hand dermatitis. J Cosmet Dermatol. 2018;17:1158–64. https://doi.org/10.1111/jocd.12764.
da Silva VA, de Melo Pereira GV, de Oliveira AC, et al. Production, formulation, and application of postbiotics in the treatment of skin conditions. Fermentation. 2023;9:264.
De Almeida CV, Antiga E, Lulli M. Oral and topical probiotics and postbiotics in skincare and dermatological therapy: a concise review. Microorganisms. 2023;11:1420.
Duarte M, Oliveira AL, Oliveira C, et al. Current postbiotics in the cosmetic market-an update and development opportunities. Appl Microbiol Biotechnol. 2022;106:5879–91. https://doi.org/10.1007/s00253-022-12116-5.
Rawal S, Ali SA. Probiotics and postbiotics play a role in maintaining dermal health. Food Funct. 2023;14:3966–81. https://doi.org/10.1039/d3fo00152k.
Coppola S, Avagliano C, Sacchi A, et al. Potential clinical applications of the postbiotic butyrate in human skin diseases. Molecules. 2022. https://doi.org/10.3390/molecules27061849.
Golkar N, Ashoori Y, Heidari R, et al. A novel effective formulation of bioactive compounds for wound healing: preparation, in vivo characterization, and comparison of various postbiotics cold creams in a rat model. Evid Based Complement Alternat Med. 2021;2021:8577116. https://doi.org/10.1155/2021/8577116.
Campolo M, Gallo G, Roviello F, et al. Evaluation of a gel containing a propionibacterium extract in an in vivo model of wound healing. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23094708.
Nam Y, Kim J, Baek J, Kim W. Improvement of cutaneous wound healing via topical application of heat-killed Lactococcus chungangensis CAU 1447 on diabetic mice. Nutrients. 2021. https://doi.org/10.3390/nu13082666.
Merial-Kieny C, Castex-Rizzi N, Selas B, Mery S, Guerrero D. Avene thermal spring water: an active component with specific properties. J Eur Acad Dermatol Venereol. 2011;25(Suppl 1):2–5. https://doi.org/10.1111/j.1468-3083.2010.03892.x.
Ribet V, Mielewczyk E, Sirvent A, Georgescu V, Rossi AB. A novel dermo-cosmetic product containing thermal spring water, sucralfate, copper sulfate, and zinc sulfate in the management of hand eczema. Clin Cosmet Investig Dermatol. 2018;11:373–81. https://doi.org/10.2147/CCID.S157849.
Sulimovic L, Licu D, Ledo E, et al. Efficacy and safety of a topically applied Avene spring water spray in the healing of facial skin after laser resurfacing. Dermatol Surg. 2002;28:415–8.
Aries MF, Hernandez-Pigeon H, Vaissière C, et al. Anti-inflammatory and immunomodulatory effects of Aquaphilus dolomiae extract on in vitro models. Clin Cosmet Investig Dermatol. 2016;9:421–34. https://doi.org/10.2147/ccid.S113180.
Fostini AC, Georgescu V, Decoster CJ, Girolomoni G. A cream based on Aquaphilus dolomiae extracts alleviates non-histaminergic pruritus in humans. Eur J Dermatol. 2017;27:317–8. https://doi.org/10.1684/ejd.2017.2994.
Bianchi P, Theunis J, Casas C, et al. Effects of a new emollient-based treatment on skin microflora balance and barrier function in children with mild atopic dermatitis. Pediatr Dermatol. 2016;33:165–71. https://doi.org/10.1111/pde.12786.
Deleuran M, Georgescu V, Jean-Decoster C. An emollient containing Aquaphilus dolomiae extract is effective in the management of xerosis and pruritus: an international, real-world study. Dermatol Ther (Heidelb). 2020;10:1013–29. https://doi.org/10.1007/s13555-020-00415-6.
Vendrely V, Mayor-Ibarguren A, Stennevin A, Ortiz-Brugues A. An emollient PLUS balm is useful for the management of xerosis in patients treated for cancer: a real-world, prospective, observational, multicenter study. Dermatol Ther (Heidelb). 2022;12:683–99. https://doi.org/10.1007/s13555-022-00685-2.
Lestienne F, Viode C, Ceruti I, et al. Cutaneous sensitivity modulation by Aquaphilus dolomiae extract-G3 on in vitro models of neuro-inflammation. J Eur Acad Dermatol Venereol. 2020;34(Suppl 5):43–8. https://doi.org/10.1111/jdv.16641.
Villaret A, Lestienne F, Vial F, et al. Clinical evaluation of anaesthetic-like effect of two dermocosmetic formulations containing Aquaphilus dolomiae extract-G3 in subjects with sensitive facial skin. J Eur Acad Dermatol Venereol. 2022;36(Suppl 5):6–12. https://doi.org/10.1111/jdv.17902.
De Rauglaudre G, Courdi A, Delaby-Chagrin F, et al. Tolerance of the association sucralfate/Cu–Zn salts in radiation dermatitis. Ann Dermatol Venereol. 2008;135:11–5. https://doi.org/10.1016/s0151-9638(08)70092-9.
Acknowledgements
The authors thank all study participants for their involvement in the study.
Medical Writing and Editorial Assistance.
The authors acknowledge Drs Cécile Desjobert, Emma Pilling and Marielle Romet (Synergy Pharm – Santé Active Edition) who participated in writing and language editing of the manuscript. Laboratoires Dermatologiques Avene funded the medical writing and editorial assistance.
Funding
The study, statistical analyses, medical writing and language editing services, and the Rapid Service Fee were funded by Pierre Fabre Dermo-Cosmétique.
Author information
Authors and Affiliations
Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. In addition, Ariadna Ortiz-Brugués contributed to the conception and design of the study, and critically reviewed the manuscript; Aline Stennevin managed the study, participated in the interpretation of data and critically reviewed the manuscript; Edward Lain was an investigator of the trial on which the manuscript is based, and critically reviewed the manuscript, Yuling Shi and Nicolas Frasson contributed to drafting and critically revising the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Edward Lain received honoraria from Galderma, L’Oréal, Allergan, Beiersdorf, and Pierre Fabre laboratories, and received support for attending meetings and/or travel from Pierre Fabre laboratories. Ariadna Ortiz-Brugués was an employee of Pierre Fabre Dermo-Cosmétique, France, at the time of the study and is now working at the Institut Universitaire du Cancer de Toulouse – Oncopole, France, and Aline Stennevin is an employee of Pierre Fabre Dermo-Cosmétique, France. Yuling Shi and Nicolas Frasson declare no conflict of interest.
Ethical Approval
This study was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments, and complied with the good clinical practice guidelines (CPMP/ICH/135/95, https://www.ema.europa.eu) and the current legislation for clinical trials with cosmetics in the countries where the study was conducted (Regulation (EC) No. 1223/2009 of the European Commission for the European countries). This noninterventional study evaluated a cosmetic product administered as part of the usual practice of the physicians and involved no constraints or invasive examinations. Therefore, approval of the protocol by an ethics committee or an institutional review board was not required in the countries participating in the study, in accordance with their current legislation in 2020. The included subjects, or their parents or guardians for subjects under 18 years old, received a leaflet in their native language containing details about the study and their rights, including the processing of their personal data and their right to access and modify their personal data, in accordance with Regulation (EU) N°2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons. All included subjects, or their parents or guardians, provided oral or written consent to take part in the study.
Additional information
The original online version of this article was revised: Few text corrections, corrections in table and figure updated.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shi, Y., Lain, E., Frasson, N. et al. The Real-World Effectiveness and Tolerability of a Soothing Cream Containing the Postbiotic Aquaphilus dolomiae Extract-G2 for Skin Healing. Dermatol Ther (Heidelb) 14, 697–712 (2024). https://doi.org/10.1007/s13555-024-01119-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01119-x