Abstract
Objectives
Stigma towards persons with mental illness is widespread. Mindfulness may protect against stigma by cultivating accepting attitudes, non-reactivity, and prosocial emotions. This study aimed to assess whether higher trait mindfulness among nurses was linked to lower stigma towards psychiatric patients, and whether compassion mediated this relationship.
Method
In this cross-sectional study among nurses in four tertiary care hospitals in Sri Lanka, stigma towards psychiatric patients was assessed using the Attribution Questionnaire (AQ-9), which assesses nine separate domains of stigma. The 20-item Six-Facet Mindfulness Questionnaire and the 5-item Santa Clara Brief Compassion Scale were used to assess mindfulness and compassion, respectively. Correlations among these variables were explored. Mediation analyses were performed.
Results
A total of 405 nurses (90.6% female, mean age = 39.6 years) participated in the study. Those with higher trait mindfulness were more likely to believe they would help a person with mental illness, and less likely to believe a person with mental illness should be avoided or segregated from the society. Compassion was inversely correlated with avoidance and anger, and positively correlated with pity, hel**, and coercion domains. Trait mindfulness was positively correlated with compassion. Mediation models revealed that compassion partially mediated the effects of trait mindfulness on hel** and avoidance. Facet-level analyses revealed significant effects of describing, non-reactivity, and observing on several stigma domains mediated through compassion.
Conclusions
Trait mindfulness among nurses appears to have a direct buffering effect against several domains of stigma towards psychiatric patients and significant indirect effects through compassion, albeit with small effect sizes.
Preregistration
This study is not pre-registered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Stigma towards patients with mental illness is a worldwide problem with wide-ranging consequences (Kudva et al., 2020; Thornicroft et al., 2007). Stigma has been defined as a mark or sign of disgrace usually eliciting negative attitudes to its bearer (Thornicroft et al., 2007). Social cognitive models of stigma describe its links with stereotypes (negative beliefs about a group), prejudice (agreement with stereotyped beliefs or negative emotional reactions, or both), and discrimination (behavioral consequences of prejudice, such as social exclusion). According to attribution theory, people respond to another’s health condition in a negative manner if they believe the individual has a high degree of responsibility and control over the condition (Weiner et al., 1988). Corrigan and colleagues (Corrigan, 2000; Corrigan et al., 2003) further studied the role of these causal attributions, particularly the fundamental attribution error or correspondence bias, in the genesis of stigma towards psychiatric patients, and how it leads to avoidance, segregation, coercion, and withholding help. Sociological theories, based on the premise that all interpersonal interactions are socially constructed, have highlighted the role of stigma as a wider societal force affecting the individual and the society, leading to labeling, stereoty**, separation, status loss, and discrimination (Link & Phelan, 2001; Yang et al., 2010).
Among healthcare workers such as nurses, there may be many who harbor stigmatizing attitudes towards psychiatric patients, subjecting these patients to manifold difficulties in accessing and utilizing healthcare services. Stigma towards mental illness may be more pervasive and disabling in low-and-middle-income countries, where the greatest burden of mental illness in the world is seen (Kudva et al., 2020; Mascayano et al., 2015). Interventions developed to combat stigma have not always shown consistent benefits, and their effectiveness may vary across different social or professional groups and cultures (Thornicroft et al., 2016). Modifiable psychological factors contributing to stigma could, therefore, be important ingredients in designing novel interventions with better efficacy to reduce stigma.
We propose that mindfulness may be protective against stigmatizing attitudes for several reasons. Many definitions of mindfulness highlight the importance of self-regulation of attention and awareness, and the accepting and non-judgmental attitude towards the present-moment experiences, as key elements of mindfulness (Bishop et al., 2004; Quaglia et al., 2015). Mindfulness, both as a state and a trait, embodies these fundamental attributes. Trait mindfulness has been defined as “the general tendency of a person to show characteristics of non-judgmental awareness of present-moment experience in their everyday life” (Krägeloh, 2020, pp. 64–65). While it is understood that trait mindfulness is enhanced through long-term practice of mindfulness, trait mindfulness is present, to varying degrees, among non-practitioners as well (Baer et al., 2008; Karl & Fischer, 2022). The benefits of higher trait mindfulness on psychological health are well-known (Carpenter et al., 2019; Mesmer-Magnus et al., 2017). Since stigma involves judgments and prejudices, the non-judgmental attitude that is embedded in mindfulness would not be conducive to stigma. A mindful person notices thoughts and feelings as they arise, and allows them to pass without clinging on to them; similarly, when negative evaluations or affective reactions about a person arise in the mind, one can observe them non-judgmentally and let them go. It has been posited that one can consciously override the influence of stereotypes, and to do so, one should have sufficient attentional resources to engage in controlled and deliberate thinking (Nolen-Hoeksema, et al., 2009); as mindfulness enhances attentional resources, it thus has the potential to prevent a person acting on stereotypes.
Limited research has explored the relationship between mindfulness and stigma. Most studies lending support to this relationship have investigated the effects of mindfulness on inter-group bias, the bulk of which explored racial bias. Oyler et al. (2021) reviewed 36 studies on mindfulness and inter-group bias, and found an overall small average effect size (g = 0.29) for this association. Both mindfulness-based interventions (MBIs) and brief inductions of mindfulness showed benefits in this review. Additionally, expert meditators were observed to have less inter-group bias than non-meditators; and higher trait mindfulness was shown to be associated with lower explicit indices of inter-group bias. While most studies in this review dealt with inter-group bias towards racial or religious groups, a few studies on bias towards other social groups such as homeless persons, homosexual persons, and feminists were also identified. Outside the findings of this review, further evidence comes from Hopthrow et al. (2017), who observed that a brief mindfulness exercise led to a reduction in the correspondence bias.
Another potential mechanism by which mindfulness may buffer against stigmatizing attitudes is by improving compassion. There is some degree of controversy over the definition of compassion (Gilbert, 2017; Strauss et al., 2016). Goetz et al. (2010), taking an approach similar to Lazarus (1991), have defined compassion as “the feeling that arises in witnessing another’s suffering and that motivates a subsequent desire to help” (p. 351). Although psychological research on compassion has often focused on compassion for others (Goetz et al., 2010), some conceptualizations of compassion view self-compassion as part of the same construct (Strauss et al., 2016). However, there is some empirical evidence suggesting compassion towards others and self-compassion may be independent constructs, as they are poorly correlated with each other (Mills et al., 2018; Neff & Pommier, 2013). While seeking a definition for compassion in healthcare, Perez-Bret et al. (2016) noted that compassion should be considered “a duty in healthcare professionals' daily work” (p. 604). This highlights the need to better understand compassion in the context of healthcare delivery.
Compassion is closely linked with mindfulness (Germer & Barnhofer, 2017). Exemplifying this link, Pommier (2010) posited that compassion towards others has the same three elements described by Neff (2003a, 2003b) for self-compassion, namely, kindness, mindfulness, and common humanity. Compassion-based practices are often incorporated into MBIs, while some studies suggest that MBIs which do not include explicit instruction in compassion also lead to improvements in compassion (Gu et al., 2015; Raab, 2014). According to Gilbert (2010), compassion consists of six attributes: sensitivity, sympathy, empathy, motivation/caring, distress tolerance, and non-judgment. Non-judgment, therefore, appears to be a key element common to both mindfulness and compassion. Further, mindfulness would theoretically promote sensitivity by increasing attentional resources and improve distress tolerance by its effect on emotional regulation, and thereby would increase compassion.
Despite the theoretical support for a potentially protective role of mindfulness against stigma towards patients with mental illness, the lack of research conducted in this regard is noteworthy. Some studies have demonstrated beneficial effects of mindfulness for self-stigma among patients with mental illness (Martin et al., 2020; Tang et al., 2021), but the effects on public stigma and stigma among healthcare professionals remain unexplored. In this setting, we set out to investigate whether trait mindfulness and facets of mindfulness were associated with lower stigma among nurses towards psychiatric patients, and to investigate whether compassion towards others acts as a mediator in these relationships.
Method
Participants
This was a cross-sectional study conducted among 405 nurses recruited from four tertiary care hospitals in Sri Lanka between August and September 2021. Nursing officers of any grade were included as potential participants. Only those who were literate in the Sinhalese language were included, as the questionnaires were provided in Sinhalese. The sociodemographic characteristics of the participants are summarized in Table 1. The large majority of the sample (90.6%) was female. The age of participants ranged from 18 to 59 years, with a mean age of 39.6 years (SD = 9.2). The total service duration in nursing ranged from 1 month to 36 years, with a mean of 14.3 years (SD = 9.6). According to the grading of nurses in Sri Lanka, the majority were from Grade II (32.9%) and Grade III (27.2%). The commonest specialties in which the participating nurses were currently working were surgery (24.8%) and internal medicine (22.6%), while 14% were from psychiatry. Almost a quarter of participants (24%) reported that they had worked in a psychiatry unit at some point during their career. Fifty-five (13.8%) nurses reported that they had a close relative with a mental illness, and 26 (6.6%) nurses reported that they had a close friend with a mental illness. The religion of the majority of participants (n = 391, 97%) was Buddhism. Eighty-nine participants (22.4%) reported that they regularly practice at least one form of mediation.
Procedure
A non-random convenience sampling method was used, where the researchers visited different wards (including the psychiatry unit) at four hospitals, namely, Colombo North Teaching Hospital, National Hospital Kandy, Teaching Hospital Karapitiya, and Teaching Hospital Anuradhapura, and invited nurses to participate in the study. A briefing was given and an information sheet provided to each participant before requesting them to sign the consent form if they wished to participate in the study out of their own free will. The researchers made sure that the routine clinical duties of the nurses participating in the study were not affected by participating in the study.
Measures
Attributions Questionnaire (AQ-9)
Stigma towards psychiatric patients was assessed using the short version of the Attribution questionnaire (AQ)-27 developed by Corrigan et al. (2003). This 9-item brief self-report version has been derived by selecting the item with the highest factor loading from each of the nine domains in the 27-item version. It measures stigmatizing attitudes by assessing emotional reactions and discriminatory responses based on a hypothetical vignette about a man named Harry who has schizophrenia. Each item measures a unique domain of stigma, and the responses are rated on a Likert scale ranging from 1 (not at all) to 9 (very much). For example, the Help domain was assessed using the item “How likely is it that you would help Harry?”; the Avoidance domain by “I would try to stay away from Harry”; and Dangerousness domain by “How dangerous would you feel Harry is?” Other domains assessed by the AQ-9 are pity (feeling pity for Harry), fear (feeling scared of Harry), blame (believing it is Harry’s own fault that he is in his present condition), segregation (believing that Harry should be kept segregated from the society), anger (feeling angry at Harry), and coercion (believing Harry should be forced into treatment even if he refuses to). AQ-9 has been used in numerous stigma research previously (Corrigan et al., 2014). For the present study, the English language version of the AQ-9 was culturally adapted into the Sinhalese language using forward and backward translation by bilingual experts, and subsequent revisions by an expert panel. It was not possible to test its factor structure using CFA or assess the internal consistency of subscales since each domain in the AQ-9 was measured by only a single item. Corrigan et al. (2003) have not endorsed summing the scores of all items in their attribution questionnaires nor have they evaluated the internal consistency of the total scale.
Six-Facet Mindfulness Questionnaire (SFMQ)—Sinhalese Version
To measure trait mindfulness, the six-facet short form of the Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006) developed in the Sinhalese language was used (Baminiwatta et al., 2022). A detailed psychometric evaluation of the SFMQ—Sinhala version was reported previously (Baminiwatta et al., 2022). SFMQ consists of 20 items selected from the 39 items in the FFMQ using factor analytic findings. The 5-factor model proposed by Baer et al. (2006), where mindfulness was parsed into five facets, viz. Observing (sample item: “I pay attention to sounds, such as clocks ticking, birds chir**, or cars passing”), Acting with Awareness (sample item: “When I do things, my mind wanders off and I’m easily distracted”), Non-judging (sample item: “I tell myself that I shouldn’t be thinking the way I’m thinking”), Describing (sample item: “I’m good at finding words to describe my feelings”), and Non-reactivity (sample item: “In difficult situations, I can pause without immediately reacting”), could not be replicated in the Sri Lankan Buddhist population. Instead, a 6-factor solution where the Acting with awareness facet split into two — Distract (sample item: “I am easily distracted”) and Autopilot (sample item: “It seems I am ‘running on automatic’ without much awareness of what I’m doing”) — received better statistical support. Cultural variations in the factor structure of mindfulness have been observed earlier and a few studies have provided support for the 6-factor structure of mindfulness (Karl et al., 2020; Lecuona et al., 2021). The 20-item scale showed acceptable internal consistency in the validation study (Cronbach’s alpha = 0.70), and the subscales, consisting of 3 to 4 items, also showed satisfactory internal consistencies (Cronbach’s α = 0.67 to 0.72). The internal consistency and scale reliability of the SFMQ in the present study were comparable (Cronbach α = 0.71; McDonald ω = 0.75).
Santa Clara Brief Compassion Scale (SCBCS)
SCBCS is a 5-item brief scale that assesses compassion towards others, particularly towards strangers rather than close ones (Hwang et al., 2008). Responses are recorded on a 7-point Likert scale ranging from 1 (not at all true of me) to 7 (very true of me), for items such as “When I hear about someone (stranger) going through a difficult time, I feel a great deal of compassion for him or her.” It has shown a strong correlation (r = 0.95) with its parent scale, the 21-item Compassionate Love Scale (Sprecher & Fehr, 2005). This brief scale was selected for this study considering its brevity. The English language version of the SCBCS was culturally adapted into the Sinhalese language using forward and backward translation by bilingual experts, followed by expert panel discussion and consensus. The 1-factor model of the Sinhalese SCBCS was supported by confirmatory factor analysis (CFA) in the present dataset with satisfactory model fit indices (Comparative Fit Index (CFI) = 0.984; Tucker-Lewis Index (TLI) = 0.968; Standardized Root Mean Square Residual (SRMR) = 0.07). The internal consistency and scale reliability of the Sinhalese SCBCS were good (Cronbach α = 0.81; McDonald ω = 0.85).
Data Analyses
Statistical software packages — IBM SPSS Version 21 and RStudio — were used for the data analysis. Pearson’s correlations between the study variables (stigma domain scores, trait mindfulness and facet scores, and compassion score) were assessed. Mediation analysis was performed to investigate whether compassion mediated the relationship between trait mindfulness and each stigma domain, as well as between mindfulness facets and each stigma domain. Mediation analysis was conducted only if (1) the relevant independent variable (i.e., trait mindfulness or facet score) and the dependent variable (i.e., stigma domain score) were significantly correlated with each other, and (2) the independent variable and the mediator (i.e., compassion score) were significantly correlated, with p < 0.05. Mediation models were tested using the structural equation modeling (SEM) function on the lavaan package in RStudio. Maximum likelihood (ML) estimation with robust (Huber-White) standard errors and a scaled test statistic (Yuan-Bentler) was used, as robust ML estimation corrects for non-normality-induced bias in standard errors (Finney & DiStefano, 2006). Except for one item in the AQ-9, the skewness and kurtosis values of the variables fell within acceptable limits recommended for SEM (skewness between − 3 and + 3, kurtosis between − 10 and + 10; Brown, 2006). The significance of direct effects (c) and indirect effects (ab) was tested. Bootstrap** (set to 10,000 draws) was used in calculating the significance of the indirect effects. The proportion of missing data for each variable of interest was less than 6.5%, and missing data were handled using ML estimation.
Results
The mean mindfulness score among nurses, when averaged per item (out of a maximum score of 5), was 3.47 (SD = 0.44). The mean compassion score (out of a maximum score of 7) was 5.50 (SD = 1.05). The mean scores on the nine domains of stigma as per the AQ-9 and mindfulness facet scores are given in Table 2. Out of the 7 domains where higher scores indicate greater stigma (i.e., except help and pity), the highest score was seen for coercion, followed by dangerousness and fear.
The correlations between mindfulness and stigma domains are given in Table 3. Out of the nine domains of stigma assessed using the AQ-9, three domains showed significant correlations with trait mindfulness. These domains were avoidance (r = − 0.22, p < 0.001), help (r = 0.15, p = 0.003), and segregation (r = − 0.11, p = 0.033). In other words, those with higher trait mindfulness were more likely to believe they would help the person with a mental illness given in the vignette, and less likely to believe the person should be avoided or segregated from the society.
When the inter-correlations between the six mindfulness facets and the stigma domains were explored, further significant correlations emerged; eight out of the nine stigma domains showed significant correlations with at least one mindfulness facet. Nurses with higher scores on the Observing and Non-reactivity facets endorsed more pity towards patients with mental illness. Those scoring higher on the Distract facet (indicating lower distractibility) showed less fear towards the patient. Nurses who scored higher on the Describing facet were less likely to find the patient blameworthy for his problems. The segregation domain of stigma showed a significant inverse correlation only with the Non-reactivity facet. Nurses with higher scores on the Describing facet were less likely to feel angry towards the patient with mental illness. A more favorable attitude towards hel** the patient correlated positively with the Describing and Non-reactivity facets. The avoidance domain showed significant inverse correlations with all facets of mindfulness except the Observing facet. Coercion (believing that the patient should be forced into treatment with the doctor even if the patient is not willing) showed a positive correlation with the Describing facet and a negative correlation with the Non-judging facet.
Trait mindfulness was positively correlated with compassion (r = 0.23, p < 0.001). Out of the six facets of mindfulness, only Observing (r = 0.20, p < 0.001), Describing (r = 0.28, p < 0.001), and Non-reactivity (r = 0.18, p = 0.001) facets showed significant positive correlations with compassion. Among the nine domains of stigma, three domains showed positive correlations with compassion, namely, pity (r = 0.30, p < 0.001), help (r = 0.25, p < 0.001), and coercion (r = 0.22, p < 0.001). Two domains, namely, anger (r = − 0.12, p < 0.001) and avoidance (r = − 0.21, p < 0.001), were inversely correlated with compassion.
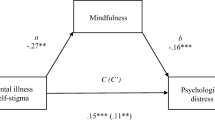
The conceptual model hypothesizing that compassion mediated the relationship between trait mindfulness and stigmatizing attitudes was applied to each of the three stigma domains (help, segregation, and avoidance) which were found to be significantly correlated with trait mindfulness in univariate analyses (see above). The mediation model for the help domain indicated a significant direct effect (c = 0.55, p = 0.009) of trait mindfulness on hel** as well as a significant indirect effect (ab = 0.23, p = 0.005) through compassion (Fig. 1a). Thus, compassion partially mediated the effect of trait mindfulness on hel** psychiatric patients. For the avoidance domain, a significant direct effect (c = 0.78, p < 0.001) of trait mindfulness as well as a significant indirect effect (ab = -0.16, p = 0.015) through compassion was observed, indicating that compassion partially mediated the effect of trait mindfulness on avoidance (Fig. 1b). The mediation model for the segregation domain did not reveal a significant indirect effect via compassion (ab = 0.04, p = 0.53), indicating that compassion did not mediate the effect of trait mindfulness on segregation (Fig. 1c).
Next, the mediating role of compassion in relation to the effects of individual mindfulness facets on stigma domains was explored. Ten mediation models were tested in this regard. As noted earlier, the Describing facet showed significant univariate correlations with five stigma domains. Compassion was found to completely mediate the effects of Describing on avoidance (ab = − 0.15, p = 0.004; c = − 0.14, p = 0.323) and coercion (ab = 0.18, p = 0.003; c = 0.15, p = 0.351) as the direct effects became non-significant, and partially mediate the effects on the help domain (ab = 0.17, p = 0.003; c = 0.48, p = 0.001), but compassion did not mediate the effect of Describing on anger and blame. As noted above, the Non-reactivity facet showed significant univariate correlations with four stigma domains; compassion was shown to completely mediate the effects of Non-reactivity on help (ab = 0.12, p = 0.012; c = 0.18, p = 0.232), avoidance (ab = − 0.09, p = 0.024; c = − 0.26, p = 0.064), and pity (ab = 0.18, p = 0.006; c = 0.16, p = 0.314) domains, but did not mediate the effect on segregation. Moreover, compassion was found to completely mediate the effect of the Observe facet on the pity domain (ab = 0.14, p = 0.004; c = 0.09, p = 0.483).
Discussion
In this study, we cross-sectionally assessed the relationship between trait mindfulness and stigma towards patients with mental illness among nurses in Sri Lanka. We found that higher trait mindfulness was associated with a greater self-report likelihood of hel** psychiatric patients, and a lower likelihood of avoiding or segregating psychiatric patients. Trait mindfulness was positively correlated with compassion. Compassion showed significant correlations with five out of the nine stigma domains. In a series of mediation analyses, we found evidence that compassion partially mediated the association between trait mindfulness and two stigma domains, namely, the help and avoidance domains. This suggests that nurses with higher trait mindfulness are more likely to help and less likely to avoid patients with mental illness at least partly because trait mindfulness enhances compassion.
As the relationship between trait mindfulness and stigma was only partially mediated by compassion, there ought to be other mediators contributing to this. The potential of mindfulness to improve self-awareness and regulation of cognitive and emotional reactions and to inculcate a non-judgmental and accepting attitude may have been other potential mechanisms (Bishop et al., 2004; Hayes & Feldman, 2004). Moreover, there is empirical evidence that mindfulness reduces the fundamental attribution error (Hopthrow et al., 2017). The role of the fundamental attribution error in the formation of stigma towards patients with mental illness is well-known (Corrigan et al., 2003), and therefore, changes in causal attribution may have been another mediator between mindfulness and stigma. Suggesting further possible mediators, mindfulness and loving-kindness meditation have been shown to reduce implicit inter-group bias by mitigating automatic stereotype activations (Lueke & Gibson, 2014; Stell & Farsides, 2016), reducing psychological stress (Kang et al., 2014), and increasing acceptance and flexibility (Lillis & Hayes, 2007).
Although overall trait mindfulness was associated with only three stigma domains, correlations for individual facets of mindfulness showed that different facets of mindfulness contributed to stigma in varied ways. Out of the nine stigma domains, all except the dangerousness domain showed significant correlations with at least one facet of mindfulness. Among the mindfulness facets, Describing (labeling experiences with words) and Non-reactivity (allowing thoughts/feelings to come and go without reacting to them or getting caught up in them) showed significant correlations with the highest number of stigma domains; Describing was correlated with five, and Non-reactivity with four domains. The least number of correlations was observed for the Observing (noticing internal/external experiences) and Autopilot (acting without conscious intention or awareness of present-moment sensory perception) facets, each contributing to only one domain. These observations indicate that mindfulness facets have differential contributions to stigmatizing attitudes, and therefore, interventions that seek to combat stigma may benefit from a greater focus towards enhancing the Describing and Non-reactivity facets. Similar to this, studies exploring the relationship between different facets of trait mindfulness and empathy have revealed heterogeneous and scattered results (Ardenghi et al., 2021).
In this study, higher trait mindfulness was associated with higher levels of compassion. This supports the theoretical association between mindfulness and compassion (Germer & Barnhofer, 2017; Neff, 2003a, 2003b; Voci et al., 2019). Although empirical data directly tap** into this relationship are limited, the close link between mindfulness practice and the development compassion is well-recognized within Buddhist literature (Kang & Whittingham, 2010; Tirch, 2010). A study by Mahon et al. (2017) has shown that mindfulness training improves compassion among nurses, but another study failed to demonstrate a significant change in SCBCS score among primary care clinicians following an abbreviated mindfulness intervention (Fortney et al., 2013). The authors of the latter study noted that the null effect on compassion may be due to high baseline compassion scores (Fortney et al., 2013). Most studies evaluating the effects of mindfulness training on compassion have investigated self-compassion rather than compassion towards others (Cheang et al., 2019). There is evidence that an increase in self-compassion may be a mediator of the benefits of mindfulness practice on psychological health (Gu et al., 2015; van der Velden et al., 2015). However, according to Neff’s model of self-compassion, which is founded on Buddhist teachings on compassion, “common humanity” is one of its three key components (Neff, 2003a, 2003b). Common humanity refers to framing one’s suffering as part of being human and as an experience that connects the self to others rather than isolating oneself from them. It has been posited that mindfulness promotes a balanced perspective taking and counters egocentrism, thereby inducing a sense of interconnectedness (Neff, 2003a, 2003b). Therefore, mindfulness training is likely to endorse compassion towards both self and others. Conversely, in a study by Neff and Pommier (2013), there was no correlation between self-compassion and compassion towards others among college undergraduates, suggesting the possibility that these are two independent constructs. As further support for this dichotomy, Mills et al. (2018) found, among nurses and doctors, that compassion for others (measured using SCBCS) and self-compassion were negatively correlated with each other. In our study also, compassion was measured using SCBCS, which conceptualizes compassion as being other-oriented. Thus, further research using different measures of compassion could tap into any differential effects of self- and other-oriented compassion on stigma. In a recent study, interconnectedness and compassion were shown to reduce stigma towards people with mental illness, but the role of mindfulness was not studied (Yu et al., 2021). Further support for the relationship between mindfulness and compassion could be derived from studies which show that mindfulness leads to prosocial behaviors (Donald et al., 2019).
At the facet level, three facets of mindfulness, namely, Observing, Describing, and Non-reactivity, were associated with compassion in the present study. Despite non-judgment being theorized to be an important attribute of compassion (Gilbert, 2010), compassion did not correlate significantly with the Non-judging facet in the present population. Published data on correlations between mindfulness facets and other-oriented compassion are scarce, but in a previous study by Medvedev et al. (2021), where a network analysis of mindfulness facets, affect, compassion, and distress was conducted, compassion was found to be negatively correlated with Non-judging. They also found a weak positive correlation between compassion and the Observing facet, similar to present findings.
Compassion was correlated with several domains of stigma in the expected direction. Higher compassion was related to higher pity and hel**. In Corrigan’s (2000) work on social attribution in mental health stigma, when one encounters a person with mental illness, an affective response of pity is generated if the symptoms are perceived as uncontrollable and the person is viewed as not responsible for their illness, and the behavioral consequence of this is hel** behavior. The link observed between compassion and hel** was anticipated because, in addition to being moved by another’s suffering, “wanting to help” is integral to compassion (Goetz et al., 2010; Lazarus, 1991). The inverse correlation between compassion and anger is also understandable; in Corrigan’s path model, anger is the affective response to a person with mental illness when the person is viewed as responsible for their illness and the symptoms are perceived as uncontrollable. Compassion-based interventions have been shown to reduce interpersonal problems including anger (Hofmann et al., 2011). Further, compassion was seen to be negatively correlated with avoidance, since a compassionate person would be unlikely to consciously avoid a person with mental illness. Interestingly, Corrigan et al. (2003) has previously noted that avoidance and withholding help are highly correlated with each other.
An unexpected positive correlation was observed between compassion and coercion. Although this may seem counterintuitive, a closer look at the question used to assess coercion in the AQ-9 provides an explanation. Participants were required to answer the question, “How much do you agree that Harry should be forced into treatment with his doctor even if he does not want to?” with regard to a man with schizophrenia who has been “hospitalized six times because of his illness,” and “sometimes hears voices and becomes upset.” The moral framing of coercive treatment in mental healthcare has been a contentious issue. It is likely that nurses with higher compassion believed that the patient would benefit from being treated involuntarily, as the patient may have lost insight due to the psychotic illness. Previous surveys among healthcare professionals have revealed a notable tendency to endorse coercive treatment for psychiatric patients, as they believed it was morally justified, constituting what has been called “good coercion” or “beneficial coercion” (Lawn et al., 2015; Lorem et al., 2015; Steiger et al., 2022). From an ethical point of view, coercive treatment may be justified in a context of “beneficence,” where the long-term benefits of treatment outweigh any temporary distress or perceived harm. Also, it has been argued that treatment restores the patient’s “autonomy,” which has been lost due to the illness (Prinsen & van Delden, 2009). Cultural differences in the moral framing of coercive treatment may also exist (Ewuoso, 2016; Shah & Basu, 2010). In Asian cultures like Sri Lanka, traditionally, a paternalistic approach has prevailed within the practice of medicine, which may have sanctioned coercive treatment (Shah & Basu, 2010). Thus, our findings call into question the validity of the coercion domain in the assessment of stigma, or at least the item used in the AQ-9 to this end.
Facet-level mediation analyses in the present study revealed that among the facets of mindfulness, Describing and Non-reactivity showed the most prominent effects against stigma, many of them being mediated either fully or partially through compassion. This implies that those who are better in describing and taking a non-reacting attitude towards their present-moment experiences are often more likely to feel compassion for others, and this makes them less likely to harbor stigmatizing attitudes towards psychiatric patients. The Observing facet also showed a positive effect on feeling pity for psychiatric patients, but this effect was also fully mediated by an increase in compassion. Thus, interventions designed to combat stigma towards psychiatric patients may benefit from a focus on enhancing mindful skills in describing, non-reacting, and observing.
Although our findings provide evidence of statistically significant effects of trait mindfulness on compassion and stigmatizing attitudes, it should be noted that these effects were small in magnitude. However, these observations are mostly consistent with our theoretical understanding of the constructs measured. These findings may have important implications at the population level, where the practice of mindfulness and compassion among healthcare workers may contribute to a reduction in the negative effects of stigma experienced by health service users.
Limitations and Future Research
The cross-sectional design of the study precluded establishing any causal relationships between the studied constructs. The sample was predominated by females, limiting the applicability of the findings to the male nursing population. The large majority of the participants (97%) were Buddhists; therefore, caution should be exercised when generalizing these findings to other cultural contexts. This study was conducted during the COVID-19 pandemic; it is possible that this context could have affected the levels of mindfulness, compassion, and stigma among nurses, thereby interfering with the results. Being compassionate is generally considered a professional duty for healthcare professionals (Perez-Bret et al., 2016); hence, social desirability bias may have exaggerated the nurses’ self-report compassion levels. Another limitation is the potential effect of common methods bias; multiple constructs being measured using common methods may have led to spurious effects due to the measurement methods rather than to the constructs being measured, possibly owing to response styles, social desirability, and priming effects (Podsakoff et al., 2012).
Our findings add useful new knowledge regarding an understudied area in stigma of mental illness. The finding that trait mindfulness, a potentially modifiable factor, was associated with lower stigma in three domains can inform the design of novel interventions for stigma reduction among healthcare workers. Mindfulness training can be either incorporated into an existing stigma reduction program supported by evidence, or used as a stand-alone intervention. Since there is no direct evidence for the latter as of now, the former approach may be preferred at this time. As compassion was seen to mediate some relationships between trait mindfulness and stigma, including overt instruction in compassion-based practices could potentially augment the efficacy of such a program. In the present study, we have focused on other-oriented compassion, setting aside self-compassion. Whether the cultivation of self-compassion in addition to other-oriented compassion has added advantages in stigma reduction needs to be investigated. At a larger scale, introducing the concepts of mindfulness and compassion to nurses at an earlier stage, preferably during training years, could be a useful step towards combating stigma in mental healthcare.
Our current findings are cross-sectional in nature, and therefore, the effect of mindfulness on stigmatizing attitudes towards psychiatric patients needs to be studied using an interventional study design before any robust recommendations can be made. To this end, a randomized controlled trial on whether a mindfulness-based intervention is effective in reducing stigma among healthcare workers, and whether this effect is mediated by compassion, would be helpful. Since compassion was only a partial mediator in the present analysis, other potential mediators should be explored in future research. Moreover, future studies could investigate whether the mediation models supported among nurses in this study can be replicated in other samples such as the general population. It is also important to study whether there are differences between meditating and non-meditating samples with regard to this conceptual model, and explore potential effects of the frequency and duration of meditation experience. Also, among the scales designed to assess public stigma, we selected a scale grounded in attribution theory; while this was supported by empirical data suggesting that mindfulness could mitigate the fundamental attribution error, exploring alternative conceptualizations of stigma could further expand our understanding of these constructs and their inter-links.
Data Availability
All data are available at the Open Science Framework (https://osf.io/syqka).
References
Ardenghi, S., Rampoldi, G., Pepe, A., Bani, M., Salvarani, V., & Strepparava, M. G. (2021). An exploratory cross-sectional study on the relationship between dispositional mindfulness and empathy in undergraduate medical students. Teaching and Learning in Medicine, 33(2), 154–163. https://doi.org/10.1080/10401334.2020.1813582
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., Walsh, E., Duggan, D., & Williams, J. M. G. (2008). Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment, 15(3), 329–342. https://doi.org/10.1177/1073191107313003
Baminiwatta, A., Alahakoon, H., Herath, N. C., Kodithuwakku, K. M., & Nanayakkara, T. (2022). Psychometric evaluation of a Sinhalese version of the Five Facet Mindfulness Questionnaire and development of a six-facet short form in a Sri Lankan Buddhist context. Mindfulness, 13(4), 1069–1082. https://doi.org/10.1007/s12671-022-01863-1
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. https://doi.org/10.1093/clipsy.bph077
Brown, T. A. (2006). Confirmatory factor analysis for applied research. Guilford Press.
Carpenter, J. K., Conroy, K., Gomez, A. F., Curren, L. C., & Hofmann, S. G. (2019). The relationship between trait mindfulness and affective symptoms: A meta-analysis of the Five Facet Mindfulness Questionnaire (FFMQ). Clinical Psychology Review, 74, 101785. https://doi.org/10.1016/j.cpr.2019.101785
Cheang, R., Gillions, A., & Sparkes, E. (2019). Do mindfulness-based interventions increase empathy and compassion in children and adolescents: A systematic review. Journal of Child and Family Studies, 28(7), 1765–1779. https://doi.org/10.1007/s10826-019-01413-9
Corrigan, P., Markowitz, F. E., Watson, A., Rowan, D., & Kubiak, M. A. (2003). An attribution model of public discrimination towards persons with mental illness. Journal of Health and Social Behavior, 44(2), 162–179. https://doi.org/10.2307/1519806
Corrigan, P. W. (2000). Mental health stigma as social attribution: implications for research methods and attitude change. Clinical Psychology: Science and Practice, 7(1), 48–67. https://doi.org/10.1093/clipsy.7.1.48
Corrigan, P. W., Powell, K. J., & Michaels, P. J. (2014). Brief battery for measurement of stigmatizing versus affirming attitudes about mental illness. Psychiatry Research, 215(2), 466–470. https://doi.org/10.1016/j.psychres.2013.12.006
Donald, J. N., Sahdra, B. K., Van Zanden, B., Duineveld, J. J., Atkins, P. W. B., Marshall, S. L., & Ciarrochi, J. (2019). Does your mindfulness benefit others? A systematic review and meta-analysis of the link between mindfulness and prosocial behaviour. British Journal of Psychology, 110(1), 101–125. https://doi.org/10.1111/bjop.12338
Ewuoso, C. (2016). Beneficial coercion in psychiatric care: Insights from African ethico-cultural system. Develo** World Bioethics, 18(2), 91–97. https://doi.org/10.1111/dewb.12137
Finney, S. J., & DiStefano, C. (2006). Non-normal and categorical data in structural equation modeling. In R. Hancock & G. Mueller (Eds.), Structural equation modeling: A second course (pp. 269–314). Information Age Publishing.
Fortney, L., Luchterhand, C., Zakletskaia, L., Zgierska, A., & Rakel, D. (2013). Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: A pilot study. Annals of Family Medicine, 11(5), 412–420. https://doi.org/10.1370/afm.1511
Germer, C., & Barnhofer, T. (2017). Mindfulness and compassion: Similarities and differences. In P. Gilbert (Ed.), Compassion: Concepts, research and applications (pp. 69–86). Routledge.
Gilbert, P. (2010). The compassionate mind. Constable and Robinson.
Gilbert, P. (2017). Compassion: concepts, research and applications. Routledge.
Goetz, J. L., Keltner, D., & Simon-Thomas, E. (2010). Compassion: An evolutionary analysis and empirical review. Psychological Bulletin, 136(3), 351–374. https://doi.org/10.1037/a0018807
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. https://doi.org/10.1016/j.cpr.2015.01.006
Hayes, A. M., & Feldman, G. (2004). Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice, 11(3), 255–262. https://doi.org/10.1093/clipsy.bph080
Hofmann, S. G., Grossman, P., & Hinton, D. E. (2011). Loving-kindness and compassion meditation: Potential for psychological interventions. Clinical Psychology Review, 31(7), 1126–1132. https://doi.org/10.1016/j.cpr.2011.07.003
Hopthrow, T., Hooper, N., Mahmood, L., Meier, B. P., & Weger, U. (2017). Mindfulness reduces the correspondence bias. Quarterly Journal of Experimental Psychology, 70(3), 351–360. https://doi.org/10.1080/17470218.2016.1149498
Hwang, J. Y., Plante, T., & Lackey, K. (2008). The development of the Santa Clara Brief Compassion Scale: An abbreviation of Sprecher and Fehr’s Compassionate Love Scale. Pastoral Psychology, 56, 421–428. https://doi.org/10.1007/s11089-008-0117-2
Kang, C., & Whittingham, K. (2010). Mindfulness: A dialogue between Buddhism and clinical psychology. Mindfulness, 1(3), 161–173. https://doi.org/10.1007/s12671-010-0018-1
Kang, Y., Gray, J. R., & Dovidio, J. F. (2014). The nondiscriminating heart: Lovingkindness meditation training decreases implicit intergroup bias. Journal of Experimental Psychology. General, 143(3), 1306–1313. https://doi.org/10.1037/a0034150
Karl, J. A., & Fischer, R. (2022). The state of dispositional mindfulness research. Mindfulness, 13(6), 1357–1372. https://doi.org/10.1007/s12671-022-01853-3
Karl, J. A., Prado, S. M. M., Gračanin, A., Verhaeghen, P., Ramos, A., Mandal, S. P., Michalak, J., Zhang, C.-Q., Schmidt, C., Tran, U. S., Druica, E., Solem, S., Astani, A., Liu, X., Luciano, J. V., Tkalčić, M., Lilja, J. L., Dundas, I., Wong, S. Y. S., & Fischer, R. (2020). The cross-cultural validity of the Five-Facet Mindfulness Questionnaire across 16 countries. Mindfulness, 11(5), 1226–1237. https://doi.org/10.1007/s12671-020-01333-6
Krägeloh, C. (2020). Mindfulness Research and Terminology Science. Mindful Practice, 1, 53–84.
Kudva, K. G., El Hayek, S., Gupta, A. K., Kurokawa, S., Bangshan, L., Armas-Villavicencio, M. V. C., Oishi, K., Mishra, S., Tiensuntisook, S., & Sartorius, N. (2020). Stigma in mental illness: Perspective from eight Asian nations. Asia-Pacific Psychiatry, 12(2), e12380. https://doi.org/10.1111/appy.12380
Lawn, S., Delany, T., Pulvirenti, M., Smith, A., & McMillan, J. (2015). A qualitative study examining the presence and consequences of moral framings in patients’ and mental health workers’ experiences of community treatment orders. BMC Psychiatry, 15, 274. https://doi.org/10.1186/s12888-015-0653-0
Lazarus, R. S. (1991). Emotion and adaptation. Oxford University Press.
Lecuona, O., García-Rubio, C., de Rivas, S., Moreno-Jiménez, J. E., Meda-Lara, R. M., & Rodríguez-Carvajal, R. (2021). A network analysis of the Five Facets Mindfulness Questionnaire (FFMQ). Mindfulness, 12(9), 2281–2294. https://doi.org/10.1007/s12671-021-01704-7
Lillis, J., & Hayes, S. C. (2007). Applying acceptance, mindfulness, and values to the reduction of prejudice: A pilot study. Behavior Modification, 31(4), 389–411. https://doi.org/10.1177/0145445506298413
Link, B. G., & Phelan, J. C. (2001). Conceptualizing stigma. Annual Review of Sociology, 27(1), 363–385. https://doi.org/10.1146/annurev.soc.27.1.363
Lorem, G. F., Hem, M. H., & Molewijk, B. (2015). Good coercion: Patients’ moral evaluation of coercion in mental health care. International Journal of Mental Health Nursing, 24(3), 231–240. https://doi.org/10.1111/inm.12106
Lueke, A., & Gibson, B. (2014). Mindfulness meditation reduces implicit age and race bias: The role of reduced automaticity of responding. Social Psychological and Personality Science, 6(3), 284–291. https://doi.org/10.1177/1948550614559651
Mahon, M. A., Mee, L., Brett, D., & Dowling, M. (2017). Nurses’ perceived stress and compassion following a mindfulness meditation and self compassion training. Journal of Research in Nursing, 22(8), 572–583. https://doi.org/10.1177/1744987117721596
Martin, T. J., Spencer, S. D., & Masuda, A. (2020). Mindfulness mediates the relationship between mental health self-stigma and psychological distress: A cross-sectional study. Current Psychology, 41, 5333–5342. https://doi.org/10.1007/s12144-020-01050-2
Mascayano, F., Armijo, J. E., & Yang, L. H. (2015). Addressing stigma relating to mental illness in low- and middle-income countries. Frontiers in Psychiatry, 6, 38. https://doi.org/10.3389/fpsyt.2015.00038
Medvedev, O. N., Cervin, M., Barcaccia, B., Siegert, R. J., Roemer, A., & Krägeloh, C. U. (2021). Network analysis of mindfulness facets, affect, compassion, and distress. Mindfulness, 12(4), 911–922. https://doi.org/10.1007/s12671-020-01555-8
Mesmer-Magnus, J., Manapragada, A., Viswesvaran, C., & Allen, J. W. (2017). Trait mindfulness at work: A meta-analysis of the personal and professional correlates of trait mindfulness. Human Performance, 30, 79–98. https://doi.org/10.1080/08959285.2017.1307842
Mills, J., Wand, T., & Fraser, J. A. (2018). Examining self-care, self-compassion and compassion for others: a cross-sectional survey of palliative care nurses and doctors. International Journal of Palliative Nursing, 24(1), 4–11. https://doi.org/10.12968/ijpn.2018.24.1.4
Neff, K. (2003a). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032
Neff, K. D. (2003b). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027
Neff, K. D., & Pommier, E. (2013). The relationship between self-compassion and other-focused concern among college undergraduates, community adults, and practicing meditators. Self and Identity, 12(2), 160–176. https://doi.org/10.1080/15298868.2011.649546
Oyler, D. L., Price-Blackshear, M. A., Pratscher, S. D., & Bettencourt, B. A. (2021). Mindfulness and intergroup bias: A systematic review. Group Processes & Intergroup Relations, 25(4), 1107–1138. https://doi.org/10.1177/1368430220978694
Perez-Bret, E., Altisent, R., & Rocafort, J. (2016). Definition of compassion in healthcare: a systematic literature review. International Journal of Palliative Nursing, 22(12), 599–606. https://doi.org/10.12968/ijpn.2016.22.12.599
Podsakoff, P. M., MacKenzie, S. B., & Podsakoff, N. P. (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569. https://doi.org/10.1146/annurev-psych-120710-100452
Pommier, E. A. (2010). The compassion scale. [Doctoral dissertation, University of Texas at Austin]. UT Electronic Theses and Dissertations. https://repositories.lib.utexas.edu/handle/2152/ETD-UT-2010-12-2213
Prinsen, E. J. D., & van Delden, J. J. M. (2009). Can we justify eliminating coercive measures in psychiatry? Journal of Medical Ethics, 35(1), 69–73. https://doi.org/10.1136/jme.2007.022780
Quaglia, J. T., Brown, K. W., Lindsay, E. K., Creswell, J. D., & Goodman, R. J. (2015). From conceptualization to operationalization of mindfulness. In K. W. Brown, J. D. Creswell, & R. M. Ryan (Eds.), Handbook of mindfulness: Theory, research, and practice (pp. 151–170). Guilford Press.
Raab, K. (2014). Mindfulness, self-compassion, and empathy among health care professionals: A review of the literature. Journal of Health Care Chaplaincy, 20(3), 95–108. https://doi.org/10.1080/08854726.2014.913876
Shah, R., & Basu, D. (2010). Coercion in psychiatric care: Global and Indian perspective. Indian Journal of Psychiatry, 52(3), 203–206. https://doi.org/10.4103/0019-5545.70971
Sprecher, S., & Fehr, B. (2005). Compassionate love for close others and humanity. Journal of Social and Personal Relationships, 22(5), 629–651. https://doi.org/10.1177/0265407505056439
Steiger, S., Moeller, J., Sowislo, J. F., Lieb, R., Lang, U. E., & Huber, C. G. (2022). Approval of coercion in psychiatry in public perception and the role of stigmatization. Frontiers in Psychiatry, 12, 819573. https://doi.org/10.3389/fpsyt.2021.819573
Stell, A. J., & Farsides, T. (2016). Brief loving-kindness meditation reduces racial bias, mediated by positive other-regarding emotions. Motivation and Emotion, 40(1), 140–147. https://doi.org/10.1007/s11031-015-9514-x
Strauss, C., Lever Taylor, B., Gu, J., Kuyken, W., Baer, R., Jones, F., & Cavanagh, K. (2016). What is compassion and how can we measure it? A review of definitions and measures. Clinical Psychology Review, 47, 15–27. https://doi.org/10.1016/j.cpr.2016.05.004
Nolen-Hoeksema, S., Fredrickson, B. L., Loftus, G. R., & Wagenaar, W. A. (2009). Atkinson & Hilgard’s introduction to psychology (15th ed.). Wadsworth.
Tang, Q., Yang, S., Liu, C., Li, L., Chen, X., Wu, F., & Huang, X. (2021). Effects of mindfulness-based cognitive therapy on stigma in female patients with schizophrenia. Frontiers in Psychiatry, 12, 694575. https://doi.org/10.3389/fpsyt.2021.694575
Thornicroft, G., Mehta, N., Clement, S., Evans-Lacko, S., Doherty, M., Rose, D., Koschorke, M., Shidhaye, R., O’Reilly, C., & Henderson, C. (2016). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet, 387(10023), 1123–1132. https://doi.org/10.1016/S0140-6736(15)00298-6
Thornicroft, G., Rose, D., Kassam, A., & Sartorius, N. (2007). Stigma: Ignorance, prejudice or discrimination? The British Journal of Psychiatry, 190, 192–193. https://doi.org/10.1192/bjp.bp.106.025791
Tirch, D. D. (2010). Mindfulness as a context for the cultivation of compassion. International Journal of Cognitive Therapy, 3, 113–123. https://doi.org/10.1521/ijct.2010.3.2.113
van der Velden, A. M., Kuyken, W., Wattar, U., Crane, C., Pallesen, K. J., Dahlgaard, J., Fjorback, L. O., & Piet, J. (2015). A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical Psychology Review, 37, 26–39. https://doi.org/10.1016/j.cpr.2015.02.001
Voci, A., Veneziani, C. A., & Fuochi, G. (2019). Relating mindfulness, heartfulness, and psychological well-being: The role of self-compassion and gratitude. Mindfulness, 10(2), 339–351. https://doi.org/10.1007/s12671-018-0978-0
Weiner, B., Perry, R., & Magnusson, J. (1988). An attribution analysis of reactions to stigmas. Journal of Personality and Social Psychology, 55, 738–748. https://doi.org/10.1037/0022-3514.55.5.738
Yang, L. H., Cho, S. H., & Kleinman, A. (2010). Stigma of mental illness. In V. Patel, A. Woodward, V. Feigin, S. Quah, & K. Heggenhougen (Eds.), Mental and neurological public health: A global perspective (pp. 219–230). Elsevier.
Yu, B. C. L., Mak, W. W. S., Leung, I. W. Y., & Chio, F. H. N. (2021). Reducing stigma through interconnectedness and compassion: A Buddhism-based approach to reduce stigma toward people with mental illness. Mindfulness, 12(7), 1779–1790. https://doi.org/10.1007/s12671-021-01640-6
Acknowledgements
We are grateful to the directors of the hospitals where the study was conducted for authorizing the data collection.
Author information
Authors and Affiliations
Contributions
AB conceptualized and designed the study, contributed to data acquisition, conducted the data analysis, and wrote the first draft of the manuscript. HA, TN, KK, and NCH contributed to study design and data acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Approval was obtained from the ethics review committee of Faculty of Medicine, University of Kelaniya. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baminiwatta, A., Alahakoon, H., Herath, N.C. et al. Trait Mindfulness, Compassion, and Stigma Towards Patients with Mental Illness: A Study Among Nurses in Sri Lanka. Mindfulness 14, 979–991 (2023). https://doi.org/10.1007/s12671-023-02108-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02108-5