Abstract
Darbepoetin alfa (DA) is used to treat anemia in lower-risk (IPSS low or int-1) myelodysplastic syndromes (MDS). However, whether mutations can predict the effectiveness of DA has not been examined. The present study aimed to determine predictive gene mutations. The primary endpoint was a correlation between the presence of highly frequent (≥ 10%) mutations and hematological improvement-erythroid according to IWG criteria 2006 by DA (240 μg/week) until week 16. The study included 79 patients (age 29–90, median 77.0 years; 52 [65.8%] male). Frequently (≥ 10%) mutated genes were SF3B1 (24 cases, 30.4%), TET2 (20, 25.3%), SRSF2 (10, 12.7%), ASXL1 (9, 11.4%), and DNMT3A (8, 10.1%). Overall response rate to DA was 70.9%. Multivariable analysis including baseline erythropoietin levels and red blood cell transfusion volumes as variables revealed that erythropoietin levels and mutations of ASXL1 gene were significantly associated with worse response (odds ratio 0.146, 95% confidence interval 0.042–0.503; p = 0.0023, odds ratio 0.175, 95% confidence interval 0.033–0.928; p = 0.0406, respectively). This study indicated that anemic patients who have higher erythropoietin levels and harbor ASXL1 gene mutations may respond poorly to DA. Alternative strategies are needed for the treatment of anemia in this population. Trial registration number and date of registration: UMIN000022185 and 09/05/2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndromes (MDS) are clonal stem cell disorders characterized by ineffective hematopoiesis, and occasionally progress to acute myelogenous leukemia (AML) [1, 2]. The pathogenesis of MDS is thought to be a multistep process involving two or more genetic alterations that cause clonal proliferation of an abnormal stem cell [3, 4]. Our understanding of the molecular pathogenesis of MDS has improved in recent years, mainly through the identification of major mutational targets [5,6,7,8,9]. The majority of patients with lower-risk MDS of International Prognostic Scoring System (IPSS) [10] low or intermediate-1 risk have symptoms of anemia due to ineffective erythropoiesis [11], and need therapeutic intervention, including red blood cell (RBC) transfusion. Although RBC transfusions can temporarily reduce anemic symptoms, frequent transfusions usually lead to iron overload, which is associated with reduced survival and lower quality of life [12].
On the other hand, the development of erythropoiesis in the fetal liver and adult bone marrow is regulated by the hormone erythropoietin (EPO) [13]. Therefore, recombinant human EPO (rHuEPO) and other erythropoiesis-stimulating agents (ESAs) are used for the treatment of MDS-related anemia [14]. In Japan, darbepoetin alfa (DA), which is a re-engineered form of EPO, has been approved for clinical practice. Around 50% of the patients respond to EPO ± granulocyte-colony stimulating factors (G-CSF), and the median duration of response is 2 years [15, 16]. DA has also been reported to show an overall response rate of about 60% when employed for the treatment of anemia in lower-risk MDS [17].
Prediction of response to ESAs in anemic MDS patients is often based on clinical biomarkers such as volume of RBC transfusion, serum EPO levels, ferritin, and IPSS/IPSS-R [18], and the use of Nordic score combined with serum EPO levels and transfusion volume has also been proposed [19]. However, the relationship between molecular pathogenesis of MDS and responsiveness to DA has not yet been well studied. Here we report the results of the West Japan Hematology Study Group (W-JHS) MDS01 trial, to determine gene mutations that predict the effectiveness of DA in treating anemia of lower-risk (low or int-1 in IPSS [10] risk category) MDS.
Materials and methods
Patient eligibility
Patients with lower-risk MDS (low or int-1 in IPSS [10] category) were registered in the W-JHS MDS01 study (UMIN000022185) between February 2016 and May 2019 at 36 institutions in Japan. Other eligibility criteria were as follows: newly diagnosed patients with definite MDS based on diagnostic criteria of FAB classification [20] and the 4th edition of World Health Organization (WHO) classification [21]; patients having anemia associated with MDS, clinically eligible for DA treatment and of age 16 years or older. Patients with present or past medical record of myocardial infarction, pulmonary infarction, cerebral infarction or similar disorders or risk of thromboembolism, uncontrollable hypertension, prior treatment with DA or other formulations of EPO, severe (requiring hospital care or judged by investigators) or uncontrollable complication, and those judged inappropriate for study participation due to complication of mental disease or psychiatric symptom and cognitive disorder were excluded. This study is registered at the University Hospital Medical Information Network Clinical Trials Registry on 09/05/2016, with ID No. 000022185.
Procedure
DA at a dose of 240 µg per body was administered once weekly for 16 weeks. Analysis was performed to confirm whether the presence of a specific gene mutation with a frequency of ≥ 10% affects the efficacy of DA. Peripheral blood sample of the subjects was collected before administration of DA, and genomic DNA was extracted. The presence of gene mutations was then analyzed with a panel of 376 genes in a previous report [6] using a next-generation sequencing method. In brief, 376 known target genes in MDS were examined for mutations in 79 patients from the cohort, using massively parallel sequencing (Illumina, Inc., San Diego, CA, USA) of SureSelect (Agilent Technologies Inc., Santa Clara, CA, USA)-captured target sequences. All sequencing data were analyzed using our in-house pipeline [22], through which highly probable oncogenic mutations were called by eliminating sequencing/map** errors using an empirical Bayesian approach [23] and known/possible SNPs based on the available databases.
Assessment of response
The primary endpoint was a correlation between highly frequent (≥ 10%) gene mutations and hematological improvement-erythroid (HI-E) according to the International Working Group (IWG) criteria 2006 [24] at week 16 after the initiation of DA treatment. Secondary endpoints were major and minor responses to DA at week 16 after the initiation of treatment in blood transfusion-dependent subjects, HI-E in blood transfusion-independent and dependent subjects, variety and frequency of gene mutations observed in all subjects, the correlation between highly frequent gene mutations and interval to achievement of the first HI-E according to the IWG criteria 2006 [24], and mortality (overall survival, OS) and progression to AML (progression-free survival, PFS) from 16 weeks to 1 year after the initiation of treatment.
The IWG criteria 2006 (HI-E) were used, defined as either hemoglobin increased by 1.5 g/dL or more compared to pre-treatment (< 11.0 g/dL) or RBC transfusion volume/8 weeks decreased by more than 4 units in RBC transfusion-dependent subjects. In Japan, one unit of red blood cell preparation is produced from 200 ml of whole blood. As for transfusion-dependent subjects, the major response was defined as no need for RBC transfusion (withdrawal from RBC transfusion dependence) for more than 56 consecutive days, and increase in the highest Hb concentration during the withdrawal period by at least 1.0 g/dL compared to the baseline Hb concentration, while the minor response was defined as ≥ 50% decrease in RBC transfusion volume over 56 consecutive days compared to baseline transfusion volume. For AML progression, progression to AML or death without progression were stated as events, and the subjects without confirmed progression to AML were censored at the date of the last known survival. For overall survival (OS), death from any cause was considered an event, and for the survival cases, the study was terminated at the date of the last known survival.
Assessment of safety
All adverse events (AEs) were recorded in subjects who received DA at least once from the first administration to day 29 of the last cycle, and classified according to the Common Terminology Criteria for Adverse Events Version 4.0 [25]. For the subjects who dropped out before completion of the study, AEs were monitored for two weeks after the last administration.
Statistical analysis
Statistical significance of EPO levels before the treatment between non-responders and responders was evaluated by the Wilcoxon rank-sum test. Correlation between numbers of gene mutations and response to DA was analyzed by the Cochran-Armitage trend test and the chi-squared test.
Odds ratios between the gene mutations and the outcomes were estimated using univariate and multivariable logistic regression models. The multivariable analysis was adjusted for baseline EPO levels (low: < 100, high: ≥ 100 mIU/mL) and RBC transfusion volumes (low: < 1 unit, high: ≥ 1 unit/month) as the explanatory variables.
The survival curves were estimated using Kaplan–Meier methods, and the confidence intervals for the median survival time (MST) and the annual survival rate were calculated using Brookmeyer and Crowley's method and Greenwood's formula, respectively. In all analyses, p < 0.05 (two-sided) was considered statistically significant. Statistical analysis was performed using SAS Ver. 9.4.
Ethics
This study was conducted in compliance with the Act on the Protection of Personal Information (Act No. 57 of May 30, 2003), the Declaration of Helsinki (October 2013, translated by the Japanese Medical Association in the revised version of Fortaleza), the Clinical Research Act (Act No. 16 of 2017), the Ordinance for Enforcement of the Clinical Research Act (Ordinance No. 17 of the Ministry of Health, Labour and Welfare of 2018), and the Ethical Guidelines for Human Genome/Gene Analysis Research (February 28, 2017).
The protocol and an explanatory document regarding the protocol provided to patients were approved by the Ethics Review Committee of each participating institution. Prior to subject enrollment, the content of the study was explained to the patients using the explanatory document, and written informed consent was obtained from all participants. If a patient was under 20 years of age, written informed consent of the patient and his or her guardian was obtained.
Results
Subjects
A total of 85 patients underwent enrollment screening. Of these, 79 subjects were included in the full analysis set (FAS), after excluding 4 ineligible patients and 2 patients who withdrew their consent before the start of protocol treatment. The median (range) follow-up for FAS was 374 (44–1094) days. Baseline characteristics of the 79 subjects are shown in Table 1. Median (range) age was 77.0 (29–90) years; 52 males (65.8%) and 27 females (34.2%) were included in the study. Median (range) Hb level was 8.1 g/dL (4.3–11.8 g/dL) in FAS, and 7.8 g/dL (4.3–10.2 g/dL) and 8.1 g/dL (4.9–11.8 g/dL) in transfusion-dependent and non-transfusion-dependent subjects, respectively. The number of transfusion-dependent cases was 15 (19.0%).
Outcomes
Rate of overall response (achievement of HI-E according to the IWG criteria 2006) was 70.9% (60.0% in transfusion-dependent cases, and 73.4% in non-transfusion-dependent cases) (Table 2). Major/minor responses were observed in 46.7% and 60.0% of the RBC transfusion-dependent subjects (n = 15). When compared levels of EPO before the treatment between non-responders (n = 23) and responders (n = 56) by the IWG criteria 2006, the levels were significantly lower in responders than non-responders (p = 0.008) (Fig. 1). The median (range) levels of non-responders and responders were 358.0 (16.7–1450.0) mIU and 66.3 (9.1–239.0) mIU/L, respectively.
EPO levels before the DA treatment in the non-responders and responders. The beeswarm boxplot of EPO levels in non-responders (N = 23) and responders (N = 56) by the IWG criteria 2006 are shown with median and the first and third quartile levels, indicating a statistical difference between them (p = 0.0008)
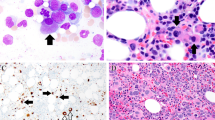
We analyzed 376 genes for mutations on 79 samples. The results are shown in Fig. 2. The highly frequent (10% or more) gene mutations included those in SF3B1 (24 cases, 30.4%), TET2 (20 cases, 25.3%), SRSF2 (10 cases, 12.7%), ASXL1 (9 cases, 11.4%), and DNMT3A (8 cases, 10.1%). As reported previously, RNA splicing- and epigenetics-regulating genes were major targets for mutations in this study.
Landscape of genetic alterations in the 83 cases. The genetic alterations in the 83 cases from this study cohort are shown. Disease classifications (FAB- and WHO 2008-based), disease risk (IPSS- and IPSS-R-based), and karyotype risks (IPSS-R karyotype risk) together with the number of affected cases are shown by color as indicated. SNV single nucleotide variant, ITD internal tandem duplication, CNA copy number alterations
At first, we studied the rate of HI-E for each number of gene mutations. The rates were 63.9% (23 cases/36 cases), 88.9% (8/9), 75.0% (9/12), 66.7% (6/9), 87.5% (7/8), 50.0% (1/2), 100.0% (1/1), 100.0% (1/1) and 0% (0/1) in 0, 1, 2, 3, 4, 5, 6, 7 and 8 mutations, respectively. The Cochran-Armitage trend test indicated that there was no correlation between numbers of gene mutations and response to DA (p = 0.7084). When compared the response between the presence or absence of gene mutations, and, the presence of > 2 or ≤ 2 gene mutations, we still could not notice any differences (p = 0.210 and 0.823, respectively).
We next evaluated the relationship between the presence of highly frequent (10% or more) mutated genes and the rate of HI-E by univariate analysis in FAS (Table 3). The univariate logistic regression analysis showed no significant association between these mutations with a frequency of ≥ 10% and therapeutic efficacy of DA. The same results were obtained when the analysis was limited to RBC non-transfusion-dependent subjects (n = 64).
In the multivariable analysis including baseline EPO levels and RBC transfusion volumes as variables, mutation of ASXL1 gene as well as baseline EPO levels was identified to independently predict poor response to DA with statistical significance (odds ratio 0.180, 95% CI 0.035–0.928, p = 0.040 for ASXL1 mutation, odds ratio 0.146, 95% confidence interval 0.042–0.503; p = 0.0023 for EPO levels) (Table 4). Transfusion volumes were not detected as predictive factors, possibly because that major part of our cohort was transfusion-independent. Response rates in subjects with low EPO (< 100 mIU/mL) + ASXL1 mutation(−) (n = 35), low EPO + ASXL1 mutation(+) (n = 5), high EPO (≥ 100 mIU/mL) + ASXL1 mutation(−), (n = 35) and high EPO + ASXL1 mutation(+) (n = 4) were 88.6, 80.0, 60.0 and 0%, respectively (Table 5). The result of chi-squared test showed that the four groups were significantly different in terms of response (p = 0.0006).
Correlation between highly frequent gene mutations and interval to the achievement of the first HI-E
Of the 79 subjects who were included in FAS, 56 subjects achieved the HI-E according to the IWG criteria 2006, and the median time to achievement (95% CI) was 7.1 weeks (6.1–10.1 weeks). After adjustment for the baseline EPO levels (cut-off, 100 mIU/mL), although none of the highly frequent gene mutations had a significant association with the time to achievement of the first HI-E according to the IWG criteria 2006, mutation of ASXL1 gene showed a tendency of later achievement: (MST of mutation(+)/mutation(−), not reached/6.7 weeks, p = 0.1649).
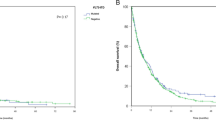
PFS and OS
Progression to AML was observed in 24 subjects from week 0 to year 1, and in 10 subjects from week 16 to year 1. A total of 23 subjects died between week 0 and year 1, and 9 subjects died between week 16 and year 1.
PFS and OS at from week 16 to year 1 after the initiation of treatment are shown on the 58 subjects who continued treatment without progression to AML until week 16 in Fig. 3 A and B. PFS (95% CI) at year 1 was 81.7% (68.6–89.7%) with MST (95% CI) of 37.7 months (29.5 months–not reached), and OS at year 1 was 83.5% (70.7–91.1%) with MST (95% CI) not reached (30.9 months–not reached).
A Progression-free survival to AML. Data in 58 subjects who continued treatment without progression to acute myelogenous leukemia till week 16. Initial date of reckoning: 16 weeks after the start of treatment. B Overall survival. Data in 58 subjects who continued treatment without progression to acute myelogenous leukemia till week 16. Initial date of reckoning: 16 weeks after the start of treatment
Safety
Grade 3/4 adverse events observed during the study period were anemia in 33 subjects (41.8%), neutrophil count decreased in 24 (30.4%), platelet count decreased in 18 (23.4%), white blood cell count decreased in 16 (20.3%), lymphocyte count decreased in 15 (19.0%), hyperglycemia in 3 (5.9%), hypoalbuminemia in 2 (3.1%), and aspartate aminotransferase increased in 1 (1.3%).
Discussion
In this study focusing on DA-eligible lower-risk MDS patients, gene mutations frequently observed in MDS were found in SF3B1 (30.4%), TET2 (25.3%), SRSF2 (12.7%), ASXL1 (11.4%), and DNMT3A (10.1%), which is consistent with a previous report [6]. The response rate of DA up to 16 weeks was 70.9% based on the IWG criteria (60.0% in transfusion-dependent cases, and 73.4% in non-transfusion-dependent cases). EPO levels before the treatment were significantly lower in the responders than non-responders. Regarding the association between gene mutations at a frequency of 10% or more and the response rate of DA, the univariate analysis showed no significant association between them. Multivariable analysis that included serum EPO levels and RBC transfusion volumes revealed that the presence of ASXL1 gene mutations and higher EPO levels (≥ 100 mIU/mL) were independent factor that predicts for poor response to DA. In a previous meta-analysis, it had been shown that the serum EPO level < 100 IU/L is a biomarker for the effectiveness of DA [26]. Similarly, in our study, DA therapy was effective in subjects with low EPO levels (< 100 mIU/mL), irrespective of the absence (response rate, 88.6%) or presence (response rate, 80.0%) of ASXL1 mutations. However, it is interesting to note that about 60% of the subjects with serum EPO levels ≥ 100mIU/mL and without ASXL1 mutations responded to DA therapy in our cohort. Even in patients with higher levels of EPO, there may be a chance to recover from anemia by DA therapy if they do not possess ASXL1 mutations. One-year PFS and OS rates was 81.7% (95% CI 68.6–89.7%) and 83.5% (70.7–91.1%), respectively. Considering that our cohort included 5 subjects with RAEB-1 according to the WHO classification, the PFS and OS were not worse than expected.
DA is an ESA in which sustainable serum concentration has been obtained by substituting 5 amino acids in EPO [27, 28]. Like EPO, DA binds to erythropoietin receptors and thereby promotes erythropoiesis in early and late erythroid progenitor cells in the bone marrow [27, 29]. When injected subcutaneously once a week, sufficient serum levels are maintained for the treatment of anemia [28]. Nine studies performed in patients with MDS reported response rates to DA according to the IWG 2000 criteria with a range of 38–72.5% within 12–24 weeks [26]. Similarly, in the present study, overall response rate to DA at week 16 was 70.9% according to the IWG criteria 2006. There was a tendency that non-transfusion-dependent subjects had a better response to DA than transfusion-dependent subjects, with ORR of 73.4 and 60.0%, respectively. The earlier commencement of DA could enable avoidance of transfusion dependency in anemic patients with lower-risk MDS.
Kosmider et al. have reported that having > 2 somatic mutations was associated with lower HI-E in the ESA treatments for lower-risk MDS [30]. This result was opposite to ours. In our study, there was no co-relation between numbers of gene mutations and response to DA (p = 0.7084). Even though we divided patients into two groups by the mutation numbers of > 2 or ≤ 2 like in their study, no differences in the response were observed (p = 0.823). Although the sample size was the same (n = 79) and response rates were similar (70.9 and 64.5% according to the IWG 2006 criteria in our and their studies), these two studies had quite different designs. Our study was prospective, while Kosmider et al.’s study retrospective. Patients in our cohort were consistently treated with DA at a dose of 240 μg/week, while those in their cohort with EPO or DA at various doses with or without G-CSF. We analyzed 326 genes for mutations, but they only 37 genes. All these may have caused different conclusions.
They also claimed that individual mutations of the frequently mutated genes had no significant impact on HI-E by the univariate analysis, which was the same result as ours. Importantly, however, by using multivariable analysis that included serum EPO level and RBC transfusion volumes as variables, we showed that the presence of ASXL1 mutations besides EPO level was significantly associated with poor response to DA among the highly frequent (> 10%) gene mutations observed in this study such as those in SF3B1, TET2, SRSF2, ASXL1, and DNMT3A. Because MDS are heterogenous not only in morphology but also in molecular pathogenesis, it was difficult for less frequent gene mutations to evaluate their predictive value on the DA treatment. Another important result of this study was that ASXL1 gene mutations were also correlated with possible prolonged interval to the achievement of the first HI-E. ASXL1 mutations are known genetic factors that predict unfavorable clinical courses [31], with a high rate of progression to AML [32]. Considering a balance between cost and benefit, DA perhaps should not be applied to patients with lower-risk MDS showing a higher level of EPO and carrying ASXL1 mutations.
ASXL1 is an epigenetics-regulating gene that supports the functions of polycomb complex PRC1 and represses the expression of oncogenes and other genes through methylation of K4 in histone H3 [33]. It has also been shown that mutant ASXL1 disrupts the function of PRC1 and causes derepression of expression in target genes [34], which possibly leads to the development of myeloid malignancies, including MDS [35]. The candidate target genes for the derepression include HOXA9 and MIR125A [36]. While HOXA9 is a known oncogene in hematopoietic tumors of the myeloid lineage [37], MIR125A is suggested to impair hematopoietic cell differentiation [38]. On the other hand, Shi et al. reported that ASXL1 loss impairs erythroid development and hinders erythroid differentiation [39], indicating that ineffective erythropoiesis of MDS may occur as a result of ASXL1 mutation. Although the precise mechanism in a regard to poor response to DA could not be identified for ASXL1-mutated subjects, the mutation could induce refractoriness to DA. From another point of view, Raimbault et al. reported that the low expressions of CD117/c-KIT+ in lower-risk MDS erythroid precursors was correlated with ESA failure [40]. It would be interesting to analyze the association between ASXL1 gene mutations and expression levels of CD117/c-KIT+ in a future study.
This prospective study provided the first evidence in the ESA therapy that the existence of some specific gene mutations (ASXL1 mutations) may be associated with response to specific treatments (DA). In our opinion, even though patients with lower-risk MDS show higher EPO levels, DA would be effective if they do not carry ASXL1 mutations. However, when patients have both the predictive factors of poor response, namely, higher levels of EPO and ASXL1 mutations, alternative therapies would be recommended as the first-line therapy for anemia. One of such candidates may be luspatercept which is a recombinant fusion protein binding TGF-β superfamily ligands and is effective in patients with increased ring sideroblasts and/or SF3B1 mutations [41]. Even in cytokine and other supportive therapies for anemia, molecular stratification needs to be established to determine their application in the near future.
References
Gangat N, Patnaik MM, Tefferi A. Myelodysplastic syndromes: contemporary review and how we treat. Am J Hematol. 2016;91:6–89.
Gidaro A, Deliliers GL, Gallipoli P, Arquati M, Wu MA, Castelli R. Laboratory and clinical risk assessment to treat myelodysplatic syndromes. Clin Chem Lab Med. 2016;54:1411–26.
Sperling AS, Gibson CJ, Ebert BL. The genetics of myelodysplastic syndrome: from clonal haematopoiesis to secondary leukaemia. Nat Rev Cancer. 2017;17:5–19.
Shallis RM, Ahmad R, Zeidan AM. The genetic and molecular pathogenesis of myelodysplastic syndromes. Eur J Haematol. 2018;101:260–71.
Bejar R, Levine R, Ebert BL. Unraveling the molecular pathophysiology of myelodysplastic syndromes. J Clin Oncol. 2011;29:504–15.
Ochi Y, Kon A, Sakata T, Nakagawa MM, Nakazawa N, Kakuta M, et al. Combined cohesin-RUNX1 deficiency synergistically perturbs chromatin loo** and causes myelodysplastic syndromes. Cancer Discov. 2020;10:836–53.
Makishima H, Yoshizato T, Yoshida K, Sekeres MA, Radivoyevitch T, Suzuki H, et al. Dynamics of clonal evolution in myelodysplastic syndromes. Nat Genet. 2017;49:204–12.
Yoshida K, Sanada M, Shiraishi Y, Nowak D, Nagata Y, Yamamoto R, et al. Frequent pathway mutations of splicing machinery in myelodysplasia. Nature. 2011;478:64–9.
Ogawa S. Genetics of MDS. Blood. 2019;133:1049–59.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Santini V. Anemia as the main manifestation of myelodysplastic syndromes. Semin Hematol. 2015;52:348–56.
Malcovati L, Della Porta MG, Cazzola M. Predicting survival and leukemic evolution in patients with myelodysplastic syndrome. Haematologica. 2006;91:1588–90.
Malik J, Kim AR, Tyre KA, Cherukuri AR, Palis J. Erythropoietin critically regulates the terminal maturation of murine and human primitive erythroblasts. Haematologica. 2013;98:1778–87.
Hellström-Lindberg E, van de Loosdrecht A. Erythropoiesis stimulating agents and other growth factors in low-risk MDS. Best Pract Res Clin Haematol. 2013;26:401–10.
Jädersten M, Montgomery SM, Dybedal I, Porwit-MacDonald A, Hellström-Lindberg E. Long-term outcome of treatment of anemia in MDS with erythropoietin and G-CSF. Blood. 2005;106:803–11.
Greenberg PL, Sun Z, Miller KB, Bennett JM, Tallman MS, Dewald G, et al. Treatment of myelodysplastic syndrome patients with erythropoietin with or without granulocyte colony-stimulating factor: results of a prospective randomized phase 3 trial by the Eastern Cooperative Oncology Group (E1996). Blood. 2009;114:2393–400.
Jang JH, Harada H, Shibayama H, Shimazaki R, Kim HJ, Sawada K, et al. A randomized controlled trial comparing darbepoetin alfa doses in red blood cell transfusion-dependent patients with low- or intermediate-1 risk myelodysplastic syndromes. Int J Hematol. 2015;102:401–12.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Hellström-Lindberg E, Gulbrandsen N, Lindberg G, Ahlgren T, Dahl IM, Dybedal I, et al. A validated decision model for treating the anaemia of myelodysplastic syndromes with erythropoietin + granulocyte colony-stimulating factor: significant effects on quality of life. Br J Haematol. 2003;120:1037–46.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–99.
Swerdlow SH, Campo E, Harris NL, editors. WHO classification of tumours of haematopoietic and lymphoid tissues, revised. 4th ed. Lyon: International Agency for Research on Cancer; 2017.
Yoshizato T, Nannya Y, Atsuta Y, Shiozawa Y, Iijima-Yamashita Y, Yoshida K, et al. Genetic abnormalities in myelodysplasia and secondary acute myeloid leukemia: impact on outcome of stem cell transplantation. Blood. 2017;129:2347–58.
Shiraishi Y, Sato Y, Chiba K, Okuno Y, Nagata Y, Yoshida K, et al. An empirical Bayesian framework for somatic mutation detection from cancer genome sequencing data. Nucleic Acids Res. 2013;41: e89.
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD, et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006;108:419–25.
NCI. CTCAE. 2010. http://evs.nci.nih.gov/ftp1/CTCAE/About.html.
Park S, Fenaux P, Greenberg P, Mehta B, Callaghan F, Kim C, et al. Efficacy and safety of darbepoetin alpha in patients with myelodysplastic syndromes: a systematic review and meta-analysis. Br J Haematol. 2016;174:730–47.
Egrie JC, Browne JK. Development and characterization of novel erythropoiesis stimulating protein (NESP). Br J Cancer. 2001;84(Suppl 1):3–10.
Egrie JC, Dwyer E, Browne JK, Hitz A, Lykos MA. Darbepoetin alfa has a longer circulating half-life and greater in vivo potency than recombinant human erythropoietin. Exp Hematol. 2003;31:290–9.
Elliott S, Pham E, Macdougall IC. Erythropoietins: a common mechanism of action. Exp Hematol. 2008;36:1573–84.
Kosmider O, Passet M, Santini V, Platzbecker U, Andrieu V, Zini G, et al. Are somatic mutations predictive of response to erythropoiesis stimulating agents in lower risk myelodysplastic syndromes? Haematologica. 2016;101:e280–3.
Thol F, Friesen I, Damm F, Yun H, Weissinger EM, Krauter J, et al. Prognostic significance of ASXL1 mutations in patients with myelodysplastic syndromes. J Clin Oncol. 2011;29:2499–506.
Chen TC, Hou HA, Chou WC, Tang JL, Kuo YY, Chen CY, et al. Dynamics of ASXL1 mutation and other associated genetic alterations during disease progression in patients with primary myelodysplastic syndrome. Blood Cancer J. 2014;4: e177.
Kato M. Functional and cancer genomics of ASXL family members. Br J Cancer. 2013;109:299–306.
Abdel-Wahab O, Gao J, Adli M, Dey A, Trimarchi T, Chung YR, et al. ASXL1 mutations promote myeloid transformation through loss of PRC2-mediated gene repression. Cancer Cell. 2012;22:180–93.
Wang J, Li Z, He Y, Pan F, Chen S, Rhodes S, et al. Loss of Asxl1 leads to myelodysplastic syndrome-like disease in mice. Blood. 2014;123:541–53.
Inoue D, Kitaura J, Togami K, Nishimura K, Enomoto Y, Uchida T, et al. Myelodysplastic syndromes are induced by histone methylation-altering ASXL1 mutations. J Clin Invest. 2013;123:4627–40.
Li J, Shen H, Himmel KL, Dupuy AJ, Largaespada DA, Nakamura T, et al. Leukaemia disease genes: large-scale cloning and pathway predictions. Nat Genet. 1999;23:348–53.
Gerrits A, Walasek MA, Olthof S, Weersing E, Ritsema M, Zwart E, et al. Genetic screen identifies microRNA cluster 99b/let-7e/125a as a regulator of primitive hematopoietic cells. Blood. 2012;119:377–87.
Shi H, Yamamoto S, Sheng M, Bai J, Zhang P, Chen R, et al. ASXL1 plays an important role in erythropoiesis. Sci Rep. 2016;6:28789.
Raimbault A, Itzykson R, Willems L, Rousseau A, Chapuis N, Mathis S, et al. The fraction of CD117/c-KIT-expressing erythroid precursors predicts ESA response in low-risk myelodysplastic syndromes. Cytom B Clin Cytom. 2019;96:215–22.
Fenaux P, Platzbecker U, Mufti GJ, Garcia-Manero G, Buckstein R, Santini V, et al. Luspatercept in patients with lower-risk myelodysplastic syndromes. N Engl J Med. 2020;382:140–51.
Acknowledgements
This study was funded by Kyowa Kirin Co., Ltd., and was supported by the Ministry of Education, Culture, Sports, Science and Technology under Grant number hp160219 and hp200138 and by AMED under Grand number JP20cm0106501h0005 to SO. We would like to thank all of the participated patients and their families. We are indebted to the physicians, all other co-medical staff and Independent Data Monitoring Committee (Shuji Nakano, Naohito Fujishima and Kenichi Yoshimura) who contributed to this study. We also thank the stuffs at the Clinical Research Support Center Kyushu (CReS Kyushu) for their excellent collection and management of data, secretarial assistance, and any other support.
Author information
Authors and Affiliations
Contributions
Contribution: MI, HK, HS, YMo, YMa, KT, TM, TH, and KM designed the study; MI, HK, HS, YMo, YMa, KT, TM, TH, and HH collected clinical data; YN, YT, SM, and SO performed sample preparation and sequencing; MI, HK, HS, YMo, YMa, KT, TM, TH, YN, HH, IM, SO, KA, YK, and KM analyzed data; JK performed statistical analysis; MI, HK, HS, YMo, YMa, KT, TM, TH, YN, YT, SM, JK, YN, SO, and KM wrote the manuscript; and all of the authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
YN (Otsuka Pharmaceutical Co., Ltd.), HK (Nippon Shinyaku Co., Ltd., Ono Pharmaceutical Co., Ltd.), SM (Fujitsu Limited), SO (Chordia Therapeutics Inc., Kan Research Institute, Inc., Otsuka Pharmaceutical Co., Ltd.), and KA (Sumitomo Dainippon Pharma Co., Ltd., Kyowa Kirin Co., Ltd.) are consultants for each company. SO has an ownership interests (including stock options) in a start-up company, the stock of which is not publicly traded for RegCell Co., Ltd., Asahi Genomics Co., Ltd., and Chordia Therapeutics, Inc. YM (Eisai Co., Ltd.), HS (Astellas Pharma Inc., Tei** Ltd., Shionogi Co., Ltd, Taiho, Pharmaceutical Co., Ltd., Eisai Co., Ltd., Celgene Corporation, Ono Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., MSD K.K., Sumitomo Dainippon Pharma Co., Ltd., Nippon Shinyaku Co., Ltd, Daiichi Sankyo Co., Ltd.), YM (Kyowa Kirin Co., Ltd.), SM (DeNA Life Science Inc.), IM (Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Ono Pharmaceutical Co., Ltd., Kyowa Kirin Co., Ltd., Shionogi Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., Asahi Kasei Pharma Corporation, Takeda Pharmaceutical Co., Ltd., Nippon Shinyaku Co., Ltd., Pfizer Japan Inc., Taiho Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Nihon Pharmaceutical Co., Ltd., Novartis Pharma K.K., Daiichi Sankyo Co., Ltd., MSD K.K., Japan Blood Products Organization, Otsuka Pharmaceutical Co., Ltd., Mundipharma K.K., AbbVie GK, Sanofi K.K., Ayumi Pharmaceutical Corporation, Eli Lilly Japan K.K.), SO (Sumitomo Dainippon Pharma Co., Ltd., Chordia Therapeutics Inc., Otsuka Pharmaceutical Co., Ltd., Eisai Co., Ltd.), KA (Celgene Corporation, Kyowa Kirin Co., Ltd, Astellas Pharma Inc., Shionogi Co., Ltd., Asahi Kasei Pharma Corporation, Chugai Pharmaceutical Co., Ltd, Bristol-Myers Squibb Co.), KM (Novartis Pharma K.K., Kyowa Kirin Co., Ltd., Chugai Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd.) have received the research funding of each companies. YM (Kyowa Kirin Co., Ltd.), MI (Kyowa Kirin Co., Ltd., Janssen Pharmaceutical K.K., Novartis Pharma K.K., Takeda Pharmaceutical Co., Ltd.), HS (Takeda Pharmaceutical Co., Ltd., Novartis Pharma K.K., Celgene Corporation, Janssen Pharmaceutical K.K., Chugai Pharmaceutical Co., Ltd., Kyowa Kirin Co., Ltd., Ono Pharmaceutical Co., Ltd, Eisai Co., Ltd., Nippon Shinyaku Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., Bristol-Myers Squibb Co., Pfizer Japan Inc., Fujimoto Pharmaceutical Corporation), YM (Kyowa Kirin Co., Ltd), TM (Bristol-Myers Squibb Co., Otsuka Pharmaceutical Co., Ltd., MSD K.K., Astellas Pharma Inc., Amgen Astellas Biopharma K.K., Celgene Corporation, AbbVie GK, Takeda Pharmaceutical Co., Ltd.), HK (Kyowa Kirin Co., Ltd., Novartis Pharma K.K., Chugai Pharmaceutical Co., Ltd.), SM (Ministry of Health, Labour and Welfare, Japan Science and Technology Agency, National Institutes of Biomedical Innovation, Health and Nutrition), IM (Pfizer Japan Inc., Novartis Pharma K.K., Daiichi Sankyo Co., Ltd., Astellas Pharma Inc., Otsuka Pharmaceutical Co., Ltd., Bristol-Myers Squibb Co.) have directly received honoraria from an entity. Seishi Ogawa (Qiagen K.K.) has received patents and royalties. KM (Celgene Corporation, Kyowa Kirin Co., Ltd.) has received a fee of expert testimony. HS (Chugai Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., AbbVie GK, AstraZeneca), and SM (Uehara Foundation, Nakagani Foundation, Otsuka Foundation, Okawa Foundation) are assigned as an entity's board of directors, speakers bureau, or its advisory committees. HH, TH, KT, HT, JK and YK have no COI to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Morita, Y., Nannya, Y., Ichikawa, M. et al. ASXL1 mutations with serum EPO levels predict poor response to darbepoetin alfa in lower-risk MDS: W-JHS MDS01 trial. Int J Hematol 116, 659–668 (2022). https://doi.org/10.1007/s12185-022-03414-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03414-9