Abstract
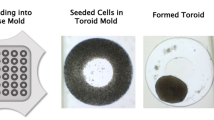
Since March 2013, animal testing for toxicity evaluation of cosmetic ingredients is banned in Europe. This directive applies to all personal care ingredients including oral ingredients. Gingival in vitro 3D models are commercially available. However, it is essential to develop “in house model” to modulate several parameters to study oral diseases, determine the toxicity of ingredients, test biocompatibility, and evaluate different formulations of cosmetic ingredients. Our expertise in tissue engineering allowed us to reconstruct human oral tissues from normal human gingival cells (fibroblasts and keratinocytes). Indeed, isolation from surgical leftover was performed to culture these gingival cells. These cells keep their endogenous capacity to proliferate allowing reconstruction of equivalent tissue close to in vivo tissue. Reconstruction of gingival epithelium, chorion equivalent, and the combination of these two tissues (full thickness) using primary gingival cells displayed all characteristics of an in vivo gingival model.






Similar content being viewed by others
References
Adams D (1975) Keratinization of the oral epithelium. Ann R Coll Surg Engl 58(5):351
Atukorallaya DS, Ratnayake RK (2021) Oral mucosa, saliva, and COVID-19 infection in oral health care. Front Med 8:656926
Bandara HMHN, Samaranayake LP (2019) Viral, bacterial, and fungal infections of the oral mucosa: types, incidence, predisposing factors, diagnostic algorithms, and management. Periodontology 2000 80(1):148–176
Capallere C, Plaza C, Meyrignac C, Arcioni M, Brulas M, Busuttil V, Garcia I, Bauza E, Botto JM (2018) Property characterization of reconstructed human epidermis equivalents, and performance as a skin irritation model, Toxicology in Vitro, Volume 53. ISSN 45–56:0887–2333
Chaudhari KS, Akamanchi KG (2019) Novel bicephalous heterolipid based self-microemulsifying drug delivery system for solubility and bioavailability enhancement of efavirenz. Int J Pharm 560:205–218
Garzón-Bello I.J, and Ibáñez Cortés M (2021) Study of the histological and anatomical characteristics of the human oral mucosa. A step towards the developement of tailored-artificial oral mucosa. Actualidad Médica 813
Groeger S, Joerg M (2019) Oral mucosal epithelial cells. Front Immunol 10:208
Hovav AH (2014) Dendritic cells of the oral mucosa. Mucosal Immunol 7(1):27–37
Imamura T (2003) The role of gingipains in the pathogenesis of periodontal disease. J Periodontol 74(1):111–8
Jia L, Han N, Du J, Guo L, Luo Z, Liu Y (2019) Pathogenesis of important virulence factors of Porphyromonas gingivalis via Toll-like receptors. Front Cell Infect Microbiol 9:262
** SH et al (2015) Isolation and characterization of human mesenchymal stem cells from gingival connective tissue. J Periodontal Res 50(4):461–467
Klausner M, Handa Y, Aizawa S (2021) In vitro three-dimensional organotypic culture models of the oral mucosa. In Vitro Cell Dev Biol-Anim 57:148–159
Koskinen Holm C, Qu C (2022) Engineering a 3D in vitro model of human gingival tissue equivalent with genipin/cytochalasin D. Int J Mol Sci 23(13):7401
Krishnan PA (2009) Fungal infections of the oral mucosa. Indian J Dent Res 23(5):650
Li N, Collyer CA (2011) Gingipains from Porphyromonas gingivalis. Complex domain structures confer diverse functions. Eur J Microbiol Immunol (Bp) 1(1):41–58
Li X, Zhang B, Wang H, Zhao X, Zhang Z, Ding G, Wei F (2020) The effect of aging on the biological and immunological characteristics of periodontal ligament stem cells. Stem Cell Res Ther 11:1–15
Mitrano TI et al (2010) Culture and characterization of mesenchymal stem cells from human gingival tissue. J Periodontol 81(6):917–925
Moharamzadeh K, Colley H, Murdoch C et al (2012) Tissue-engineered oral mucosa. J Dent Res 91(7):642–650
Moll R, Franke WW, Schiller DL, Geiger B, Krepler R (1982) The catalog of human cytokeratins: patterns of expression in normal epithelia, tumors and cultured cells. Cell 31:11–24
Peehl D, Ham R (1980) Growth and differentiation of human keratinocytes without a feeder layer or conditioned medium. In Vitro 16:516–525
Rheinwald JG, Green H (1975) Serial cultivation of strains of human epidermal keratinocytes: the formation of keratinizing colonies from single cells. Cell 6:33
Rosdy M, Clauss LC (1990) Terminal epidermal differentiation of human keratinocytes grown in chemically defined medium on inert filter substrates at the air-liquid interface. J Invest Dermatol 95:409–414
Russell WMS, Burch RL (1959) The principles of humane experimental technique. London: Methuen & Co. Special edition. Universities Federation for Animal Welfare (UFAW), pp 1992
Schneeberger EE, Lynch RD (2004) The tight junction: a multifunctional complex. Am J Physiol Cell Physiol 286:C1213–C1228
Şenel S (2021) An overview of physical, microbiological and immune barriers of oral mucosa. Int J Mol Sci 22(15):7821
Shimono M, Ishikawa T, Enokiya Y, Muramatsu T, Matsuzaka K, Inoue T, Abiko Y, Yamaza T, Kido MA, Tanaka T, Hashimoto S (2003) Biological characteristics of the junctional epithelium. J Electron Microsc (Tokyo) 52(6):627–639
Shirato M, Nakamura K, Tenkumo T, Kano Y, Ishiyama K, KannoT,Sasaki K, Niwano Y, Matsuura H (2019) Oral mucosal irritation potential of antimicrobial chemotherapy involving hydrogen peroxide photolysis with high-power laser irradiation for the treatment of periodontitis J Photochem Photobiol B 201, Article 111633.
Souza LR, Oliveira MVM, Basile JR et al. (2015) Anatomical and physiopathological aspects of oral cavity and oropharynx components related to oropharyngeal dysphagia. In: Seminars in dysphagia. InTech. https://doi.org/10.5772/60766
Squier C, Brogden K (2010) Human oral mucosa: development, structure and function. Wiley
Squier CA, Kremer MJ (2001) Biology of oral mucosa and esophagus. J Natl Cancer Inst Monogr 29:7–15
Su L, Morgan PR, Lane EB (1994) Protein and mRNA expression of simple epithelial keratins in normal, dysplastic, and malignant oral epithelia. Am J Pathol 145:1349–1357
Takahashi N, Sulijaya B, Yamada-Hara M, Tsuzuno T, Tabeta K, Yamazaki K (2019) Gingival epithelial barrier: regulation by beneficial and harmful microbes. Tissue Barriers 7(3)
Tuddenham S, Sears CL (2015) The intestinal microbiome and health. Curr Opin Infect Dis 28(5):464–70
Vijayashree RJ, Sivapathasundharam B (2022) The diverse role of oral fibroblasts in normal and disease. J Oral Maxillofac Pathol: JOMFP 26(1):6
Villalobos V, Garrido M, Reyes A, Fernández C, Diaz C, Torres V, Cáceres M (2022) Aging envisage imbalance of the periodontium: a keystone in oral disease and systemic health. Front Immunol 13:1044334
Yadev NR, Murdoch C, Saville SP, Thornhill MH (2011) Evaluation of tissue engineered models of the oral mucosa to investigate oral candidiasis. Microb Pathog 50(6):278–285
Acknowledgements
I thank Doctor Hagege for his expertise in oral medicine and support in this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Plaza, C., Capallere, C., Meyrignac, C. et al. Development of 3D gingival in vitro models using primary gingival cells. In Vitro Cell.Dev.Biol.-Animal (2024). https://doi.org/10.1007/s11626-024-00923-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11626-024-00923-1