Abstract
Background
The volume-outcome relationship has been well-established for pancreaticoduodenectomy (PD). It remains unclear if this is primarily driven by hospital volume or individual surgeon experience.
Objective
This study aimed to determine the relationship of hospital and surgeon volume on short-term outcomes of patients with pancreatic adenocarcinoma undergoing PD.
Methods
Patients >65 years of age who underwent PD for pancreatic adenocarcinoma were identified from the Surveillance, Epidemiology, and End Results (SEER)–Medicare database (2008–2015). Analyses were stratified by hospital volume and then surgeon volume, creating four volume cohorts: low-low (low hospital, low surgeon), low-high (low hospital, high surgeon), high-low (high hospital, low surgeon), high-high (high hospital, high surgeon). Propensity scores were created for the odds of undergoing surgery with high-volume surgeons. Following matching, multivariable analysis was used to assess the impact of surgeon volume on outcomes within each hospital volume cohort.
Results
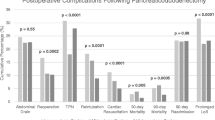
In total, 2450 patients were identified: 54.3% were treated at high-volume hospitals (27.0% low-volume surgeons, 73.0% high-volume surgeons) and 45.7% were treated at low-volume hospitals (76.9% low-volume surgeons, 23.1% high-volume surgeons). On matched multivariable analysis, there were no significant differences in the risk of major complications, 90-day mortality, and 30-day readmission based on surgeon volume within the low and high hospital volume cohorts.
Conclusion
Compared with surgeon volume, hospital volume is a more significant factor in predicting short-term outcomes after PD. This suggests that a focus on resources and care pathways, in combination with volume metrics, is more likely to achieve high-quality care for patients undergoing PD across all hospitals.


Similar content being viewed by others
References
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. New Engl J Med. 2002;346(15):1128–37.
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. New Engl J Med. 2003;349(22):2117–27.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. New Engl J Med. 2011;364(22):2128–37.
Mamidanna R, Ni Z, Anderson O, Spiegelhalter SD, Bottle A, Aylin P, et al. Surgeon volume and cancer esophagectomy, gastrectomy, and pancreatectomy: a population-based study in England. Ann Surg. 2016;263(4):727–32.
Hata T, Motoi F, Ishida M, Naitoh T, Katayose Y, Egawa S, et al. Effect of hospital volume on surgical outcomes after pancreaticoduodenectomy: a systematic review and meta-analysis. Ann Surg. 2016;263(4):664–72.
Eppsteiner RW, Csikesz NG, McPhee JT, Tseng JF, Shah SA. Surgeon volume impacts hospital mortality for pancreatic resection. Ann Surg. 2009;249(4):635–40.
McPhee JT, Hill JS, Whalen GF, Zayaruzny M, Litwin DE, Sullivan ME, et al. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007;246(2):246–53.
de Geus SWL, Hachey KJ, Nudel JD, Ng SC, McAneny DB, Davies JD, et al. Volume of pancreas-adjacent operations favorably influences pancreaticoduodenectomy outcomes at lower volume pancreas centers. Ann Surg. 2020;1:2. https://doi.org/10.1097/SLA.0000000000004432.
Hachey K, Morgan R, Rosen A, Rao SR, McAneny D, Tseng J, et al. Quality comes with the (anatomic) territory: evaluating the impact of surgeon operative mix on patient outcomes after pancreaticoduodenectomy. Ann Surg Oncol. 2018;25(13):3795–803.
Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010;145(7):634–40.
Stella M, Bissolati M, Gentile D, Arriciati A. Impact of surgical experience on management and outcome of pancreatic surgery performed in high- and low-volume centers. Updates Surg. 2017;69(3):351–8.
Enomoto LM, Gusani NJ, Dillon PW, Hollenbeak CS. Impact of surgeon and hospital volume on mortality, length of stay, and cost of pancreaticoduodenectomy. J Gastrointest Surg. 2014;18(4):690–700.
SEER-Medicare Linked Database: National Cancer Institute. Available at: https://healthcaredelivery.cancer.gov/seermedicare/.
Surveillance, Epidemiology, and End Results Program NIH National Cancer Institute. Available at: www.seer.cancer.gov.
Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250(6):1029–34.
Hyder O, Dodson RM, Nathan H, Schneider EB, Weiss MJ, Cameron JL, et al. Influence of patient, physician, and hospital factors on 30-day readmission following pancreatoduodenectomy in the United States. JAMA Surg. 2013;148(12):1095–102.
Nathan H, Atoria CL, Bach PB, Elkin EB. Hospital volume, complications, and cost of cancer surgery in the elderly. J Clin Oncol. 2015;33(1):107–14.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–33.
Elixhauser Comorbidity Software, Version 3.7: Agency for Healthcare Research and Quality (AHRQ). https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp
Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80(1):27–38.
Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21(16):2409–19.
Ho V, Heslin MJ. Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann Surg. 2003;237(4):509–14.
Kennedy TJ, Cassera MA, Wolf R, Swanstrom LL, Hansen PD. Surgeon volume versus morbidity and cost in patients undergoing pancreaticoduodenectomy in an academic community medical center. J Gastrointest Surg. 2010;14(12):1990–6.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49(12):1076–81.
van Rijssen LB, Zwart MJ, van Dieren S, de Rooij T, Bonsing BA, Bosscha K, et al. Variation in hospital mortality after pancreatoduodenectomy is related to failure to rescue rather than major complications: a nationwide audit. HPB (Oxford). 2018;20(8):759–67.
Sheetz KH, Chhabra KR, Smith ME, Dimick JB, Nathan H. Association of discretionary hospital volume standards for high-risk cancer surgery with patient outcomes and access, 2005–2016. JAMA Surg. 2019;154(11):1005–12.
Funding
Marianna Papageorge is supported by a T32 Grant through Boston University School of Medicine (award #T32HP10028), and Alison Woods is supported by a T32 grant through Johns Hopkins University School of Medicine, from the National Institutes of Health (National Cancer Institute award #T32CA126607). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH and supporting institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Marianna V. Papageorge, Susanna W.L. de Geus, Alison P. Woods, Sing Chau Ng, David McAneny, Jennifer F. Tseng, Kelly M. Kenzik, and Teviah E. Sachs have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Papageorge, M.V., de Geus, S.W.L., Woods, A.P. et al. The Effect of Hospital Versus Surgeon Volume on Short-Term Patient Outcomes After Pancreaticoduodenectomy: a SEER–Medicare Analysis. Ann Surg Oncol 29, 2444–2451 (2022). https://doi.org/10.1245/s10434-021-11196-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-11196-3