Abstract
Background
Performance of pancreaticoduodenectomy (PD) in high-volume centers has been posited to improve postoperative morbidity and mortality, consistent with the volume-outcomes hypothesis. We sought to evaluate the impact of hospital volume on 90-day PD outcomes at hepatopancreatobiliary (HPB) centers within a regionalized system.
Methods
A retrospective population-based observational cohort study was performed, using administrative records of patients undergoing PD between 2005 and 2013 in Ontario, Canada. Postoperative administrative codes were used to define complications. Patients’ 90-day postoperative outcomes were compared between center-volume categories using chi-square tests and multivariable regression. Volume cutoffs were defined using minimal regional standards (20PD/year), with assessment of the impact of further volume increases.
Results
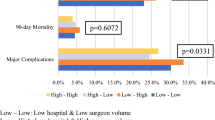
Of 2660 patients, 2563 underwent PD at HPB centers. Of these, 38.9% underwent surgery at higher-volume centers (>40 PD/year), 36.9% at medium-volume centers (20–39 PD/year), and 24.1% at lower-volume centers (10–19 PD/year). Mortality (30- and 90-day) was lowest at higher-volume hospitals (1.5%, 2.7%, respectively) compared to medium-volume (3.9%, 6.3%) and lower-volume hospitals (2.9%, 5.2%) (p < 0.01). Patients treated at higher- and medium-volume centers had lower reoperation rates (10.3%, 10.7% vs. 16.7%, p = 0.0002) and less prolonged length of stay (23.2%, 22.0% vs. 31.6%, p < 0.0001) compared to lower-volume centers.
Conclusion
Progressive increases in hospital volume correspond to improved 90-day outcomes following PD.


Similar content being viewed by others
References
Donahue TR, Reber HA. Surgical management of pancreatic cancer—pancreaticoduodenectomy. Seminars in oncology. 2015;42(1):98-109. doi:10.1053/j.seminoncol.2014.12.009.
Are C, Dhir M, Ravipati L. History of pancreaticoduodenectomy: early misconceptions, initial milestones and the pioneers. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2011;13(6):377-84. doi:10.1111/j.1477-2574.2011.00305.x.
Lai EC, Lau SH, Lau WY. Measures to prevent pancreatic fistula after pancreatoduodenectomy: a comprehensive review. Archives of Surgery. 2009;144(11):1074-80.
Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. Journal of Gastrointestinal Surgery. 2006;10(9):1199-211.
Allen PJ, Gönen M, Brennan MF, Bucknor AA, Robinson LM, Pappas MM et al. Pasireotide for postoperative pancreatic fistula. New England Journal of Medicine. 2014;370(21):2014-22.
Vollmer CM. The economics of pancreas surgery. Surgical Clinics of North America. 2013;93(3):711-28.
Enestvedt CK, Diggs BS, Cassera MA, Hammill C, Hansen PD, Wolf RF. Complications nearly double the cost of care after pancreaticoduodenectomy. The American Journal of Surgery. 2012;204(3):332-8.
Ihse I. The volume-outcome relationship in cancer surgery: a hard sell. Annals of surgery. 2003;238(6):777.
Hata T, Motoi F, Ishida M, Naitoh T, Katayose Y, Egawa S et al. Effect of Hospital Volume on Surgical Outcomes After Pancreaticoduodenectomy: A Systematic Review and Meta-analysis. Annals of surgery. 2015. doi:10.1097/SLA.0000000000001437.
Marcaccio M, Langer, B., Rumble, B., Hunter, A.; Expert Panel on HPB Surgical Oncology. Hepatic, pancreatic, and biliary tract (HPB) surgical oncology standards. Program in Evidence-based Care Practice Guideline Report. Toronto (ON): Cancer Care Ontario; 2006.
Schultz SE, Rothwell DM, Chen Z, Tu K. Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic diseases and injuries in Canada. 2013;33(3):160-6.
Kralj B. Measuring “rurality” for purposes of health-care planning: an empirical measure for Ontario. Ontario Med Rev. 2000;67:33-52.
Mackillop WJ, Zhang-Salomons J, Groome PA, Paszat L, Holowaty E. Socioeconomic status and cancer survival in Ontario. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1997;15(4):1680-9.
Kagedan DJ, Abraham L, Goyert N, Li Q, Paszat LF, Kiss A et al. Beyond the dollar: Influence of sociodemographic marginalization on surgical resection, adjuvant therapy, and survival in patients with pancreatic cancer. Cancer. 2016;122(20):3175-82. doi:10.1002/cncr.30148.
Reid RJ, Roos NP, MacWilliam L, Frohlich N, Black C. Assessing population health care need using a claims-based ACG morbidity measure: a validation analysis in the Province of Manitoba. Health services research. 2002;37(5):1345-64.
Reid RJ, MacWilliam L, Verhulst L, Roos N, Atkinson M. Performance of the ACG case-mix system in two Canadian provinces. Medical care. 2001;39(1):86-99.
Nam RK, Cheung P, Herschorn S, Saskin R, Su J, Klotz LH et al. Incidence of complications other than urinary incontinence or erectile dysfunction after radical prostatectomy or radiotherapy for prostate cancer: a population-based cohort study. The Lancet Oncology. 2014;15(2):223-31. doi:10.1016/S1470-2045(13)70606-5.
Tee MC, Shubert CR, Ubl DS, Habermann EB, Nagorney DM, Que FG. Preoperative anemia is associated with increased use of hospital resources in patients undergoing elective hepatectomy. Surgery. 2015;158(4):1027-36; discussion 36-8. doi:10.1016/j.surg.2015.06.004.
Offodile AC, 2nd, Aherrera A, Guo L. Risk factors associated with prolonged postoperative stay following free tissue transfer: an analysis of 2425 patients from the American College of Surgeons National Surgical Quality Improvement Program database. Plastic and reconstructive surgery. 2014;134(6):1323-32. doi:10.1097/PRS.0000000000000735.
Gershman B, Moreira DM, Boorjian SA, Lohse CM, Cheville JC, Costello BA et al. Comprehensive Characterization of the Perioperative Morbidity of Cytoreductive Nephrectomy. European urology. 2016;69(1):84-91. doi:10.1016/j.eururo.2015.05.022.
Zetlen H, Daratha KB, Harper JD, Wessells H, Roberts KP, Gore JL. Hospital-level Variation in the Quality of Benign Inpatient Urologic Surgery. Urology. 2015. doi:10.1016/j.urology.2015.07.067.
Wright FC, Fitch M, Coates AJ, Simunovic M. A qualitative assessment of a provincial quality improvement strategy for pancreatic cancer surgery. Annals of surgical oncology. 2011;18(3):629-35. doi:10.1245/s10434-010-1337-0.
Simunovic M, Urbach D, Major D, Sutradhar R, Baxter N, To T et al. Assessing the volume-outcome hypothesis and region-level quality improvement interventions: pancreas cancer surgery in two Canadian Provinces. Annals of surgical oncology. 2010;17(10):2537-44. doi:10.1245/s10434-010-1114-0.
Streiner DL, Norman GR. Correction for multiple testing: is there a resolution? Chest. 2011;140(1):16-8. doi:10.1378/chest.11-0523.
Mise Y, Vauthey JN, Zimmitti G, Parker NH, Conrad C, Aloia TA et al. Ninety-day Postoperative Mortality Is a Legitimate Measure of Hepatopancreatobiliary Surgical Quality. Annals of surgery. 2015;262(6):1071-8. doi:10.1097/SLA.0000000000001048.
Birkmeyer JD, Dimick JB. Potential benefits of the new Leapfrog standards: effect of process and outcomes measures. Surgery. 2004;135(6):569-75. doi:10.1016/j.surg.2004.03.004.
Greenblatt DY, Kelly KJ, Rajamanickam V, Wan Y, Hanson T, Rettammel R et al. Preoperative factors predict perioperative morbidity and mortality after pancreaticoduodenectomy. Annals of surgical oncology. 2011;18(8):2126-35.
Yoshioka R, Yasunaga H, Hasegawa K, Horiguchi H, Fushimi K, Aoki T et al. Impact of hospital volume on hospital mortality, length of stay and total costs after pancreaticoduodenectomy. British Journal of Surgery. 2014;101(5):523-9.
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I et al. Hospital volume and surgical mortality in the United States. New England Journal of Medicine. 2002;346(15):1128-37.
Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery. 1999;125(3):250-6.
Ansari D, Williamsson C, Tingstedt B, Andersson B, Lindell G, Andersson R. Pancreaticoduodenectomy—the transition from a low- to a high-volume center. Scandinavian journal of gastroenterology. 2014;49(4):481-4.
Swan RZ, Niemeyer DJ, Seshadri RM, Thompson KJ, Walters A, Martinie JB et al. The Impact of Regionalization of Pancreaticoduodenectomy for Pancreatic Cancer in North Carolina since 2004. The American Surgeon. 2014;80(6):561-6.
De Wilde R, Besselink M, van der Tweel I, de Hingh I, van Eijck C, Dejong C et al. Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. British Journal of Surgery. 2012;99(3):404-10.
Eppsteiner RW, Csikesz NG, McPhee JT, Tseng JF, Shah SA. Surgeon volume impacts hospital mortality for pancreatic resection. Annals of surgery. 2009;249(4):635-40.
Nathan H, Cameron JL, Choti MA, Schulick RD, Pawlik TM. The volume-outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. Journal of the American College of Surgeons. 2009;208(4):528-38. doi:10.1016/j.jamcollsurg.2009.01.007.
Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Archives of surgery. 2010;145(7):634-40. doi:10.1001/archsurg.2010.118.
Mamidanna R, Ni Z, Anderson O, Spiegelhalter SD, Bottle A, Aylin P et al. Surgeon Volume and Cancer Esophagectomy, Gastrectomy, and Pancreatectomy: A Population-based Study in England. Annals of surgery. 2016;263(4):727-32. doi:10.1097/SLA.0000000000001490.
Kanhere HA, Trochsler MI, Kanhere MH, Lord AN, Maddern GJ. Pancreaticoduodenectomy: outcomes in a low-volume, specialised Hepato Pancreato Biliary unit. World journal of surgery. 2014;38(6):1484-90. doi:10.1007/s00268-013-2431-9.
Sohn TA, Yeo CJ, Cameron JL, Geschwind JF, Mitchell SE, Venbrux AC et al. Pancreaticoduodenectomy: role of interventional radiologists in managing patients and complications. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2003;7(2):209-19.
Sanjay P, Kellner M, Tait IS. The role of interventional radiology in the management of surgical complications after pancreatoduodenectomy. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2012;14(12):812-7. doi:10.1111/j.1477-2574.2012.00545.x.
Baker TA, Aaron JM, Borge M, Pierce K, Shoup M, Aranha GV. Role of interventional radiology in the management of complications after pancreaticoduodenectomy. American journal of surgery. 2008;195(3):386-90; discussion 90. doi:10.1016/j.amjsurg.2007.12.026.
Amini N, Spolverato G, Kim Y, Pawlik TM. Trends in Hospital Volume and Failure to Rescue for Pancreatic Surgery. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2015;19(9):1581-92. doi:10.1007/s11605-015-2800-9.
Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Annals of surgery. 2009;250(6):1029-34.
Newhook TE, LaPar DJ, Lindberg JM, Bauer TW, Adams RB, Zaydfudim VM. Morbidity and mortality of pancreaticoduodenectomy for benign and premalignant pancreatic neoplasms. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2015;19(6):1072-7. doi:10.1007/s11605-015-2799-y.
Nordback L, Parviainen M, Raty S, Kuivanen H, Sand J. Resection of the head of the pancreas in Finland: effects of hospital and surgeon on short-term and long-term results. Scand J Gastroenterol. 2002;37(12):1454-60.
Pal N, Axisa B, Yusof S, Newcombe RG, Wemyss-Holden S, Rhodes M et al. Volume and outcome for major upper GI surgery in England. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2008;12(2):353-7. doi:10.1007/s11605-007-0288-7.
Castleberry AW, White RR, De La Fuente SG, Clary BM, Blazer DG, 3rd, McCann RL et al. The impact of vascular resection on early postoperative outcomes after pancreaticoduodenectomy: an analysis of the American College of Surgeons National Surgical Quality Improvement Program database. Annals of surgical oncology. 2012;19(13):4068-77. doi:10.1245/s10434-012-2585-y.
Riediger H, Makowiec F, Fischer E, Adam U, Hopt UT. Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2006;10(8):1106-15. doi:10.1016/j.gassur.2006.04.002.
Harris JW, Martin JT, Maynard EC, McGrath PC, Tzeng CW. Increased morbidity and mortality of a concomitant colectomy during a pancreaticoduodenectomy: an NSQIP propensity-score matched analysis. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2015;17(9):846-54. doi:10.1111/hpb.12471.
Temple SJ, Kim PT, Serrano PE, Kagedan D, Cleary SP, Moulton CA et al. Combined pancreaticoduodenectomy and colon resection for locally advanced peri-ampullary tumours: analysis of peri-operative morbidity and mortality. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2014;16(9):797-800. doi:10.1111/hpb.12263.
Acknowledgements
The authors declare no conflicts of interest. This study is funded by an Operating Grant from the Cancer Research Society and Rob Lutterman Memorial Fund, 2013–2015. The principal investigator (N.G.C.) is the Sherif and Mary Lou Hanna Chair in Surgical Oncology Research for salary and operating funds. All funding was used for collection, management, analysis, and interpretation of data. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. Nor endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed herein are those of the author and not necessarily those of CIHI. Parts of this material are based on data and information provided by Cancer Care Ontario (CCO). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of CCO. No endorsement by CCO is intended or should be inferred.
Author Contribution
D.J.K. made substantial contributions to the conception and design of the work, the acquisition, analysis, and interpretation of data for the work. N.G., Q.L., A.K., and C.C.E. made substantial contributions to the acquisition, analysis, and interpretation of data for the work. P.J.K., A.C.W., and N.M. made substantial contributions to the conception and design of the work. N.G.C. made substantial contributions to the conception and design of work, the acquisition, analysis, and interpretation of data for the work. All authors participated in drafting the work and revising it critically for important intellectual content, and final approval of the version to be published. All authors are in agreement to be accountable for all aspects of the work in ensuring that questions relating to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding Sources
This study is funded by an Operating Grant from the Cancer Research Society and Rob Lutterman Memorial Fund, 2013–2015. The principal investigator (N.G.C.) is the Sherif and Mary Lou Hanna Chair in Surgical Oncology Research for salary and operating funds. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Previous Presentation of Material
An abstract based on these results has been presented at the American College of Surgeons Clinical Congress, October 2016 in Washington DC as a poster. There are no accompanying submission or publication requirements.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOCX 20 kb)
Supplementary Table 2
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Kagedan, D.J., Goyert, N., Li, Q. et al. The Impact of Increasing Hospital Volume on 90-Day Postoperative Outcomes Following Pancreaticoduodenectomy. J Gastrointest Surg 21, 506–515 (2017). https://doi.org/10.1007/s11605-016-3346-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3346-1