Abstract
Background
Guidelines recommend limiting minimally invasive pancreaticoduodenectomy (MIPD) to high-volume centers. However, the definition of high-volume care remains unclear. We aimed to objectively define a minimum number of MIPD performed annually per hospital associated with improved outcomes in a contemporary patient cohort.
Patients and Methods
Resectable pancreatic adenocarcinoma patients undergoing MIPD were included from the National Cancer Database (2010–2017). Multivariable modeling with restricted cubic splines was employed to identify an MIPD annual hospital volume threshold associated with lower 90-day mortality. Outcomes were compared between patients treated at low-volume (≤ model-identified cutoff) and high-volume (> cutoff) centers.
Results
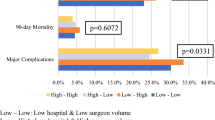
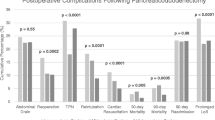
Among 3079 patients, 141 (5%) died within 90 days. Median hospital volume was 6 (range 1–73) cases/year. After adjustment, increasing hospital volume was associated with decreasing 90-day mortality for up to 19 (95% CI 16–25) cases/year, indicating a threshold of 20 cases/year. Most cases (82%) were done at low-volume (< 20 cases/year) centers. With adjustment, MIPD at low-volume centers was associated with increased 90-day mortality (OR 2.7; p = 0.002). Length of stay, positive surgical margins, 30-day readmission, and overall survival were similar. On analysis of the most recent two years (n = 1031), patients at low-volume centers (78.2%) were younger and had less advanced tumors but had longer length of stay (8 versus 7 days; p < 0.001) and increased 90-day mortality (7% versus 2%; p = 0.009).
Conclusions
The cutpoint analysis identified a threshold of at least 20 MIPD cases/year associated with lower postoperative mortality. This threshold should inform national guidelines and institution-level protocols aimed at facilitating the safe implementation of this complex procedure.

Similar content being viewed by others
Data Access, Responsibility, and Analysis
Statistical analysis was performed by Dr. Mohamed Adam. Dr. Adam had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Ohtani H, Tamamori Y, Noguchi K, et al. A meta-analysis of randomized controlled trials that compared laparoscopy-assisted and open distal gastrectomy for early gastric cancer. J Gastrointest Surg. 2010;14(6):958–64. https://doi.org/10.1007/s11605-010-1195-x.
Vanounou T, Steel JL, Nguyen KT, et al. Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol. 2010;17(4):998–1009. https://doi.org/10.1245/s10434-009-0839-0.
Anderson KL, Adam MA, Thomas S, Roman SA, Sosa JA. Impact of minimally invasive vs. open distal pancreatectomy on use of adjuvant chemoradiation for pancreatic adenocarcinoma. Am J Surg. 2017;213(4):601–5. https://doi.org/10.1016/j.amjsurg.2017.01.005.
Varley PR, Zenati MS, Klobuka A, et al. Does robotic pancreaticoduodenectomy improve outcomes in patients with high risk morphometric features compared to the open approach. HPB (Oxford). 2019;21(6):695–701. https://doi.org/10.1016/j.hpb.2018.10.016.
Baimas-George M, Watson M, Murphy KJ, et al. Robotic pancreaticoduodenectomy may offer improved oncologic outcomes over open surgery: a propensity-matched single-institution study. Surg Endosc. 2020;34(8):3644–9. https://doi.org/10.1007/s00464-020-07564-x.
Palanivelu C, Senthilnathan P, Sabnis SC, et al. Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg. 2017;104(11):1443–50. https://doi.org/10.1002/bjs.10662.
Poves I, Burdío F, Morató O, et al. Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP randomized controlled trial. Ann Surg. 2018;268(5):731–9. https://doi.org/10.1097/SLA.0000000000002893.
Adam MA, Choudhury K, Dinan MA, et al. Minimally invasive versus open pancreaticoduodenectomy for cancer: practice patterns and short-term outcomes among 7061 patients. Ann Surg. 2015;262(2):372–7. https://doi.org/10.1097/SLA.0000000000001055.
Sharpe SM, Talamonti MS, Wang CE, et al. Early national experience with laparoscopic pancreaticoduodenectomy for ductal adenocarcinoma: a comparison of laparoscopic pancreaticoduodenectomy and open pancreaticoduodenectomy from the National Cancer Data Base. J Am Coll Surg. 2015;221(1):175–84. https://doi.org/10.1016/j.jamcollsurg.2015.04.021.
van Hilst J, de Rooij T, Bosscha K, et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019;4(3):199–207. https://doi.org/10.1016/S2468-1253(19)30004-4.
Adam MA, Thomas S, Youngwirth L, Pappas T, Roman SA, Sosa JA. Defining a hospital volume threshold for minimally invasive pancreaticoduodenectomy in the United States. JAMA Surg. 2017;152(4):336–42. https://doi.org/10.1001/jamasurg.2016.4753.
Ahola R, Siiki A, Vasama K, Vornanen M, Sand J, Laukkarinen J. Effect of centralization on long-term survival after resection of pancreatic ductal adenocarcinoma. Br J Surg. 2017;104(11):1532–8. https://doi.org/10.1002/bjs.10560.
Asbun HJ, Moekotte AL, Vissers FL, et al. The Miami international evidence-based guidelines on minimally invasive pancreas resection. Ann Surg. 2020;271(1):1–14. https://doi.org/10.1097/SLA.0000000000003590.
Network NCC. Clinical practice guidelines in oncology: pancreatic adenocarcinoma (Version 1.2021). https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed 10 Feb 2021.
Speicher PJ, Nussbaum DP, White RR, et al. Defining the learning curve for team-based laparoscopic pancreaticoduodenectomy. Ann Surg Oncol. 2014;21(12):4014–9. https://doi.org/10.1245/s10434-014-3839-7.
Torphy RJ, Friedman C, Halpern A, et al. Comparing short-term and oncologic outcomes of minimally invasive versus open pancreaticoduodenectomy across low and high volume centers. Ann Surg. 2019;270(6):1147–55. https://doi.org/10.1097/SLA.0000000000002810.
About the National Cancer Database. https://www.facs.org/Quality-Programs/Cancer/NCDB/about. Accessed 22 Dec 2020.
Adam MA, Pura J, Goffredo P, et al. Presence and number of lymph node metastases are associated with compromised survival for patients younger than age 45 years with papillary thyroid cancer. J Clin Oncol. 2015;33(21):2370–5. https://doi.org/10.1200/JCO.2014.59.8391.
Croome KP, Farnell MB, Que FG, et al. Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg. 2014;260(4):633–8. https://doi.org/10.1097/SLA.0000000000000937 (discussion 638–640).
Wang M, Li D, Chen R, et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 2021. https://doi.org/10.1016/S2468-1253(21)00054-6.
Wang M, Peng B, Liu J, et al. Practice patterns and perioperative outcomes of laparoscopic pancreaticoduodenectomy in China: a retrospective multicenter analysis of 1029 patients. Ann Surg. 2021;273(1):145–53. https://doi.org/10.1097/SLA.0000000000003190.
Adam MA, Thomas S, Youngwirth L, et al. Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes? Ann Surg. 2017;265(2):402–7. https://doi.org/10.1097/SLA.0000000000001688.
Hachey K, Morgan R, Rosen A, et al. Quality comes with the (anatomic) territory: evaluating the impact of surgeon operative mix on patient outcomes after pancreaticoduodenectomy. Ann Surg Oncol. 2018;25(13):3795–803. https://doi.org/10.1245/s10434-018-6732-y.
Liao CH, Wu YT, Liu YY, et al. Systemic review of the feasibility and advantage of minimally invasive pancreaticoduodenectomy. World J Surg. 2016;40(5):1218–25. https://doi.org/10.1007/s00268-016-3433-1.
Wood TW, Ross SB, Bowman TA, et al. High-volume hospitals with high-volume and low-volume surgeons: is there a “field effect” for pancreaticoduodenectomy? Am Surg. 2016;82(5):407–11.
Joseph B, Morton JM, Hernandez-Boussard T, Rubinfeld I, Faraj C, Velanovich V. Relationship between hospital volume, system clinical resources, and mortality in pancreatic resection. J Am Coll Surg. 2009;208(4):520–7. https://doi.org/10.1016/j.jamcollsurg.2009.01.019.
Moekotte AL, Rawashdeh A, Asbun HJ, et al. Safe implementation of minimally invasive pancreas resection: a systematic review. HPB (Oxford). 2020;22(5):637–48. https://doi.org/10.1016/j.hpb.2019.11.005.
Hogg ME, Besselink MG, Clavien PA, et al. Training in minimally invasive pancreatic resections: a paradigm shift away from “see one, do one, teach one.” HPB (Oxford). 2017;19(3):234–45. https://doi.org/10.1016/j.hpb.2017.01.016.
Tsamalaidze L, Stauffer JA. Pancreaticoduodenectomy: minimizing the learning curve. J Vis Surg. 2018;4:64. https://doi.org/10.21037/jovs.2018.03.07.
Funding
P.C.C. was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, UCSF-CTSI Grant Number TL1 TR001871. J.A.L. was supported by the National Cancer Institute, National Institutes of Health, Grant Number T32CA25107001, and S.M. was supported by the National Institutes of Health, Grant Number 5T32AI125222-05. These contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
PCC, MD: Conceptualization, data curation, writing—original draft, writing—review and editing, visualization, project administration. LC, BA, MPhil: Writing—original draft, writing—review and editing. JAL, MD, MPH: Writing—review and editing. SM, MD, MPH: Writing—review and editing. AK, MD, PhD: Conceptualization, writing—review and editing. KH, MD: Conceptualization, writing—review and editing. EN, MD, PhD: Conceptualization, writing—review and editing. CC, MD: Conceptualization, writing—review and editing. JAS, MD, MA: Writing—review and editing. AS, MD: Writing—review and editing. KSK, MD: Conceptualization, writing—review and editing. AA, MD, EdM: Conceptualization, writing—review and editing. MAA, MD: Conceptualization, methodology, software, validation, formal analysis, investigation, resources, writing—review and editing, supervision, project administration.
Corresponding author
Ethics declarations
Disclosures
J.A.S. is a member of the Data Monitoring Committee of the Medullary Thyroid Cancer Consortium Registry supported by GlaxoSmithKline, Novo Nordisk, Astra Zeneca, and Eli Lilly. She receives institutional research funding from Exelixis and Eli Lilly. All other authors declare no conflicts of interest. All other authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Conroy, P.C., Calthorpe, L., Lin, J.A. et al. Determining Hospital Volume Threshold for Safety of Minimally Invasive Pancreaticoduodenectomy: A Contemporary Cutpoint Analysis. Ann Surg Oncol 29, 1566–1574 (2022). https://doi.org/10.1245/s10434-021-10984-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10984-1