Abstract
Objectives
Non-neoplastic salivary gland diseases are rare in children. This paper aims to present the spectrum of encountered non-neoplastic salivary gland diseases at a tertiary center by describing the demographics, clinical characteristics, and outcomes in this patient population.
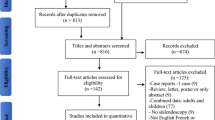
Methods
A review of electronic medical records was performed from 2010 until 2020. Relevant data were retrieved and charted according to the type of salivary gland disease. A comparison between diseases was made for demographics, presenting symptoms, treatment, and outcomes.
Results
Fifty patients with 11 different non-neoplastic salivary gland diseases were identified. Sialolithiasis was the most prevalent condition (12/50), with 83% localized in the submandibular gland. In contrast to gender, age, and symptoms, the location of pathology was significantly associated with the diagnosis (p < 0.001). In patients with sialolithiasis, a hybrid procedure (combined endoscopy and lithotomy) resulted in 100% resolution of symptoms. For (plunging) ranula, marsupialisation had a relative risk of recurrence of 9.6 compared to (partial) extirpation of the sublingual gland.
Conclusions
Children with salivary gland diseases present with overlap** symptoms, making clinical diagnosis challenging. The present study may aid physicians and specialists in diagnosing the most prevalent conditions in children. Although no gold standards exist for their treatment, hybrid procedures (sialolithiasis) and subglingual gland extirpation (ranula) showed superior results over alternatives.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gellrich D, Bichler M, Reichel CA et al (2020) Salivary gland disorders in children and adolescents: a 15-year experience. Int Arch Otorhinolaryngol 24:E31–E37. https://doi.org/10.1055/S-0039-1697993
Heinrich I, Zenk J (2014) Salivary gland diseases in children. GMS Curr Top Otorhinolaryngol Head Neck Surg 13:Doc06. https://doi.org/10.3205/CTO000109
Lustmann J, Regev E, Melamed Y (1990) Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg 19:135–138
Chung MK, Jeong H-S, Ko M-H, et al Pediatric sialolithiasis: what is different from adult sialolithiasis? https://doi.org/10.1016/j.ijporl.2007.01.019
Sigismung P, Zenk J, Koch M et al (2015) Nearly 3,000 salivary stones: some clinical and epidemiologic aspects. Laryngoscope 125:1879–1882. https://doi.org/10.1002/LARY.25377
Schwarz Y, Bezdjian A, Daniel SJ (2018) Sialendoscopy in treating pediatric salivary gland disorders: a systematic review. Eur Arch Otorhinolaryngol 275:347–356. https://doi.org/10.1007/s00405-017-4830-2
Faure F, Querin S, Dulguerov P, et al (2007) Pediatric salivary gland obstructive swelling: sialendoscopic approachhttps://doi.org/10.1097/MLG.0b013e318068657c
Van Cleemput T, Vanpoecke J, Coropciuc R, Politis C (2021) Sialendoscopy: a four-year single center experience. J Oral Maxillofac Surg 79:2285–2291. https://doi.org/10.1016/J.JOMS.2021.06.020
Schwartz N, Hazkani I, Goshen S (2015) Combined approach sialendoscopy for management of submandibular gland sialolithiasishttps://doi.org/10.1016/j.amjoto.2015.04.001
Choi M-G (2019) Case report of the management of the ranula. J Korean Assoc Oral Maxillofac Surg 45:357–363. https://doi.org/10.5125/JKAOMS.2019.45.6.357
Nahlieli O, Shacham R, Shlesinger M, Eliav E (2004) Juvenile recurrent parotitis: a new method of diagnosis and treatment. Pediatrics 114:9–12. https://doi.org/10.1542/PEDS.114.1.9
Maynard J (1965) Recurrent parotid enlargement. Br J Surg 52:784–789. https://doi.org/10.1002/BJS.1800521021
Hemenway W (1971) Chronic punctate parotitis. Laryngoscope 81:485–509. https://doi.org/10.1288/00005537-197104000-00001
Wittekindt C, Jungehülsing M, Fischbach R, Landwehr P (2000) Chronic recurrent parotitis in childhood in monozygotic twins. Magnetic resonance sialography. HNO 48:221–225. https://doi.org/10.1007/S001060050036
Reid L, Douglas F, Crow Y et al (1998) Autosomal dominant juvenile recurrent parotitis. J Med Genet 35:417–419. https://doi.org/10.1136/JMG.35.5.417
Ericson S, Zetterlund B, Ohman J (1991) Recurrent parotitis and sialectasis in childhood. Clinical, radiologic, immunologic, bacteriologic, and histologic study. Ann Otol Rhinol Laryngol 100:527–535. https://doi.org/10.1177/000348949110000702
Glasenapp GB, Schmidt W, Kessler L, Otto HJ (1970) Treatment of chronic recurrent parotitis by roentgen irradiation under scintigraphic control. Zeitschrift fur Laryngologie, Rhinologie, Otologie und ihre Grenzgebiete 49:520–525
Shacham R, Droma E, London D et al (2009) Long-term experience with endoscopic diagnosis and treatment of juvenile recurrent parotitis. J Oral Maxillofac Surg 67:162–167. https://doi.org/10.1016/J.JOMS.2008.09.027
Quenin S, Plouin-Gaudon I, Marchal F et al (2008) Juvenile recurrent parotitis: sialendoscopic approach. Arch Otolaryngol Head Neck Surg 134:715–719. https://doi.org/10.1001/ARCHOTOL.134.7.715
Capaccio P, Sigismund P, Luca N et al (2012) Modern management of juvenile recurrent parotitis. J Laryngol Otol 126:1254–1260. https://doi.org/10.1017/S0022215112002319
Hviid A, Rubin S, Mühlemann K (2008) Mumps. The Lancet 371:932–944. https://doi.org/10.1016/S0140-6736(08)60419-5
Author information
Authors and Affiliations
Contributions
JVB contributed to the study conception and design. Material preparation, data collection, and analysis were performed by JVB and KB. The first draft of the manuscript was written by JVB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was obtained from the Ethics Committee for Research from the University Hospitals (reference number S66048).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ver Berne, J., Brijs, K., Coropciuc, R. et al. Non-neoplastic salivary gland diseases in children: a 10-year review at a tertiary center. Oral Maxillofac Surg 27, 693–697 (2023). https://doi.org/10.1007/s10006-022-01103-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-022-01103-9