Abstract
Aim:
This study was conducted to test the selectivity of DC031050 on cardiac and neuronal potassium channels.
Methods:
Human ether-à-go-go related gene (hERG), KCNQ and Kv1.2 channels were expressed in CHO cells. The delayed rectifier potassium current (IK) was recorded from dissociated hippocampal pyramidal neurons of neonatal rats. Whole-cell voltage patch clamp was used to record the voltage-activated potassium currents. Drug-containing solution was delivered using a RSC-100 Rapid Solution Changer.
Results:
Both DC031050 and dofetilide potently inhibited hERG currents with IC50 values of 2.3±1.0 and 17.9±1.2 nmol/L, respectively. DC031050 inhibited the IK current with an IC50 value of 2.7±1.5 μmol/L, which was >1000 times the concentration required to inhibit hERG current. DC031050 at 3 μmol/L did not significantly affect the voltage-dependence of the steady activation, steady inactivation of IK, or the rate of IK from inactivation. Intracellular application of DC031050 (5 μmol/L) was insufficient to inhibit IK. DC031050 up to 10 μmol/L had no effects on KCNQ2 and Kv1.2 channel currents.
Conclusion:
DC031050 is a highly selective hERG potassium channel blocker with a substantial safety margin of activity over neuronal potassium channels, thus holds significant potential for therapeutic application as a class III antiarrhythmic agent.
Similar content being viewed by others
Introduction
Potassium channel blockers are categorised as class III antiarrhythmic agents due to their ability to prolong the duration of the cardiac action potential1, 2, 3, 4. These drugs include ibutilide, somatilide, sotalol, azimilide, droneradone and amiodarone, which elicit their actions by blocking one or more cardiac potassium channels, such as IKr, IKs and IKur, among others. The class III antiarrhythmic drugs have been subject to extensive clinical investigation as safer and more effective alternatives to class I drugs, which exhibit recognised risks in selected populations5, 6, 7. However, numerous noncardiac side effects, such as nausea, drizzles and headaches, also frequently occur with the use of class III antiarrhythmic drugs. Some adverse effects outside of cardiac tissues are consistent with the observation that the class III agents have been found to act on noncardiac ion channels. For example, tedisamil, a class III agent that is currently under evaluation in clinical trials, inhibits a calcium-dependent potassium (BK) channel of rat hippocampal CA1 neurons and guinea-pig portal vein smooth muscle cells. The inhibition of neuronal BK channels was thought to be related to nervous system toxicity associated with tedisamil8, 9. E4031, a potent IKr blocker, exhibits inhibitory effects on all transient, sustained and inwardly rectifying potassium currents of rat taste cells10. Therefore, the assessment of the effects elicited by class III agents on noncardiac channels is important for evaluating the safety and clinical side effects of these drugs at an early stage of the drug discovery process.
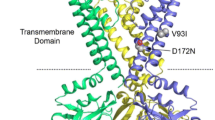
Dofetilide is a relatively new class III antiarrhythmic drug that has been approved for the conversion of atrial fibrillation and flutter and the maintenance of normal sinus rhythm. It selectively blocks the rapid delayed rectifier potassium channel (IKr), but does not slow the delayed rectifier potassium channel (IKs) IK1, sodium channels or calcium channels11, 12. To discover more effective class III antiarrhythmic agents, we have designed and synthesised a series of new methylsulfonamido phenylethylamine analogues based on the structure and pharmacophore of dofetilide13, 14. Biological assays using guinea pig atria indicated that all of the analogues exert significant class III activities, including the prolongation of action potential duration and of effective refractory duration. Of all of the analogues, DC031050 (N-Benzyl-N-[2-(p-methanesulfonamindo phenoxy)ethyl]-p-methanesulfonamido Phenethylamine) was identified as one of the most effective compounds. At the very low concentration of 16 nmol/L, DC031050 prolonged the effective refractory period for 10 ms. Furthermore, at a concentration of 10 μmol/L, DC031050 improved the force of constriction significantly more (24%) than dofetilide (17%)14. A comparison of the chemical structures of DC031050 and dofetilide revealed that the substitution of the methyl group with a benzyl group in DC0310590 improves its biological activity (Figure 1)14, representing a modification strategy of dofetilide to obtain more effective class III agents. Prior to further modification, we sought to further understand the durability of these dofetilide-like class III analogues by assessing whether they acted on noncardiac channels. Thus, we evaluated DC031050 for its effects on three types of voltage-gated neuronal potassium channels: KCNQ2, Kv1.2 and a delayed rectifier in hippocampal neurons. Our results showed that only the delayed rectifier channel was inhibited by DC031050, but at ∼1 000 times the concentration needed to block hERG.
Materials and methods
Compound synthesis
DC031050 was prepared according to previously reported procedures13, 14. The chemical structure of DC031050 is shown in Figure 1.
Preparation of dissociated hippocampal pyramidal neurons
Hippocampal neurons were dissociated from 5- to 9-day-old Sprague-Dawley rats as described previously. Briefly, mini-slices (500 μm) of the hippocampal CA1 region were cut in an ice-cold, oxygenated dissociation solution containing the following components (in mmol/L): Na2SO4 82, K2SO4 30, MgCl2 5, HEPES 10 and glucose 10 (pH 7.3). The slices were incubated in a dissociation solution containing protease XXIII (3 mg/mL) at 32 °C for 8 min. The solution was then replaced with dissociation solution containing trypsin inhibitor type II-S (1 mg/mL) and bovine serum albumin (1 mg/mL). The slices were allowed to cool to room temperature in an oxygenated solution. Before recording, the slices were triturated using a series of fire-polished Pasteur pipettes with progressively decreasing tip diameters. The dissociated neurons were placed into a recording dish and perfused with an external solution containing the following components (in mmol/L): NaCl 135, KCl 5, MgCl2 2, HEPES 10, glucose 10 and tetrodotoxin 0.001 (pH 7.3).
Cell culture and transfection
Chinese hamster ovary (CHO) cells were grown in 50/50 DMEM/F12 (Cellgro, Manassas, VA) supplemented with 10% fetal bovine serum (FBS) and 2 mmol/L L-glutamine (Gibco, Carlsbad, CA, USA). To overexpress the KCNQ and hERG channel proteins, the cells were split 24 h before transfection, plated into 60-mm dishes, and transfected with the appropriate plasmids using the Lipofectamine 2000™ reagent (Invitrogen, Carlsbad, CA, USA), according to the manufacturer's protocols. Twenty-four hours after transfection, the cells were split and re-plated onto coverslips coated with poly-L-lysine (Sigma-Aldrich, St Louis, MO, USA). A green fluorescent protein (GFP) expression plasmid (Amaxa, Gaithersburg, MD, USA) was cotransfected to allow for the identification of transfected cells by fluorescence microscopy.
Whole-cell voltage-clamp recording of hippocampal neurons and cultured CHO cells
The recordings were made at 21–23 °C using an Axopatch 200B amplifier (Molecular Devices, Sunnyvale, CA, USA). Electrodes with a tip resistance of 3–5 MΩ were pulled from borosilicate glass pipettes (World Precision Instruments, Sarasota, Fl) and filled with a pipette solution containing the following components (in mmol/L): KCl 140, MgCl2 1, CaCl2 1, HEPES 10 and EGTA 10 (pH 7.3). Voltage protocols were provided by pClamp 9.2 software via a DigiData-1322A interface (Molecular Devices, Sunnyvale, CA, USA). Series resistance was compensated by 75%–85%. For hippocampal neurons, the bath solution contained the following components (in mmol/L): NaCl 135, KCl 5, MgCl2 2, HEPES 10, glucose 10 and tetrodotoxin 0.001 (pH 7.3). The cells were maintained at −50 mV. The delayed rectifier current (IK) in hippocampal neurons was elicited by a series of 400-ms depolarising steps from −70 mV to +70 mV in 10 mV incremental steps following a 600-ms hyperpolarising pre-pulse to −110 mV and a 50-ms interval at −50 mV immediately after the pre-pulse to inactivate the transient component of the current. The resulting signals were sampled at frequencies of 10–40 kHz and filtered at 2–10 kHz. Linear leak and residual capacitance currents were subtracted on-line using a P/4 protocol. Unless otherwise stated, all IK amplitudes were obtained at 300 ms after the initiation of the stimulating pulse. The effect of DC031050 was assessed after the neurons were exposed to the drug for 40 s, and a minimum of 5-s interval was used between stimulations.
For cultured CHO cells, the pipette solution contained the following components (in mmol/L): KCl 145, MgCl2 1, EGTA 5, HEPES 10, and Mg-ATP 5 (pH=7.3 with KOH). The extracellular solution contained the following components (in mmol/L): NaCl 140, KCl 3, CaCl2 2, MgCl2 1.5, HEPES 10, and glucose 10 (pH=7.4 with NaOH).
Drug application
DC031050 was dissolved in dimethylsulfoxide (DMSO) to prepare a 10 mmol/L stock solution, from which the appropriate volumes were added to the external or pipette solutions to produce the desired concentrations. DMSO (less than 0.1% in the final dilution) elicited no observable effect on the K+ currents. For the electrophysiological recordings in neurons, the external solution containing DC031050 was delivered using a RSC-100 Rapid Solution Changer (BioLogic Co, France) that could change the external solution over the recorded neuron during a 10-ms period. For recordings in cultured CHO cells, a constant perfusion of extracellular solution was maintained using a BPS perfusion system (ALA scientific Instruments, Westburg, NY, USA). The DC031050 in the pipette solution was diffused into the neuron, and changes were recorded immediately after the rupture of the membrane patch. Unless otherwise stated, all chemicals were purchased from Sigma-Aldrich China Inc.
Data analysis
The concentration of DC031050 required to inhibit 50% of the K+ currents (IC50) was determined by fitting normalised data to the equation I/I0=1/{1+([C]/IC50)n}, where I0 and I are the current amplitudes measured in the absence and presence of the drug, respectively. [C] is the concentration of the drug in the external solution, and n is the Hill coefficient. For analysing the voltage-dependence of the steady-state activation or inactivation of the K+ currents, normalised conductance or current was plotted against the membrane potential and fitted to the Boltzmann equations as follows: Y=1/{1+exp[(V-V1/2)/k]}, where Y is the normalised conductance or current, V is the test potential, V1/2 is the voltage at half-maximal activation or inactivation, and k is the slope factor. The time course of recovery of the K+ currents from inactivation was fitted with a mono-exponential function as follows: I/Imax=A*{1(exp[(Δt/τ]}, where Imax is the maximal current amplitude, I is the current after a recovery period of Δt, τ the time constant, and A is the amplitude coefficient. Data are presented as mean±SEM. Statistical significance was assessed using Student's t-test, where P<0.05 was considered significant.
Results
Inhibition of hERG channel by DC031050
In our previous study, DC031050 exhibited typical class III agent activity in biological assays using guinea pig atria14. Given its structural similarity with dofetilide, we hypothesised that the biological activity of DC031050 was elicited by its inhibition of hERG channels. To test our hypothesis, hERG channel proteins were transiently expressed in CHO cells, and the resulting currents elicited by depolarisation step pulses followed by repolarisation to −50 mV were recorded. As shown in Figure 2A & B, hERG currents were completely inhibited by 10 μmol/L DC03105015. At 20 min after washout, the inhibitory effects were not reversed. Analysis of the concentration-response relationships revealed an IC50 value of 2.3±1.0 nmol/L. In contrast, the IC50 of dofetilide on hERG channels is 17.9±1.2 nmol/L (Figure 2D). The more potent inhibition of hERG channels by DC031050 compared to dofetilide is consistent with the potent biological activity of DC031050 observed in vivo13, 14.
Concentration-dependent inhibition on hERG channel by DC031050. (A) Representative traces of hERG response to a series of depolarizing steps from −60 to +60 mV with 10 mV increment, delivered every 10 s, in the absence (control, left) and presence of 10 μmol/L DC031050 (right). (B) Overlap of representative traces of hERG responses to a depolarization step to +50 mV in the absence and presence of 10 μmol/L DC031050. (C) The I–V plot of hERG (the tail after returning to −50 mV) in the absence (control, open circle) and presence of 10 μmol/L DC031050 (filled circle) (n=4). (D) Dose dependence of hERG channel inhibition on DC031050 and dofetilide (n=6).
Lack of effect of DC031050 on neuronal KCNQ2 and Kv1.2 channels expressed in CHO cells
KCNQ channels, also called Kv7 channels, include five members. KCNQ2 and KCNQ3 form heterotetramers in the neurons and mediate the M current, a potassium current could be inhibited by activation of muscarinic receptor. Inhibition of the M current by a mutation of KCNQ2 or KCNQ3 can result in various pathologies including benign familial neonatal convulsion, a form of neuronal hyperexcitibility13, 14.
However, similar to other class III antiarrhythmic agents, dofetilide exhibits general noncardiac side effects, including headache, dizziness, rash and some nervous system effects, such as paralysis, migraine and syncope30, 31. Although there is no direct evidence linking these side effects to the dysfunction of noncardiac ion channels, the functional disorders of noncardiac ion channels are known to cause these syndromes. For example, mutations of brain-specific P/Q type calcium channels were linked to familial hemiplegic migraines32, whereas the functional down-regulation of Kir2.6, an inwardly rectifying potassium channel, was linked to thyrotoxic hypokalemic periodic paralysis33. Consistent with its adverse effects in the nervous system, a low concentration (100 μmol/L) of dofetilide acted on ion channels in hippocampal neurons (eg, the voltage-independent block of a calcium-dependent potassium channel (BK))34. Notably, the plasma concentration of dofetilide exceeds 100 nmol/L when administered at 1 mg twice daily continuously for 24 h35.
DC031050 is a dofetilide analogue that more potently blocks hERG channels, with an excellent safety margin on neuronal potassium channels
In the current study, we confirmed that DC031050 is a potent and complete blocker of hERG, with an IC50 value of 2.3 nmol/L, which is significantly less than the IC50 of dofetilide on hERG channels (17.9 nmol/L). hERG channels are cardiac potassium channels that are known to significantly influence the duration of cardiac action potentials. Thus, the electrophysiological data on heterologously expressed hERG channels is consistent with the results obtained from biological assays using guinea pig atria13, 14. Surveying a number of noncardiac potassium channels revealed that DC031050 (at 10 μmol/L concentration) elicited negligible effects on KCNQ2 and Kv1.2 channels that were expressed in CHO cells, but was sufficient to block IK in rat hippocampal neurons. The IC50 of DC031050 on IK was 2.7 μmol/L, which is more than 1000-fold higher than that on hERG. Thus, DC031050 should provide a broad concentration range for the selective therapeutic blockade of hERG channels without affecting other noncardiac potassium channels. The high selectivity of DC031050 on hERG channels strongly supports its potential for therapeutic application as a class III antiarrhythmic agent. The inhibitory effects on neuronal IK at the micromolar concentrations argue for further early drug discovery stage evaluation of the effects of this compound on noncardiac channels to obtain safer class III antiarrythymia drugs. This is particularly important given that, in addition to IK, KCNQ2 and Kv1.2, there are many other types of potassium channels that are expressed in neuronal tissues. To fully discern the safety of DC031050, the effects of the drug on other noncardiac potassium channels should be further studied.
Inhibition of neuronal delayed rectifier potassium channel by DC031050
The inhibition of DC031050 on the delayed rectified potassium channels in rat hippocampal neurons is dose dependent and exhibits the following principal properties. (1) DC031050 markedly accelerated the decay of IK in a concentration-dependent manner, which is consistent with more potent inhibition of the steady state current than of the peak current. These data suggest that DC031050 might be an open-channel blocker, indicating that opening of the channel is a prerequisite to blocking. Alternatively, DC031050 might accelerate the inactivation of IK. (2) DC031050 does not alter the kinetic properties of IK. DC031050 elicited no significant effects on either the voltage-dependence of inactivation or the time course of recovery from inactivation, which precludes the notion that this drug might act through acceleration of channel inactivation.
Two experiments supported the notion that DC031050 might act at the extracellular face of IK channels. In contrast to the marked inhibition of IK elicited by the external perfusion of 5 μmol/L DC031050, the intracellular application of the same concentration of this drug elicited a negligible effect. Furthermore, the inhibition of DC031050 was diminished by co-treatment with 15 mmol/L TEA, which is known to block potassium channels from the extracellular face. This indicates that when a TEA molecule occupies the external TEA binding site, a steric hindrance effect might prevent DC031050 from interacting with the channel. Combined with the observed acceleration of decay and the lack of effects on kinetics, DC031050 appears to be an open channel blocker, which acts at an external binding site(s) on the outer mouth of the neuronal delayed rectifier potassium channel.
In summary, we have identified DC031050, an analogue of dofetilide, as a highly selective hERG potassium channel blocker with an excellent safety margin over neuronal potassium channels. DC031050 exhibits therapeutic potential as a class III antiarrhythmic agent. Our study strongly supports the evaluation of effects elicited by class III agents on noncardiac channels at early stages of the drug discovery process.
Author contribution
Zhao-bing GAO, Hong LIU, and Hua-liang JIANG designed research; ** LI, Hai-feng SUN and **-zheng ZHOU performed research; all authors analyzed data; ** LI, Hai-feng SUN, Hong LIU, Zhao-bing GAO, and Guo-yuan HU wrote the paper.
References
Lazzara R . From first class to third class: recent upheaval in antiarrhythmic therapy — lessons from clinical trials. Am J Cardiol 1996; 78: 28–33.
Phillips GB, Morgan TK Jr, Nickisch K, Lind JM, Gomez RP, Wohl RA, et al. Synthesis and cardiac electrophysiological activity of aryl-substituted derivatives of the class III antiarrhythmic agent sematilide. Potential class I/III agents. J Med Chem 1990; 33: 627–33.
Selnick HG, Liverton NJ, Baldwin JJ, Butcher JW, Claremon DA, Elliott JM, et al. Class III antiarrhythmic activity in vivo by selective blockade of the slowly activating cardiac delayed rectifier potassium current IKs by (R)-2-(2,4-trifluoromethyl)-N-[2-oxo-5-phenyl-1-(2,2,2-trifluoroethyl)- 2,3-dihydro-1H-benzo[e][1,4]diazepin-3-yl]acetamide. J Med Chem 1997; 40: 3865–8.
Sahar DI, Reiffel JA, Bigger JT Jr, Squatrito A, Kidwell GA . Efficacy, safety, and tolerance of d-sotalol in patients with refractory supraventricular tachyarrhythmias. Am Heart J 1989; 117: 562–8.
Vaughan Williams EM . A classification of antiarrhythmic actions reassessed after a decade of new drugs. J Clin Pharmacol 1984; 24: 129–47.
Colastsky TJ . Ahtiarrhythmic drugs: where are we going? Technical review. Pharm News 1995; 2: 17–23.
MacNeil DJ . The side effect profile of class III antiarrhythmic drugs: focus on d,l-sotalol. Am J Cardiol 1997; 80: 90G–98G.
Pfrunder D, Kreye VA . Tedisamil blocks single large-conductance Ca2+-activated K+ channels in membrane patches from smooth muscle cells of the guinea-pig portal vein. Pflugers Arch 1991; 418: 308–12.
Church J, McLarnon JG . Tedisamil blocks BK-type Ca2+-dependent K+ channels and modulates action potentials in rat hippocampal neurons. Neurosci Lett 2002; 319: 79–82.
Sun XD, Herness MS . Inhibition of potassium currents by the antiarrhythmic drug E4031 in rat taste receptor cells. Neurosci Lett 1996; 204: 149–52.
Lenz TL, Hilleman DE . Dofetilide, a new class III antiarrhythmic agent. Pharmacotherapy 2000; 20: 776–86.
Lenz TL, Hilleman DE . Dofetilide: a new antiarrhythmic agent approved for conversion and/or maintenance of atrial fibrillation/atrial flutter. Drugs Today (Barc) 2000; 36: 759–71.
Liu H, Ji M, Jiang H, Liu L, Hua W, Chen K, et al. Computer-aided design, synthesis and biological assay of p-methylsulfonamido phenylethylamine analogues. Bioorg Med Chem Lett 2000; 10: 2153–7.
Liu H, Ji M, Luo X, Shen J, Huang X, Hua W, et al. New p-methylsulfonamido phenylethylamine analogues as class III antiarrhythmic agents: design, synthesis, biological assay, and 3D-QSAR analysis. J Med Chem 2002; 45: 2953–69.
Kiehn J, Lacerda AE, Wible B, Brown AM . Molecular physiology and pharmacology of HERG. Single-channel currents and block by dofetilide. Circulation 1996; 94: 2572–9.
**ong Q, Gao Z, Wang W, Li M . Activation of Kv7 (KCNQ) voltage-gated potassium channels by synthetic compounds. Trends Pharmacol Sci 2008; 29: 99–107.
Shapiro MS, Roche JP, Kaftan EJ, Cruzblanca H, Mackie K, Hille B . Reconstitution of muscarinic modulation of the KCNQ2/KCNQ3 K+ channels that underlie the neuronal M current. J Neurosci 2000; 20: 1710–21.
Wang HS, Pan Z, Shi W, Brown BS, Wymore RS, Cohen IS, et al. KCNQ2 and KCNQ3 potassium channel subunits: molecular correlates of the M-channel. Science 1998; 282: 1890–3.
Bagetta G, Nistico G, Dolly JO . Production of seizures and brain damage in rats by alpha-dendrotoxin, a selective K+ channel blocker. Neurosci Lett 1992; 139: 34–40.
Storm JF . Action potential repolarization and a fast after-hyperpolarization in rat hippocampal pyramidal cells. J Physiol 1987; 385: 733–59.
Guidoni L, Carloni P . Tetraethylammonium binding to the outer mouth of the KcsA potassium channel: implications for ion permeation. J Recept Signal Transduct Res 2002; 22: 315–31.
Heginbotham L, MacKinnon R . The aromatic binding site for tetraethylammonium ion on potassium channels. Neuron 1992; 8: 483–91.
Singh BN, Hauswirth O . Comparative mechanisms of action of antiarrhythmic drugs. Am Heart J 1974; 87: 367–82.
Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. The Cardiac Arrhythmia Suppression Trial II Investigators. N Engl J Med 1992; 327: 227–33.
Singh BN . The coming of age of the class III antiarrhythmic principle: retrospective and future trends. Am J Cardiol 1996; 78: 17–27.
Julian DG, Prescott RJ, Jackson FS, Szekely P . Controlled trial of sotalol for one year after myocardial infarction. Lancet 1982; 1: 1142–7.
Grimm W, Maisch B . Sudden cardiac death in dilated cardiomyopathy — therapeutic options. Herz 2002; 27: 750–9.
Frost L, Mortensen PE, Tingleff J, Platou ES, Christiansen EH, Christiansen N . Efficacy and safety of dofetilide, a new class III antiarrhythmic agent, in acute termination of atrial fibrillation or flutter after coronary artery bypass surgery. Dofetilide Post-CABG Study Group. Int J Cardiol 1997; 58: 135–40.
Pedersen OD, Bagger H, Keller N, Marchant B, Køber L, Torp-Pedersen C, et al. Efficacy of dofetilide in the treatment of atrial fibrillation-flutter in patients with reduced left ventricular function: a Danish investigations of arrhythmia and mortality on dofetilide (diamond) substudy. Circulation 2001; 104: 292–6.
Rasmussen HS, Allen MJ, Blackburn KJ, Butrous GS, Dalrymple HW . Dofetilide, a novel class III antiarrhythmic agent. J Cardiovasc Pharmacol 1992; 20 Suppl 2: S96–105.
Falk RH, Pollak A, Singh SN, Friedrich T . Intravenous dofetilide, a class III antiarrhythmic agent, for the termination of sustained atrial fibrillation or flutter. Intravenous Dofetilide Investigators. J Am Coll Cardiol 1997; 29: 385–90.
Terwindt GM, Ophoff RA, Haan J, Vergouwe MN, van Eijk R, Frants RR, et al. Variable clinical expression of mutations in the P/Q-type calcium channel gene in familial hemiplegic migraine. Dutch Migraine Genetics Research Group. Neurology 1998; 50: 1105–10.
Ryan DP, da Silva MR, Soong TW, Fontaine B, Donaldson MR, Kung AW, et al. Mutations in potassium channel Kir2.6 cause susceptibility to thyrotoxic hypokalemic periodic paralysis. Cell 2010; 140: 88–98.
McLarnon JG, Wang XP . Actions of cardiac drugs on a calcium-dependent potassium channel in hippocampal neurons. Mol Pharmacol 1991; 39: 540–6.
Walker DK, Alabaster CT, Congrave GS, Hargreaves MB, Hyland R, Jones BC, et al. Significance of metabolism in the disposition and action of the antidysrhythmic drug, dofetilide. In vitro studies and correlation with in vivo data. Drug Metab Dispos 1996; 24: 447–55.
Acknowledgements
We gratefully acknowledge Michael ** ZHU for his comments on this manuscript and the financial support from the National Natural Science Foundation of China (81072579, 20872153, and 81025017).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Li, P., Sun, Hf., Zhou, Pz. et al. Comparison of the effects of DC031050, a class III antiarrhythmic agent, on hERG channel and three neuronal potassium channels. Acta Pharmacol Sin 33, 728–736 (2012). https://doi.org/10.1038/aps.2012.41
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.41
- Springer Nature Singapore Pte Ltd.