Abstract
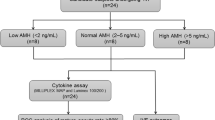
Polycystic ovary syndrome (PCOS) is a complex endocrine disorder syndrome with an incidence of 6% to 10% in women of reproductive age. Women with PCOS not only exhibit abnormal follicular development and fertility disorders, but also have a greater tendency to develop anxiety and depression. Our aim was to evaluate the ability of inflammatory factors in follicular fluid to predict embryonic developmental potential and pregnancy outcome and to construct a machine learning model that can predict IVF pregnancy outcomes based on indicators such as basic sex hormones, embryonic morphology, the follicular microenvironment, and negative emotion. In this study, inflammatory factors (CRP, IL-6, and TNF-α) in follicular fluid samples obtained from 225 PCOS and 225 non-PCOS women were detected via ELISA. For patients with PCOS, the levels of CRP and IL-6 in the follicular fluid in the pregnant group were significantly lower than those in the nonpregnant group. For non-patients with PCOS, only the level of IL-6 in the follicular fluid was significantly lower in the pregnant group than in the nonpregnant group. In addition, for both PCOS and non-patients with PCOS, compared with those in the pregnant group, patients in the nonpregnant group showed more pronounced signs of anxiety and depression. Finally, the factors that were significantly different between the two subgroups (pregnancy and nonpregnancy) of patients with or without PCOS were identified by an independent sample t test first and further analysed by multilayer perceptron (MLP) and random forest (RF) models to distinguish the two clinical pregnancy outcomes according to the classification function. The accuracy of the RF model in predicting pregnancy outcomes in patients with or without PCOS was 95.6% and 91.1%, respectively. The RF model is more suitable than the MLP model for predicting pregnancy outcomes in IVF patients. This study not only identified inflammatory factors that can affect embryonic development and assessed the anxiety and depression tendencies of PCOS patients, but also constructed an AI model that predict pregnancy outcomes through machine learning methods, which is a beneficial clinical tool.








Similar content being viewed by others
Data Availability
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Abbreviations
- AFC:
-
Antral follicle count
- AMH:
-
Anti-müllerian hormone
- AUC:
-
The average area under the curve
- BMI:
-
Body mass index
- CRP:
-
C reactive protein
- E2:
-
Estradiol
- FSH:
-
Follicle-stimulating hormone
- hCG:
-
Human chorionic gonadotropin
- HQ:
-
Blastocysts rate; high quality blastocysts rate
- IL-6:
-
Interleukin-6
- IVF:
-
In vitro fertilization
- LH:
-
Luteotrophic hormone
- ML:
-
Machine learning
- MLP:
-
Multilayer perceptron
- PCOS:
-
Polycystic ovary syndrome
- PCA:
-
Principal component analysis
- P:
-
Progesterone
- RF:
-
Random forest
- ROC:
-
Receiver operating characteristic
- SDS:
-
SAS, Self-rating anxiety Scale; Self-rating depression scale
- T:
-
Testosterone
- TNF-α:
-
Tumor necrosis factor-α
References
Norman RJ, Dewailly D, Legro RS, Hickey TE. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–97.
Orio F Jr, Palomba S, Cascella T, Di Biase S, Manguso F, Tauchmanova L, Nardo LG, Labella D, Savastano S, Russo T, et al. The increase of leukocytes as a new putative marker of low-grade chronic inflammation and early cardiovascular risk in polycystic ovary syndrome. J Clin Endocrinol Metab. 2005;90(1):2–5.
Sangeeta S. Metformin and pioglitazone in polycystic ovarian syndrome: a comparative study. J Obstet Gynaecol India. 2012;62(5):551–6.
Barlampa D, Bompoula MS, Bargiota A, Kalantaridou S, Mastorakos G, Valsamakis G. Hypothalamic inflammation as a potential pathophysiologic basis for the heterogeneity of clinical, hormonal, and metabolic presentation in PCOS. Nutrients. 2021;13(2):520.
Rudnicka E, Suchta K, Grymowicz M, Calik-Ksepka A, Smolarczyk K, Duszewska AM, Smolarczyk R, Meczekalski B. Chronic low grade inflammation in pathogenesis of PCOS. Int J Mol Sci. 2021;22(7):3789.
Shorakae S, Ranasinha S, Abell S, Lambert G, Lambert E, de Courten B, Teede H. Inter-related effects of insulin resistance, hyperandrogenism, sympathetic dysfunction and chronic inflammation in PCOS. Clin Endocrinol (Oxf). 2018;89(5):628–33.
Siddiqui S, Mateen S, Ahmad R, Moin S. A brief insight into the etiology, genetics, and immunology of polycystic ovarian syndrome (PCOS). J Assist Reprod Genet. 2022;39(11):2439–73.
Gao L, Gu Y, Yin X. High serum tumor necrosis factor-alpha levels in women with polycystic ovary syndrome: a meta-analysis. PLoS ONE. 2016;11(10):e0164021.
Kolhe JV, Chhipa AS, Butani S, Chavda V, Patel SS. PCOS and depression: common links and potential targets. Reprod Sci. 2022;29(11):3106–23.
**ng L, Xu J, Wei Y, Chen Y, Zhuang H, Tang W, Yu S, Zhang J, Yin G, Wang R, et al. Depression in polycystic ovary syndrome: focusing on pathogenesis and treatment. Front Psychiatry. 2022;13:1001484.
Fux Otta C, Fiol de Cuneo M, Szafryk de Mereshian P. Polycystic ovary syndrome: physiopathology review. Rev Fac Cien Med Univ Nac Cordoba. 2013;70(1):27–30.
Wood JR, Dumesic DA, Abbott DH, Strauss JF 3rd. Molecular abnormalities in oocytes from women with polycystic ovary syndrome revealed by microarray analysis. J Clin Endocrinol Metab. 2007;92(2):705–13.
Wood JR, Nelson VL, Ho C, Jansen E, Wang CY, Urbanek M, McAllister JM, Mosselman S, Strauss JF 3rd. The molecular phenotype of polycystic ovary syndrome (PCOS) theca cells and new candidate PCOS genes defined by microarray analysis. J Biol Chem. 2003;278(29):26380–90.
Bilbo SD, Klein SL. Special issue: the neuroendocrine-immune axis in health and disease. Horm Behav. 2012;62(3):187–190.
**ong YL, Liang XY, Yang X, Li Y, Wei LN. Low-grade chronic inflammation in the peripheral blood and ovaries of women with polycystic ovarian syndrome. Eur J Obstet Gynecol Reprod Biol. 2011;159(1):148–50.
Boulman N, Levy Y, Leiba R, Shachar S, Linn R, Zinder O, Blumenfeld Z. Increased C-reactive protein levels in the polycystic ovary syndrome: a marker of cardiovascular disease. J Clin Endocrinol Metab. 2004;89(5):2160–5.
Rudnicka E, Kunicki M, Suchta K, Machura P, Grymowicz M, Smolarczyk R. Inflammatory Markers in Women with Polycystic Ovary Syndrome. Biomed Res Int. 2020;2020:4092470.
Duffy DM, Ko C, Jo M, Brannstrom M, Curry TE. Ovulation: parallels with inflammatory processes. Endocr Rev. 2019;40(2):369–416.
Repaci A, Gambineri A, Pasquali R. The role of low-grade inflammation in the polycystic ovary syndrome. Mol Cell Endocrinol. 2011;335(1):30–41.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Human Reproduction. 2004;19(1):41–47.
Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry. 2017;17(1):329.
Lei M, Li C, **ao X, Qiu J, Dai Y, Zhang Q. Evaluation of the psychometric properties of the Chinese version of the resilience Scale in Wenchuan earthquake survivors. Compr Psychiatry. 2012;53(5):616–22.
Dunstan DA, Scott N. Clarification of the cut-off score for Zung’s self-rating depression scale. BMC Psychiatry. 2019;19(1):177.
Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20(1):90.
Feng Q, Zhang QL, Du Y, Ye YL, He QQ. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS ONE. 2014;9(6):e100914.
Peng B, Gong H, Tian H, Zhuang Q, Li J, Cheng K, Ming Y. The study of the association between immune monitoring and pneumonia in kidney transplant recipients through machine learning models. J Transl Med. 2020;18(1):370.
Matzuk MM, Burns KH, Viveiros MM, Eppig JJ. Intercellular communication in the mammalian ovary: oocytes carry the conversation. Science. 2002;296(5576):2178–80.
Adashi EY. The potential relevance of cytokines to ovarian physiology. J Steroid Biochem Mol Biol. 1992;43(5):439–44.
Adashi EY. The potential relevance of cytokines to ovarian physiology: the emerging role of resident ovarian cells of the white blood cell series. Endocr Rev. 1990;11(3):454–64.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Toulis KA, Goulis DG, Mintziori G, Kintiraki E, Eukarpidis E, Mouratoglou SA, Pavlaki A, Stergianos S, Poulasouchidou M, Tzellos TG, et al. Meta-analysis of cardiovascular disease risk markers in women with polycystic ovary syndrome. Hum Reprod Update. 2011;17(6):741–60.
Diamanti-Kandarakis E, Paterakis T, Alexandraki K, Piperi C, Aessopos A, Katsikis I, Katsilambros N, Kreatsas G, Panidis D. Indices of low-grade chronic inflammation in polycystic ovary syndrome and the beneficial effect of metformin. Hum Reprod. 2006;21(6):1426–31.
Xu X, Du C, Zheng Q, Peng L, Sun Y. Effect of metformin on serum interleukin-6 levels in polycystic ovary syndrome: a systematic review. BMC Womens Health. 2014;14:93.
Escobar-Morreale HF, Luque-Ramirez M, Gonzalez F: Circulating inflammatory markers in polycystic ovary syndrome: a systematic review and metaanalysis. Fertil Steril. 2011;95(3):1048–1058, e1041–1042.
Artimani T, Karimi J, Mehdizadeh M, Yavangi M, Khanlarzadeh E, Ghorbani M, Asadi S, Kheiripour N. Evaluation of pro-oxidant-antioxidant balance (PAB) and its association with inflammatory cytokines in polycystic ovary syndrome (PCOS). Gynecol Endocrinol. 2018;34(2):148–52.
Lai Y, Ye Z, Mu L, Zhang Y, Long X, Zhang C, Li R, Zhao Y, Qiao J. Elevated Levels of Follicular Fatty Acids Induce Ovarian Inflammation via ERK1/2 and Inflammasome Activation in PCOS. J Clin Endocrinol Metab. 2022;107(8):2307–17.
Gnawali A, Patel V, Cuello-Ramirez A, Al Kaabi AS, Noor A, Rashid MY, Henin S, Mostafa JA. Why are women with polycystic ovary syndrome at increased risk of depression? Exploring the etiological maze. Cureus. 2021;13(2):e13489.
Sadeeqa S, Mustafa T, Latif S. Polycystic ovarian syndrome-related depression in adolescent girls: a review. J Pharm Bioallied Sci. 2018;10(2):55–9.
Karjula S, Morin-Papunen L, Franks S, Auvinen J, Jarvelin MR, Tapanainen JS, Jokelainen J, Miettunen J, Piltonen TT. Population-based Data at Ages 31 and 46 Show Decreased HRQoL and Life Satisfaction in Women with PCOS Symptoms. J Clin Endocrinol Metab. 2020;105(6):1814–26.
Cesta CE, Viktorin A, Olsson H, Johansson V, Sjölander A, Bergh C, Skalkidou A, Nygren KG, Cnattingius S, Iliadou AN. Depression, anxiety, and antidepressant treatment in women: association with in vitro fertilization outcome. Fertil Steril. 2016;105(6):1594–1602.e3.
Peng M, Wen M, Jiang T, Jiang Y, Lv H, Chen T, Ling X, Li H, Meng Q, Huang B, et al. Stress, anxiety, and depression in infertile couples are not associated with a first IVF or ICSI treatment outcome. BMC Pregnancy Childbirth. 2021;21(1):725.
Sn S. Prediction of breast cancer through random forest. Curr Med Imaging. 2023;19(10):1144–55.
Ma J, Yin H, Hao X, Sha W, Cui H. Development of a random forest model to classify sarcoidosis and tuberculosis. Am J Transl Res. 2021;13(6):6166–74.
Blank C, Wildeboer RR, DeCroo I, Tilleman K, Weyers B, de Sutter P, Mischi M, Schoot BC. Prediction of implantation after blastocyst transfer in in vitro fertilization: a machine-learning perspective. Fertil Steril. 2019;111(2):318–26.
Huang X, Hong L, Wu Y, Chen M, Kong P, Ruan J, Teng X, Wei Z. Raman spectrum of follicular fluid: a potential biomarker for oocyte developmental competence in polycystic ovary syndrome. Front Cell Dev Biol. 2021;9:777224.
Acknowledgements
We thank Dr. Jun Zhang from Basecare Medical Device Co. for his guidance in building machine learning models.
Funding
This work was supported by grants from Natural Science Foundation of Shanghai Municipal Science and Technology Commission (General Project) (23ZR1450200).
Author information
Authors and Affiliations
Contributions
**n Huang and Zhe Yin drafted the manuscript, completed the experiments and performed statistical analysis. **n Huang and Yanqiu Wang designed the experiment and revised the article. Junting Xu collected follicular fluid samples and completed testing for inflammatory factors. Zhe Yin completed the patients’ anxiety and depression score survey and the construction of machine learning models. **n Huang and Yanqiu Wang confirm the authenticity of all the raw data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by Institutional Ethical Review Board of Shanghai Tongji Hospital (Reference: K-W-2019–007). The patients/participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, X., Yin, Z., Xu, J. et al. The Inflammatory State of Follicular Fluid Combined with Negative Emotion Indicators can Predict Pregnancy Outcomes in Patients with PCOS. Reprod. Sci. (2024). https://doi.org/10.1007/s43032-024-01538-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43032-024-01538-3