Abstract
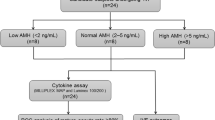
Ovarian reserve is an important determinant of a woman’s reproductive potential, and women with diminished ovarian reserve (DOR) often seek in vitro fertilization (IVF). The underlying etiology of DOR is unknown, but follicular fluid cytokine concentrations likely play a role in follicular development and maturation. The present study seeks to investigate the expression of cytokines in follicular fluid (FF) of women with DOR undergoing IVF and explore correlated functional pathways. One hundred ninety-four women undergoing ovarian stimulation were recruited at the time of oocyte retrieval. Women were classified as having DOR if they met one or more of the following criteria: AMH < 1 ng/ml, FSH > 10 mIU/ml, and/or AFC < 10. Controls included women undergoing IVF for male factor, tubal factor due to tubal ligation, or planned oocyte cryopreservation (non-oncologic). The concentrations of 480 cytokines and related growth factors in follicular fluid were determined using a multiplex immunoassay. Fifty-nine cytokines had significantly different concentrations (53 higher and 6 lower) in the DOR relative to the control group after adjusting for age and body mass index (BMI) (false discovery rate; FDR < 0.1). Using the most informative 44 biomarkers as indicated by a random forest (RF) model, an area under the curve (AUC) of 0.78 was obtained. Thus, follicular microenvironment differs between women with DOR and normal ovarian reserve. The differentially expressed cytokines belong to diverse processes that are primarily involved in follicular maturation and ovulation. These changes may play an important role in treatment outcomes in women with DOR.


Similar content being viewed by others
Data Availability
Data is available from the authors upon reasonable request.
Code Availability
Data is available from the authors upon reasonable request.
References
Sunderam S, Kissin DM, Zhang Y, Folger SG, Boulet SL, Warner L, et al. Assisted Reproductive Technology Surveillance - United States, 2016. MMWR Surveill Summ. 2019;68(4):1–23. https://doi.org/10.15585/mmwr.ss6804a1.
Broekmans FJ, Soules MR, Fauser BC. Ovarian aging: mechanisms and clinical consequences. Endocr Rev. 2009;30(5):465–93. https://doi.org/10.1210/er.2009-0006.
Practice Committee of the American Society for Reproductive M. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril. 2015;103(3):e9–17. https://doi.org/10.1016/j.fertnstert.2014.12.093.
Pastore LM, Christianson MS, Stelling J, Kearns WG, Segars JH. Reproductive ovarian testing and the alphabet soup of diagnoses: DOR, POI, POF, POR, and FOR. J Assist Reprod Genet. 2018;35(1):17–23. https://doi.org/10.1007/s10815-017-1058-4.
Baker VL, Gracia C, Glassner MJ, Schnell VL, Doody K, Coddington CC, et al. Multicenter evaluation of the Access AMH antimullerian hormone assay for the prediction of antral follicle count and poor ovarian response to controlled ovarian stimulation. Fertil Steril. 2018;110(3):506-13.e3. https://doi.org/10.1016/j.fertnstert.2018.03.031.
Hamdine O, Eijkemans MJ, Lentjes EW, Torrance HL, Macklon NS, Fauser BC, et al. Ovarian response prediction in GnRH antagonist treatment for IVF using anti-Mullerian hormone. Hum Reprod. 2015;30(1):170–8. https://doi.org/10.1093/humrep/deu266.
Steiner AZ, Pritchard D, Stanczyk FZ, Kesner JS, Meadows JW, Herring AH, et al. Association between biomarkers of ovarian reserve and infertility among older women of reproductive age. JAMA. 2017;318(14):1367–76. https://doi.org/10.1001/jama.2017.14588.
Richardson MC, Guo M, Fauser BC, Macklon NS. Environmental and developmental origins of ovarian reserve. Hum Reprod Update. 2014;20(3):353–69. https://doi.org/10.1093/humupd/dmt057.
Morin SJ, Patounakis G, Juneau CR, Neal SA, Scott RT, Seli E. Diminished ovarian reserve and poor response to stimulation in patients <38 years old: a quantitative but not qualitative reduction in performance. Hum Reprod. 2018;33(8):1489–98. https://doi.org/10.1093/humrep/dey238.
Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483–91. https://doi.org/10.3109/13697137.2015.1020484.
Quinn MM, Cedars MI. Cardiovascular health and ovarian aging. Fertil Steril. 2018;110(5):790–3. https://doi.org/10.1016/j.fertnstert.2018.07.1152.
Bouet PE, Boueilh T, de la Barca JMC, Boucret L, Blanchard S, Ferre-L’Hotellier V, et al. The cytokine profile of follicular fluid changes during ovarian ageing. J Gynecol Obstet Hum Reprod. 2020;49(4):101704. https://doi.org/10.1016/j.jogoh.2020.101704.
Spanou S, Kalogiannis D, Zapanti E, Gazouli M, Sfontouris IA, Siristatidis C, et al. Interleukin 15 concentrations in follicular fluid and their effect on oocyte maturation in subfertile women undergoing intracytoplasmic sperm injection. J Assist Reprod Genet. 2018;35(6):1019–25. https://doi.org/10.1007/s10815-018-1170-0.
Bayasula, Iwase A, Kobayashi H, Goto M, Nakahara T, Nakamura T, et al. A proteomic analysis of human follicular fluid: comparison between fertilized oocytes and non-fertilized oocytes in the same patient. J Assist Reprod Genet. 2013;30(9):1231–8. https://doi.org/10.1007/s10815-013-0004-3.
Hammadeh ME, Braemert B, Baltes S, Georg T, Rosenbaum P, Schmidt W. Relationship between ovarian stimulation regimen and cytokine concentration in follicular fluid and their effect on fertilization and pregnancy outcome of patients undergoing ICSI program. Am J Reprod Immunol. 2000;43(1):12–20. https://doi.org/10.1111/j.8755-8920.2000.430103.x.
Revelli A, DellePiane L, Casano S, Molinari E, Massobrio M, Rinaudo P. Follicular fluid content and oocyte quality: from single biochemical markers to metabolomics. Reprod Biol Endocrinol. 2009;7:40. https://doi.org/10.1186/1477-7827-7-40.
Zhou Q, Mao YQ, Jiang WD, Chen YR, Huang RY, Zhou XB, et al. Development of IGF signaling antibody arrays for the identification of hepatocellular carcinoma biomarkers. PLoS ONE. 2012;7(10):e46851. https://doi.org/10.1371/journal.pone.0046851.
Abhari S, Hipp HS, Gerkowicz SA, Katler QS, McKenzie LJ, Weirong S, et al. Differences in follicular fluid cytokine profile in women with diminished ovarian reserve. Fertility and Sterility. 2020;114(3):e452.
Practice Committee of the American Society for Reproductive Medicine. Electronic address aao, Practice Committee of the American Society for Reproductive M (2020) Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril 114(6):1151–7. https://doi.org/10.1016/j.fertnstert.2020.09.134.
Agarwal R, Whang DH, Alvero AB, Visintin I, Lai Y, Segal EA, et al. Macrophage migration inhibitory factor expression in ovarian cancer. Am J Obstet Gynecol. 2007;196(4):348.e1-5. https://doi.org/10.1016/j.ajog.2006.12.030.
Kats R, Metz CN, Akoum A. Macrophage migration inhibitory factor is markedly expressed in active and early-stage endometriotic lesions. J Clin Endocrinol Metab. 2002;87(2):883–9. https://doi.org/10.1210/jcem.87.2.8260.
Leech M, Metz C, Hall P, Hutchinson P, Gianis K, Smith M, et al. Macrophage migration inhibitory factor in rheumatoid arthritis: evidence of proinflammatory function and regulation by glucocorticoids. Arthritis Rheum. 1999;42(8):1601–8. https://doi.org/10.1002/1529-0131(199908)42:8%3c1601::AID-ANR6%3e3.0.CO;2-B.
Chen L, Guo L, Tian J, He H, Marinova E, Zhang P, et al. Overexpression of CXC chemokine ligand 14 exacerbates collagen-induced arthritis. J Immunol. 2010;184(8):4455–9. https://doi.org/10.4049/jimmunol.0900525.
Padilla J, Jenkins NT, Lee S, Zhang H, Cui J, Zuidema MY, et al. Vascular transcriptional alterations produced by juvenile obesity in Ossabaw swine. Physiol Genomics. 2013;45(11):434–46. https://doi.org/10.1152/physiolgenomics.00038.2013.
Hsieh M, Zamah AM, Conti M. Epidermal growth factor-like growth factors in the follicular fluid: role in oocyte development and maturation. Semin Reprod Med. 2009;27(1):52–61. https://doi.org/10.1055/s-0028-1108010.
Inoue Y, Miyamoto S, Fukami T, Shirota K, Yotsumoto F, Kawarabayashi T. Amphiregulin is much more abundantly expressed than transforming growth factor-alpha and epidermal growth factor in human follicular fluid obtained from patients undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2009;91(4):1035–41. https://doi.org/10.1016/j.fertnstert.2008.01.014.
Zamah AM, Hsieh M, Chen J, Vigne JL, Rosen MP, Cedars MI, et al. Human oocyte maturation is dependent on LH-stimulated accumulation of the epidermal growth factor-like growth factor, amphiregulin. Hum Reprod. 2010;25(10):2569–78. https://doi.org/10.1093/humrep/deq212.
Salmassi A, Schmutzler AG, Huang L, Hedderich J, Jonat W, Mettler L. Detection of granulocyte colony-stimulating factor and its receptor in human follicular luteinized granulosa cells. Fertil Steril. 2004;81(Suppl 1):786–91. https://doi.org/10.1016/j.fertnstert.2003.09.039.
Zhang L, Xu WH, Fu XH, Huang QX, Guo XY, Zhang L, et al. Therapeutic role of granulocyte colony-stimulating factor (G-CSF) for infertile women under in vitro fertilization and embryo transfer (IVF-ET) treatment: a meta-analysis. Arch Gynecol Obstet. 2018;298(5):861–71. https://doi.org/10.1007/s00404-018-4892-4.
Noel L, Fransolet M, Jacobs N, Foidart JM, Nisolle M, Munaut C. A paracrine interaction between granulosa cells and leukocytes in the preovulatory follicle causes the increase in follicular G-CSF levels. J Assist Reprod Genet. 2020;37(2):405–16. https://doi.org/10.1007/s10815-020-01692-y.
Nivet AL, Leveille MC, Leader A, Sirard MA. Transcriptional characteristics of different sized follicles in relation to embryo transferability: potential role of hepatocyte growth factor signalling. Mol Hum Reprod. 2016;22(7):475–84. https://doi.org/10.1093/molehr/gaw029.
Kawano Y, Zeineh Hasan K, Fukuda J, Mine S, Miyakawa I. Production of vascular endothelial growth factor and angiogenic factor in human follicular fluid. Mol Cell Endocrinol. 2003;202(1–2):19–23. https://doi.org/10.1016/s0303-7207(03)00056-x.
Sahin N, Toylu A, Gulekli B, Dogan E, Kovali M, Atabey N. The levels of hepatocyte growth factor in serum and follicular fluid and the expression of c-Met in granulosa cells in patients with polycystic ovary syndrome. Fertil Steril. 2013;99(1):264-9.e3. https://doi.org/10.1016/j.fertnstert.2012.08.059.
Lum L, Beachy PA. The Hedgehog response network: sensors, switches, and routers. Science. 2004;304(5678):1755–9. https://doi.org/10.1126/science.1098020.
Wang Y, McMahon AP, Allen BL. Shifting paradigms in Hedgehog signaling. Curr Opin Cell Biol. 2007;19(2):159–65. https://doi.org/10.1016/j.ceb.2007.02.005.
Nguyen NT, Lin DP, Yen SY, Tseng JK, Chuang JF, Chen BY, et al. Sonic hedgehog promotes porcine oocyte maturation and early embryo development. Reprod Fertil Dev. 2009;21(6):805–15. https://doi.org/10.1071/RD08277.
Russell MC, Cowan RG, Harman RM, Walker AL, Quirk SM. The hedgehog signaling pathway in the mouse ovary. Biol Reprod. 2007;77(2):226–36. https://doi.org/10.1095/biolreprod.106.053629.
Spicer LJ, Sudo S, Aad PY, Wang LS, Chun SY, Ben-Shlomo I, et al. The hedgehog-patched signaling pathway and function in the mammalian ovary: a novel role for hedgehog proteins in stimulating proliferation and steroidogenesis of theca cells. Reproduction. 2009;138(2):329–39. https://doi.org/10.1530/REP-08-0317.
Brannstrom M, Mayrhofer G, Robertson SA. Localization of leukocyte subsets in the rat ovary during the periovulatory period. Biol Reprod. 1993;48(2):277–86. https://doi.org/10.1095/biolreprod48.2.277.
Kollmann Z, Schneider S, Fux M, Bersinger NA, von Wolff M. Gonadotrophin stimulation in IVF alters the immune cell profile in follicular fluid and the cytokine concentrations in follicular fluid and serum. Hum Reprod. 2017;32(4):820–31. https://doi.org/10.1093/humrep/dex005.
Ledee N, Lombroso R, Lombardelli L, Selva J, Dubanchet S, Chaouat G, et al. Cytokines and chemokines in follicular fluids and potential of the corresponding embryo: the role of granulocyte colony-stimulating factor. Hum Reprod. 2008;23(9):2001–9. https://doi.org/10.1093/humrep/den192.
Fahey TJ 3rd, Tracey KJ, Tekamp-Olson P, Cousens LS, Jones WG, Shires GT, et al. Macrophage inflammatory protein 1 modulates macrophage function. J Immunol. 1992;148(9):2764–9.
Requena A, Cruz M, Agudo D, Pacheco A, Garcia-Velasco JA. Type of gonadotropin during controlled ovarian stimulation affects the endocrine profile in follicular fluid and apoptosis rate in cumulus cells. Eur J Obstet Gynecol Reprod Biol. 2016;197:142–6. https://doi.org/10.1016/j.ejogrb.2015.12.018.
Acknowledgements
We wish to thank Dawayland Cobb and Laura Sheckter for their assistance with this project.
Funding
This study was supported by RayBiotech Life, Inc.’s Collaborative Research Grant, Guangzhou Innovation Leadership Team (CXLJTD-201602). Additional support was from the National Institutes of Health (UL1TR002378), and the Building Interdisciplinary Research Careers in Women’s Health Program (K12HD085850). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
RayBiotech manufactures the Quantibody® Human Cytokine Antibody Array Q440 and Quantibody Human Cytokine Antibody Array Q12. RPH is the founder and CEO of RayBiotech, JL, BP, HHY, YM, and HT are employees of RayBiotech.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abhari, S., Lu, J., Hipp, H.S. et al. A Case–Control Study of Follicular Fluid Cytokine Profiles in Women with Diminished Ovarian Reserve. Reprod. Sci. 29, 2515–2524 (2022). https://doi.org/10.1007/s43032-021-00757-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00757-2