Abstract
Background
Rapid diagnosis and proper management of intracerebral hemorrhage (ICH) play a crucial role in the outcome. Prediction of the outcome with a high degree of accuracy based on admission data including imaging information can potentially influence clinical decision-making practice.
Methods
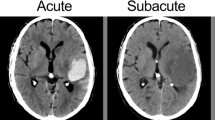
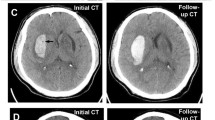
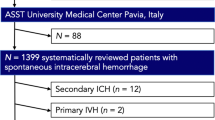
We conducted a retrospective multicenter study of consecutive ICH patients admitted between 2012–2017. Medical history, admission data, and initial head computed tomography (CT) scan were collected. CT scans were semiautomatically segmented for hematoma volume, hematoma density histograms, and sphericity index (SI). Discharge unfavorable outcomes were defined as death or severe disability (modified Rankin Scores 4–6). We compared (1) hematoma volume alone; (2) multiparameter imaging data including hematoma volume, location, density heterogeneity, SI, and midline shift; and (3) multiparameter imaging data with clinical information available on admission for ICH outcome prediction. Multivariate analysis and predictive modeling were used to determine the significance of hematoma characteristics on the outcome.
Results
We included 430 subjects in this analysis. Models using automated hematoma segmentation showed incremental predictive accuracies for in-hospital mortality using hematoma volume only: area under the curve (AUC): 0.85 [0.76–0.93], multiparameter imaging data (hematoma volume, location, CT density, SI, and midline shift): AUC: 0.91 [0.86–0.97], and multiparameter imaging data plus clinical information on admission (Glasgow Coma Scale (GCS) score and age): AUC: 0.94 [0.89–0.99]. Similarly, severe disability predictive accuracy varied from AUC: 0.84 [0.76–0.93] for volume-only model to AUC: 0.88 [0.80–0.95] for imaging data models and AUC: 0.92 [0.86–0.98] for imaging plus clinical predictors.
Conclusions
Multiparameter models combining imaging and admission clinical data show high accuracy for predicting discharge unfavorable outcome after ICH.


Similar content being viewed by others
References
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
Feigin VL. Stroke in develo** countries: can the epidemic be stopped and outcomes improved? Lancet Neurol. 2007;6:94–7.
Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53.
Moon JS, Janjua N, Ahmed S, Kirmani JF, Harris-Lane P, Jacob M, et al. Prehospital neurologic deterioration in patients with intracerebral hemorrhage. Crit Care Med. 2008;36:172–5.
Yang W-S, Li Q, Li R, Liu Q-J, Wang X-C, Zhao L-B, et al. Defining the optimal midline shift threshold to predict poor outcome in patients with supratentorial spontaneous intracerebral hemorrhage. Neurocrit Care. 2018;28:314–21.
Kiphuth IC, Huttner HB, Breuer L, Schwab S, Kohrmann M. Sonographic monitoring of midline shift predicts outcome after intracerebral hemorrhage. Cerebrovasc Dis. 2012;34:297–304.
Fogelholm R, Murros K, Rissanen A, Avikainen S. Admission blood glucose and short term survival in primary intracerebral haemorrhage: a population based study. J Neurol Neurosurg Psychiatry. 2005;76:349–53.
Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24:987–93.
Al-Shahi Salman R, Frantzias J, Lee RJ, Lyden PD, Battey TWK, Ayres AM, et al. Absolute risk and predictors of the growth of acute spontaneous intracerebral haemorrhage: a systematic review and meta-analysis of individual patient data. Lancet Neurol. 2018;17:885–94.
Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369:293–8.
Rodriguez-Luna D, Boyko M, Subramaniam S, Klourfeld E, Jo P, Diederichs BJ, et al. Magnitude of hematoma volume measurement error in intracerebral hemorrhage. Stroke. 2016;47:1124–6.
Divani AA, Majidi S, Luo X, Souslian FG, Zhang J, Abosch A, et al. The ABCs of accurate volumetric measurement of cerebral hematoma. Stroke. 2011;42:1569–74.
Webb AJ, Ullman NL, Morgan TC, Muschelli J, Kornbluth J, Awad IA, et al. Accuracy of the ABC/2 Score for Intracerebral Hemorrhage: systematic Review and Analysis of MISTIE, CLEAR-IVH, and CLEAR III. Stroke. 2015;46:2470–6.
Hussein HM, Tariq NA, Palesch YY, Qureshi AI. Reliability of hematoma volume measurement at local sites in a multicenter acute intracerebral hemorrhage clinical trial. Stroke. 2013;44:237–9.
Wang CW, Juan CJ, Liu YJ, Hsu HH, Liu HS, Chen CY, et al. Volume-dependent overestimation of spontaneous intracerebral hematoma volume by the ABC/2 formula. Acta Radiol. 2009;50:306–11.
Boulouis G, Morotti A, Brouwers H, et al. Association between hypodensities detected by computed tomography and hematoma expansion in patients with intracerebral hemorrhage. JAMA Neurol. 2016;73:961–8.
Barras CD, Tress BM, Christensen S, Collins M, Desmond PM, Skolnick BE, et al. Quantitative CT densitometry for predicting intracerebral hemorrhage growth. AJNR Am J Neuroradiol. 2013;34:1139–44.
Boulouis G, Morotti A, Brouwers HB, Charidimou A, Jessel MJ, Auriel E, et al. Noncontrast computed tomography hypodensities predict poor outcome in intracerebral hemorrhage patients. Stroke. 2016;47:2511–6.
Delcourt C, Zhang S, Arima H, Sato S, Al-Shahi Salman R, Wang X, et al. Significance of hematoma shape and density in intracerebral hemorrhage: the intensive blood pressure reduction in acute intracerebral hemorrhage trial study. Stroke. 2016;47:1227–32.
Zhang D, Chen J, Xue Q. Heterogeneity signs on noncontrast computed tomography predict hematoma expansion after intracerebral hemorrhage: a meta-analysis. Biomed Res. 2018;2018:6038193.
Hevesi M, Bershad EM, Jafari M, Mayer SA, Selim M, Suarez JI, et al. Untreated hypertension as predictor of in-hospital mortality in intracerebral hemorrhage: a multi-center study. J Crit Care. 2018;43:235–9.
Divani AA, Hevesi M, Pulivarthi S, Luo X, Souslian F, Suarez JI, et al. Predictors of nosocomial pneumonia in intracerebral hemorrhage patients: a multi-center observational study. Neurocrit Care. 2015;22:234–42.
Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32:891–7.
Poplawski NJ, Shirinifard A, Agero U, Gens JS, Swat M, Glazier JA. Front instabilities and invasiveness of simulated 3D avascular tumors. PLoS ONE. 2010;5:e10641.
Lee JH, Park CM, Park SJ, Bae JS, Lee SM, Goo JM. Value of computerized 3D shape analysis in differentiating encapsulated from invasive thymomas. PLoS ONE. 2015;10:e0126175.
Liao CC, Chen YF, **ao F. Brain midline shift measurement and its automation: a review of techniques and algorithms. Int J Biomed Imaging. 2018;2018:4303161.
Hummel M, Edelmann D, Kopp-Schneider A. Clustering of samples and variables with mixed-type data. PLoS ONE. 2017;12:e0188274.
Harrell FE. Regression modeling strategies with applications to linear models, logistic regression and survival analysis. Stat Med 2003;22:2531.
Kuhn M, Johnson K. Applied predictive modeling. New York: Springer; 2013.
Tian TS. Functional data analysis in brain imaging studies. Front Psychol. 2010;1:35.
Petersen A, Zhao J, Carmichael O, Muller HG. Quantifying individual brain connectivity with functional principal component analysis for networks. Brain Connect. 2016;6:540–7.
Ramsay JO, Silverman BW. Functional data analysis (springer series in statistics). 2nd ed. New York: Springer; 2005.
Petersen A, Muller H-G. Functional data analysis for density functions by transformation to a Hilbert space. Ann Stat. 2016;44:183–218.
Al-Mufti F, Thabet AM, Singh T, El-Ghanem M, Amuluru K, Gandhi CD. Clinical and radiographic predictors of intracerebral hemorrhage outcome. Interv Neurol. 2018;7:118–36.
Safatli DA, Gunther A, Schlattmann P, Schwarz F, Kalff R, Ewald C. Predictors of 30-day mortality in patients with spontaneous primary intracerebral hemorrhage. Surg Neurol Int. 2016;7:2152–7806.
Flemming KD, Wijdicks EF, Li H. Can we predict poor outcome at presentation in patients with lobar hemorrhage? Cerebrovasc Dis. 2001;11:183–9.
Nilsson OG, Lindgren A, Brandt L, Saveland H. Prediction of death in patients with primary intracerebral hemorrhage: a prospective study of a defined population. J Neurosurg. 2002;97:531–6.
Wang CW, Liu YJ, Lee YH, Hueng DY, Fan HC, Yang FC, et al. Hematoma shape, hematoma size, Glasgow coma scale score and ICH score: which predicts the 30-day mortality better for intracerebral hematoma? PLoS ONE. 2014;9:e102326.
Barras CD, Tress BM, Christensen S, MacGregor L, Collins M, Desmond PM, et al. Density and shape as CT predictors of intracerebral hemorrhage growth. Stroke. 2009;40:1325–31.
Nowinski WL, Gomolka RS, Qian G, Gupta V, Ullman NL, Hanley DF. Characterization of intraventricular and intracerebral hematomas in non-contrast CT. Neuroradiol J. 2014;27:299–315.
Hanley DF. Intraventricular hemorrhage and ICH outcomes: severity factor and treatment target. Stroke J Cereb Circ. 2009;40:1533–8.
Gregorio T, Pipa S, Cavaleiro P, Atanasio G, Albuquerque I, Chaves PC, et al. Prognostic models for intracerebral hemorrhage: systematic review and meta-analysis. BMC Med Res Methodol. 2018;18:145.
Bharath K, Kurtek S, Rao A, Baladandayuthapani V. Radiologic image-based statistical shape analysis of brain tumours. J R Stat Soc Ser C Appl Stat. 2018;67:1357–78.
Goldberg-Zimring D, Talos IF, Bhagwat JG, Haker SJ, Black PM, Zou KH. Statistical validation of brain tumor shape approximation via spherical harmonics for image-guided neurosurgery. Acad Radiol. 2005;12:459–66.
Crawford L, Monod A, Chen A, Mukherjee S, Rabadan R. Functional data analysis using a topological summary statistic: the smooth Euler characteristic transform. 2016. ar**v:161106818.
Author information
Authors and Affiliations
Contributions
PS designed and performed statistical analysis and contributed to manuscript preparation and subsequent revisions. MDN contributed to the study design, manuscript preparation, and subsequent revisions. MJ contributed to data collection and manuscript preparation. AJ contributed to data collection and manuscript preparation. WZ contributed to manuscript preparation. SAM contributed to manuscript preparation. AP contributed to statistical analysis design and manuscript preparation. EMB contributed to manuscript preparation. RD contributed to manuscript preparation. AAD designed the study, interpreted the results, prepared the manuscript the subsequent revisions, and supervised the project.
Corresponding author
Ethics declarations
Source of Support
No funding.
Conflict of interest
Dr. Salazar is an employee of Vital Images (Minnetonka, MN, USA).
Ethical Approval/Informed Consent
The Institutional Review Boards at Hennepin Healthcare System and Fairview Health Services in Minneapolis, Minnesota, approved the study. The data are reported based on the recommendations from STROBE (Strengthening The Reporting of OBservational Studies in Epidemiology). Informed consent is not required for this retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Salazar, P., Di Napoli, M., Jafari, M. et al. Exploration of Multiparameter Hematoma 3D Image Analysis for Predicting Outcome After Intracerebral Hemorrhage. Neurocrit Care 32, 539–549 (2020). https://doi.org/10.1007/s12028-019-00783-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00783-8