Abstract
Background
Nosocomial pneumonia (NP) is a frequent complication among spontaneous intracerebral hemorrhage (sICH) patients. This study was aimed at identifying in-hospital risk factors that predispose sICH patients to NP.
Methods
We identified 591 consecutive sICH subjects admitted to six tertiary care hospitals between 2008 and 2012. Information regarding patients’ demographics, admission data, laboratory tests, medical history, diagnostic imaging, in-hospital treatments, complications, and outcomes were collected. Using a competing risks analysis, we assessed risk factors associated with NP.
Results
Mean age of the subjects was 68 years; 51 % were female and 76 % were white. One-hundred sixteen (19.6 %) of the sICH patients had NP. In the univariate analysis, variables including age, non-white race, early hospital admission (<6 h after onset), larger hematoma volume, basal ganglia or intraventricular hemorrhage, multisite hemorrhage, in-hospital aspiration, intubation, nasogastric tube placement, hematoma evacuation, high ICH score, ventricular drainage, and tracheostomy had a positive association with NP. However, in the multivariate analysis, only early hospital admission, in-hospital aspiration, intubation, and tracheostomy remained statistically significant predictors (p < 0.05). For patients who survived hospitalization, the median length-of-stay (LOS) with or without NP was 20.0 and 4.0 days, respectively (p < 0.0001). For patients who did not survive to discharge, the median LOS with or without NP was 10.5 and 2.0 days, respectively (p < 0.001).
Conclusions
Independent predictors of NP included early hospital admission, in-hospital aspiration, intubation, and tracheostomy. NP was associated with prolonged hospital LOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
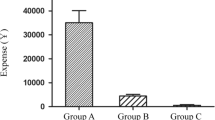
Pneumonia is a frequent complication of stroke and is associated with a threefold increase in mortality [1, 2]. Nosocomial pneumonia (NP) is associated with prolonged length-of-stay (LOS) and in-hospital death among intensive care unit (ICU) patients [3–6]. In a study of 18,017 stroke patients, the median LOS was 13 days for patients who developed NP, compared to 5 days for those without pneumonia [7]. The total direct hospital cost for all stroke subtypes patients with pneumonia is significantly higher than that for stroke patients without pneumonia [8]. Reported risk factors for pneumonia in stroke patients include multiple vascular territory distribution, vertebrobasilar stroke, high admission NIH Stroke Scale (NIHSS), dysphagia, tachypnea, and intubation [2, 4, 9].
There are few published studies focusing on risk factors for develo** NP in patients with spontaneous intracerebral hemorrhage (sICH). In one study, the presence of NP was reported as the highest (20 %) pulmonary complication in sICH patients [5] and was reported to increase LOS and mortality [10]. The lack of studies focusing on NP among sICH patients warrants further investigation to better ascertain risk factors specifically pertaining to this patient population. The present study may shed light on potential risk factors for earlier identification of patients who are predisposed to NP, which can then be validated in a further prospective study. The aim of this study was to assess the risk factors associated with NP and to determine the impact on LOS and in-hospital mortality among sICH patients.
Materials and Methods
We conducted a retrospective study of consecutive sICH patients admitted over 5 years (January 1, 2008 to December 31, 2012) to six tertiary care hospitals (Hennepin County Medical Center, Fairview Lakes Medical Center, Fairview Northland Medical Center, Fairview Ridges Hospital, Fairview Southdale Hospital, and University of Minnesota Medical Center, Fairview) in MN. Institutional Review Board approval was obtained through the Hennepin County Medical Center and Fairview Health Services prior to study initiation. We used International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) primary diagnosis codes 431, 432, and 432.9 to identify subjects with sICH. To reduce errors associated with coding misclassification, we also referenced our prospective database for stroke patients, which contained information regarding the presence of ICH. We also conducted a search through the databases available in the departments of Neurology and Neurosurgery to ensure we were not missing any patients due to possible errors in ICD-9 coding. These databases include demographic and clinical data related to inpatient stroke admissions, and are collected by stroke nurse coordinators in each department. We excluded patients with subarachnoid hemorrhage, subdural or epidural hemorrhage, hemorrhagic transformation of ischemic stroke, and traumatic ICH based on review of the chart documentations, and neuroimaging studies for each patient. The decision to exclude these cases was based on the following criteria: (1) Presence of hemorrhages in subarachnoid, subdural, or epidural space in conjunction with sICH is usually from other etiologies, mainly trauma. The same issue pertains to the presence of infarcted/ischemic tissue in a case of hemorrhagic transformation with or without thrombolysis. (2) The small number of such cases would not allow for a meaningful subgroup analysis. We also excluded subjects that were diagnosed with the presence of pneumonia upon admission (as was documented in the medical records by the treating physicians), since our focus was NP rather than community-acquired or aspiration pneumonia occurring outside the hospital. A standardized data collection form was used to gather demographic data, admission time, symptom onset, vital signs, laboratory tests, medical history, and imaging data. In-hospital treatments and complications with associated time were documented, as well as ICU, regular floor, and total hospital LOS. Neurological status was determined from NIHSS (when available), Glasgow Coma Scale (GCS), ICH score, and modified Rankin Scale (mRS) upon admission and discharge. Aspiration during hospital stay was defined as reflux of orogastric contents into the airway as documented in the chart by the healthcare personnel including nurses, respiratory therapists, or physicians.
Determination of NP
We identified cases of NP, among sICH subjects, by reviewing the charts for radiographic evidence of pulmonary consolidation and with the presence of two or more of the following: leukocytosis with white blood cell count ≥11,000 µl−1, fever greater than 38.5 °C, positive sputum culture, and crackles on pulmonary exam, tachypnea, or hypoxia. The same criteria have been used in other studies of neurological patients with pneumonia [5, 9].
Measurement of ICH Volume
We reviewed the initial and follow-up head CT scans to determine hematoma size and location (lobar, basal ganglia, thalamus, pons, cerebellum, and midbrain). We also recorded the presence of intraventricular hemorrhage (IVH) on each CT scan. The CT images were reconstructed at 2.5-mm thick transverse sections. Medical Image Processing, Analysis, and Visualization (MIPAV, National Institute of Health) was used to perform semi-automated computerized planimetry measurements [11]. The segmented boundary (area) of the hematoma observed in each CT slice was multiplied by the thickness of the slice to obtain the volume of each CT slice. The total volume was calculated as the sum of measured volumes for each CT slice [11].
Statistical Analysis
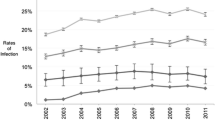
Baseline characteristics, including demographics, medical history, and hospitalization covariates were summarized for the NP and non-NP groups and compared using t test for continuous variables (Wilcoxon rank sum testing in the case of skewed variables) and χ 2 test for proportions. We used competing risk analysis as the primary analysis method, where non-NP mortalities were considered as a competing rather than a censoring event of NP, to assess the factors associated with NP in the presence of in-hospital mortality. Note that the usual survival analysis methods, such as the log-rank test and Cox regression, are not appropriate for competing risks data since these methods require the censoring event to be independent of the event of interest. In our case, NP and death were likely correlated. Specifically, we used cumulative incidence curves to estimate the risk of NP at different time points, Gray’s test [12] for comparing the risk of NP for different groups as a univariate analysis, and Fine and Gray proportional hazards regression [13] for multivariable analysis adjusting for covariates. We used Cox regression to study the effect of NP on patients’ survival at hospital discharge, where NP was treated as a time-dependent covariate. NP-free survival (i.e., disease-free survival) analysis was also conducted using Cox regression. Model checking was routinely performed for all regressions. Also, potential interactions between clinically relevant variables were tested for. We did not include the number of ventilator days in our multivariate regression model due to the fact that this was nested to intubation status. Therefore, we only chose intubation procedure and not ventilation length in our model.
All tests were two-sided. p values <0.05 were considered statistically significant. Competing risks analyses were conducted in R 3.0.2 (R Core Team). All other analyses were performed in SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
We reviewed 1,392 charts for the study. We excluded 780 cases because of a primary diagnosis (SDH, SAH, ICH due to trauma, arteriovenous fistula, arteriovenous malformation, hemorrhage due to dural venous sinus thrombosis, cavernomas, hemorrhagic transformation, hemorrhage due to brain tumor, etc.) other than sICH as was mentioned previously. After detailed review of the remaining 612 cases, we further excluded 21 cases that were diagnosed with pneumonia on admission. Therefore, we included 591 sICH patients in our study. Summaries of demographics, medical history, and clinical presentations related to the study subjects are shown in Table 1. We observed a 19.6 % (n = 116) occurrence rate of NP in our study population. Factors including age, race, time of symptom onset to hospital arrival, hematoma volume, ICH in basal ganglia, presence of IVH, multisite ICH, aspiration, intubation, nasogastric tube, hematoma evacuation, ICH score, ventricular drainage, and tracheostomy exhibited a statistically significant association with NP in univariate analysis (see Table 2). The following variables (not shown in Table 2) did not reveal any significant association with NP in the univariate analysis: gender, smoking status, history of hypertension, history of diabetes mellitus, history of heart failure (HF), chronic obstructive pulmonary disease, presence of hydrocephalus on initial CT, admission sodium and glucose levels, admission respiratory rate, admission blood pressure level, as well as admission mRS, NIHSS, and GCS scores.
The outcomes of the multivariable regression model are shown in Table 3. After adjusting for all the significant factors obtained from the univariate analysis (Gray’s test), subjects who arrived at the hospital more than 6 h after symptom onset had a lower hazard ratio (HR) of develo** NP 0.60 (95 % CI 0.40–0.91, p = 0.017). Subjects who experience in-hospital aspiration had a highest significant HR 3.03 (95 % CI 1.67–5.49, p = 0.0003) for NP. The HR of develo** NP for subjects who were intubated was 2.31 (95 % CI 1.19–4.49, p = 0.01) regardless of where the intubation procedure was performed (e.g., outside the hospital, in the emergency room, or in the neuro-ICU). Tracheostomy procedure significantly increased risk of NP (HR 2.37, 95 % CI 1.41–3.98, p = 0.001).
As a supplement to the analysis of NP, we conducted analysis of non-NP mortality—the competing risk of NP—for all the factors found significant on NP univariate analysis (see Tables 2, 4). In such a way, we hoped to see if the factors significant in determining NP were also related to non-NP mortality.
We found a lower cumulative incidence of NP, but at the same time significantly higher cumulative incidence of non-NP mortality among white subjects compared to nonwhites (HR 2.40, 95 % CI 1.31–4.39, p = 0.005). In addition, hematoma volumes larger than 60 ml (HR 4.88, 95 % CI 2.20–10.84, p = 0.0001) and intubation (HR 4.66, 95 % CI 2.25–9.68, p < 0.0001) increased the incidence of non-NP mortality. However, aspiration (HR 0.13, 95 % CI 0.03–0.68, p = 0.02), nasogastric tube usage (HR 0.45, 95 % CI 0.25–0.80, p = 0.007), hematoma evacuation (HR 0.37, 95 % CI 0.19–0.73, p = 0.004), and tracheostomy (HR 0.06, 95 % CI 0.01–0.30, p = 0.0006) were found to significantly decrease non-NP mortality risk.
We also found that those patients admitted to the hospital <6 h from symptom onset were not statistically different in terms of age, gender, and GCS score from those who were admitted ≥6 h after symptom onset. However, those admitted at <6 h had significantly higher NIHSS score (11.45 vs. 7.62, p < 0.0001) and admission mRS (4.08 vs. 3.86, p = 0.03) compared to those admitted after 6 h.
In association with NP, we analyzed the LOS among subjects discharged alive and those who died in hospital. The median LOS and interquartile range [IQR] for NP and non-NP subjects who were discharged alive were 20.0 [14.5–25.0] and 4.0 [2.0–8.0] days, respectively (p < 0.0001). For the subjects who died in hospital, median LOS [IQR] for NP versus non-NP subjects was 10.5 [5.3–14.5] and 2.0 [2.0–4.3] days, respectively (p < 0.001).
We also assessed the effect of NP on inpatient mortality, adjusting for the other potential risk factors including age, GCS, intubation, baseline NIHSS, hematoma volume, and IVH. The presence of NP was not found to be associated with in-hospital mortality, with or without adjusting for other factors.
Discussion
We present the largest study to date evaluating predictors of NP in ICH patients. The only other study we are aware of on this specific topic was published recently by Alsumrain et al. [14]. They found that mechanical ventilation, tube feeding, dysphagia, and tracheostomy were independently associated with NP. In our study cohort, we found that factors such as early hospital admission, in-hospital aspiration, intubation, and tracheostomy were independent predictors of NP.
Our analysis showed that the development of NP and mortality were associated with an earlier time of admission from symptom onset. We believe that the main factor which may account for this finding is that patients who admitted earlier suffered a more severe neurological deficit as determined by the NIHSS. These patients may have been identified and brought into the hospital more quickly. Another interesting observation was that the factors independently associated with decreased mortality in patients with non-NP mortality included hematoma evacuation and tracheostomy, whereas higher ICH score and intubation increased mortality. We believe that the latter indicates more severe ICH. The fact that surgical intervention was associated with lower mortality rates may indicate that the procedures performed may have been life-saving, or may have been a selection bias due to the choice to pursue more aggressive life sustaining measures, rather than withdrawal of support. Due to study limitations, we cannot determine whether patients underwent surgery had associated improved long-term outcomes. The association between tracheostomy and reduced mortality is not easily explained but may be due to censoring. We speculate that patients undergoing tracheostomies may have been discharged from the hospital to long-term acute care facilities and may have had further adverse outcomes outside the initial admitting institution. Whether tracheostomy decreases mortality will have to be determined in a prospective, controlled, randomized clinical trial.
We observed an overall rate of NP in our study population similar to another reported ICH study [5]. Some results obtained from the non-NP mortality analysis (as a supplementary to the analysis of NP) showed opposite directions on certain factors (e.g. race, aspiration, and tracheostomy) than those from the NP analysis. This may be explained by the fact that a higher rate of early death of a group of patients was usually associated with shorter LOS, hence less time for pneumonia to develop. Similarly, a lower rate of death would lead to a longer LOS and higher chance for develo** pneumonia.
We acknowledge the following additional limitations to our study. First, as the study is retrospective, we cannot rule out inherent methodological issues. The most important one was relying on written documentations to determine which patients had pneumonia. As a safety measure, we also referenced our prospective database for stroke patients, which contained information regarding the presence of ICH. Another limitation is that a standard scale such as the Clinical Pulmonary Infection Score (CPIS) was not used to define NP, but given the nature of this study, the individual components including degree of tracheal secretions and PaO2 to FiO2 ratios were not well documented or measured in all patients [15]. Furthermore, bronchoscopy or mini-BAL may be more accurate in diagnosing pneumonia; however, these procedures are not routinely done in the neuro-ICU due to the risks of elevating ICP. Additionally, we cannot be entirely sure that cases of aspiration pneumonitis were mistakenly identified as pneumonia, since the criteria we used to identify pneumonia can be positive for other reasons, such as fever from non-infectious etiology or leukocytosis from demargination, in the critically ill ICH patients. Nevertheless, these patients are usually empirically treated for pneumonia since one cannot be sure in clinical practice how to accurately differentiate these conditions. Both gram-positive (such as Staphylococcus aureus, Methicillin-resistant Staphylococcus aureus, Streptococcus pneumonia, and Micrococcus) and gram-negative organisms (such as Klebsiella pneumonia, Escherichia coli, Pseudomonas aeruginosa, and Haemophilus influenze) were reported for the patients diagnosed with NP. However, due to the presence missing data, we did not report any statistics on the type of microorganisms in culture-positive pneumonia patients. Furthermore, it is possible that some cases of pulmonary edema were misclassified as pneumonia, since the pulmonary edema may resemble consolidation on chest X-ray, or crackles may be heard in both conditions. Our definition of NP, however, also included findings which are not typical for pulmonary edema including fever, leukocytosis, and positive sputum culture. Therefore, it would not be expected that cases of pulmonary edema were misclassified as pneumonia.
It is also important to note that we have only presented outcome data upon hospital discharge. Outcomes such as long-term functional neurological outcome would be more useful at elucidating the effect of NP on long-term disability in sICH patients, but the retrospective design prohibited this analysis. Some other factors that we did not analyze include in-hospital HF or MI, since the reliability of these diagnoses in retrospective analysis is questionable, as ICH patients may have neurogenic pulmonary edema and having pneumonia may be difficult to differentiate from HF. Furthermore, ICH patients often have troponin elevation and/or EKG changes that may not indicate true MI, but cardiac strain and ICH patients are often unable to communicate clinical symptoms of chest pain due to neurological impairment.
Conclusions
We observed a high frequency of pneumonia among sICH patients, and identified symptom onset to arrival, aspiration, intubation, and tracheostomy as independent factors associated with NP. The impact of NP on morbidity and longer LOS highlights the importance of strict implementation of evidence-based VAP prevention bundles and aspiration precautions to reduce the incidence of NP [16–18]. There is a need to design large prospective studies to further assess and ascertain the risk factors that predispose sICH patients to develop NP. Once these risk factors are better elucidated, specific interventions can be instituted to reduce the frequency of NP and thus improve patient outcome.
References
Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60(4):620–5.
Walter U, Knoblich R, Steinhagen V, Donat M, Benecke R, Kloth A. Predictors of pneumonia in acute stroke patients admitted to a neurological intensive care unit. J Neurol. 2007;254(10):1323–9.
Bercault N, Boulain T. Mortality rate attributable to ventilator-associated nosocomial pneumonia in an adult intensive care unit: a prospective case-control study. Crit Care Med. 2001;29(12):2303–9.
Hilker R, Poetter C, Findeisen N, Sobesky J, Jacobs A, Neveling M, Heiss W-D. Nosocomial pneumonia after acute stroke: implications for neurological intensive care medicine. Stroke. 2003;34(4):975–81.
Maramattom BV, Weigand S, Reinalda M, Wijdicks EF, Manno EM. Pulmonary complications after intracerebral hemorrhage. Neurocrit Care. 2006;5(2):115–9.
Yilmaz GR, Cevik MA, Erdinc FS, Ucler S, Tulek N. The risk factors for infections acquired by cerebral hemorrhage and cerebral infarct patients in a neurology intensive care unit in Turkey. Jpn J Infect Dis. 2007;60(2–3):87–91.
Lakshminarayan K, Tsai AW, Tong X, Vazquez G, Peacock JM, George MG, Luepker RV, Anderson DC. Utility of dysphagia screening results in predicting poststroke pneumonia. Stroke. 2010;41(12):2849–54.
Katzan IL, Dawson NV, Thomas CL, Votruba ME, Cebul RD. The cost of pneumonia after acute stroke. Neurology. 2007;68(22):1938–43.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–63.
Saloheimo P, Lapp TM, Juvela S, Hillbom M. The impact of functional status at three months on long-term survival after spontaneous intracerebral hemorrhage. Stroke. 2006;37(2):487–91.
Divani AA, Majidi S, Luo X, Souslian FG, Zhang J, Abosch A, Tummala RP. The ABCs of accurate volumetric measurement of cerebral hematoma. Stroke. 2011;42(6):1569–74.
Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16(3):1141–54.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509.
Alsumrain M, Melillo N, Debari VA, Kirmani J, Moussavi M, Doraiswamy V, Katapally R, Korya D, Adelman M, Miller R. Predictors and Outcomes of Pneumonia in Patients With Spontaneous Intracerebral Hemorrhage. J Intensive Care Med. 2012;28:118–23.
Luyt CE, Chastre J, Fagon JY. Value of the clinical pulmonary infection score for the identification and management of ventilator-associated pneumonia. Intensive Care Med. 2004;30(5):844–52.
O’Keefe-McCarthy S, Santiago C, Lau G. Ventilator-associated pneumonia bundled strategies: an evidence-based practice. Worldviews Evid Based Nurs. 2008;5(4):193–204.
Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidelines for preventing health-care-associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR recommendations and reports: morbidity and mortality weekly report recommendations and reports/Centers for Disease Control. Respir care. 2004;53(3):1–36.
Tolentino-DelosReyes AF, Ruppert SD, Shiao SY. Evidence-based practice: use of the ventilator bundle to prevent ventilator-associated pneumonia. Am J Crit Care. 2007;16(1):20–7.
Acknowledgments
The authors express their gratitude to Katherine van Meurs, BA, Eduardo Paredes-Andrade, MD, and Derya Uludüz, MD, for their assistance in data collection. The study was supported in part by a generous donation from the family of Stanley S. Hubbard and HealthEZ (Bloomington, MN). Mario Hevesi, BS, was also supported by Nelson Heart Scholarship from the American Heart Association.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Divani, A.A., Hevesi, M., Pulivarthi, S. et al. Predictors of Nosocomial Pneumonia in Intracerebral Hemorrhage Patients: A Multi-center Observational Study. Neurocrit Care 22, 234–242 (2015). https://doi.org/10.1007/s12028-014-0065-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0065-x