Abstract
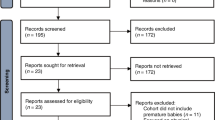
Artificial intelligence, including machine learning and deep learning, play an essential role in the medical industry for predicting various diseases. One such disease or disorder is a congenital disease that affects the newborn infant or unborn foetus by different viruses carried by the mother and passed on to the baby either during the time of pregnancy or delivery. Based on PRISMA guidelines, an extensive survey has been done to predict congenital diseases, including neonatal and postnatal. We have considered 115 articles related to the prediction of congenital diseases such as Zika virus, congenital heart disease, chromosome anomalies, sepsis, hypertension, cytomegalovirus, and many more using artificial intelligence published from 2008 to 2022 on different databases, journals, and conferences. In addition, the review also depicts the current work done by several researchers in the field of congenital disease prediction, along with their datasets and limitations. For complete work, we have designed four investigations and, in the end, explored solutions for the same. From the survey, it has been found that irrespective of various approaches used in the reported work, they can achieve predicted outcomes, but still, several problems need to be resolved. Thus, there is a need for more extensive research to deal with the challenges in the area of predicting various congenital diseases in the early stages.









Similar content being viewed by others
References
Waldorf KMA, McAdams RM (2013) Influence of infection during pregnancy on fetal development. Reproduction (Cambridge, England). https://doi.org/10.1530/REP-13-0232
McAuley JB (2011) Congenital toxoplasmosis. J Pediat Infect Dis Soc. https://doi.org/10.1093/jpids/piu077
Spitzer MH, Nolan GP (2016) Mass cytometry: single cells, many features. Cell 165:780–791. https://doi.org/10.1016/j.cell.2016.04.019
https://www.atsu.edu/faculty/chamberlain/Website/lectures/lecture/congen.htm
Tejera E, Areias MJ, Rodrigues A, Ramõa A, Nieto-Villar JM, Rebelo I (2011) Artificial neural network for normal, hypertensive, and preeclamptic pregnancy classification using maternal heart rate variability indexes. J Matern Fetal Neonatal Med. https://doi.org/10.3109/14767058.2010.545916
WHO fact sheet on congenital anomalies, updated September 2016, Available at www.who.int/mediacentre/factsheets/fs370/en/, Accessed 5 Oct 2018
Shahid N, Rappon T, Berta W (2019) Applications of artificial neural networks in health care organizational decision-making: a sco** review. PLoS ONE. https://doi.org/10.1371/journal.pone.0212356
Fatima M, Pasha M (2017) Survey of machine learning algorithms for disease diagnostic. J Intell Learn Syst Appl. https://doi.org/10.4236/jilsa.2017.91001
Workowski KA, Bachmann LH, Chan PA, Johnston CM, et al. (2021) Sexually Transmitted Infections Treatment Guidelines. MMWR Recommendation Report, 181–187
Workowski KA, Berman S (2010) Sexually transmitted diseases treatment guidelines. Morbidity and Mortality Weekly Report, 107–113
Liu W, Yu Z, Raj B, Yi L, Zou X, Li M (2015) Efficient autism spectrum disorder prediction with eye movement: a machine learning framework. Int Conf Affect Comput Intell Interact (ACII). https://doi.org/10.1109/ACII.2015.7344638
Marty FM, Ljungman P, Chemaly PF, Maertens J, Dadwal SS, Duarte RF, Haider S et al (2017) Letermovir prophylaxis for cytomegalovirus in hematopoietic-cell transplantation. N Engl J Med. https://doi.org/10.1056/NEJMoa1706640
Santis MD, Luca CD, Mappa I, Spagnuolo T et al (2012) Syphilis infection during pregnancy: fetal risks and clinical management. Infect Dis Obstert Gynecol. https://doi.org/10.1155/2012/430585
Wu X, Long E, Lin H, Liu Y (2016) Prevalence and epidemiological characteristics of con-genital cataract: a systematic review and meta-analysis. Sci Rep. https://doi.org/10.1038/srep28564
Veiga RV, Schuler-Faccini L, França GVA, Andrade RFS et al (2021) Classification algorithm for congenital Zika syndrome: characterizations, diagnosis and validation. Sci Rep. https://doi.org/10.1038/s41598-021-86361-5
Stevens GA, White RA, Flaxman SR, Price H, Jonas JB, Keeffe J, Leasher J et al (2013) Global prevalence of vision impairment and blindness: magnitude and temporal trends. Ophthalmology. https://doi.org/10.1016/j.ophtha.2013.05.025
Taruscio D, Mantovani A, Carbone P, Barisic I, Bianchi F et al (2015) Primary prevention of congenital anomalies: recommendable, feasible and achievable. Public Health Genom. https://doi.org/10.1159/000379739
Tejera E, Areias MJ, Rodrigues A, Ramoa A, Nieto-Villar JM, Rebelo I (2011) Artificial neural network for normal, hypertensive, and preeclamptic pregnancy classification using maternal heart rate variability indexes. J Matern Fetal Neonatal Med. https://doi.org/10.3109/14767058.2010.545916
Jung KH, Choi J, Gong EJ, Lee JH, Choi KD et al (2019) Can endoscopists diferentiate cytomegalovirus esophagitis from herpes simplex virus esophagitis based on gross endoscopic fndings? Medicine. https://doi.org/10.1097/MD.0000000000015845
Uchechi HO, Ifeyinwa OM, Asemota E, Okpokam D (2018) Seroprevalence of transfusion-transmissible infections (hbv, hcv, syphilis and hiv) among prospective blood donors in a tertiary health care facility in Calabar Nigeria; an eleven years evaluation. BMC Public Health. https://doi.org/10.1186/s12889-018-5555-x
Lawton B, MacDonald EJ, Brown SA, Wilson L, Stanley J, Tait JD (2014) Preventability of severe acute maternal morbidity. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2013.12.032
Huanga Y, Wanga H, Li T, Li C, Tanga J et al (2021) Comparison of detection strategies for screening and confirming congenital cytomegalovirus infection in newborns in a highly seroprevalent population: a mother-child cohort study. Lancet Region Health West Pacific. https://doi.org/10.1016/j.lanwpc.2021.100182
Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR (2016) Zika virus and birth defects-reviewing the evidence for causality. N Engl J Med. https://doi.org/10.1056/NEJMsr1604338
Adachi KN, Saines KN, Klausner JD (2021) Chlamydia trachomatis screening and treatment in pregnancy to reduce adverse pregnancy and neonatal outcomes: a review. Front Public Health. https://doi.org/10.3389/fpubh.2021.531073
Wallace J, Pitts M, Liu C, Lin V, Hajarizadeh B, Richmond J, Locarnini S (2017) More than a virus: a qualitative study of the social implications of hepatitis b infection in china. Int J Equity Health. https://doi.org/10.1186/s12939-017-0637-4
Oliveira D, W. K. et al. (2016) Increase in reported prevalence of microcephaly in infants born to women living in areas with confrmed Zika virus transmission during the frst trimester of pregnancy-Brazil. Morbidity and Mortality Weekly Report. https://doi.org/10.15585/mmwr.mm6509e2
Franca GVA, Faccini LS, Oliveira WK, Henriques CMP et al (2016) Congenital Zika virus syndrome in Brazil: a case series of the frst 1501 livebirths with complete investigation. Lancet. https://doi.org/10.1016/S0140-6736(16)30902-3
Aragao MDFV, Linden VVD, Brainer-Lima AM et al (2016) Clinical features and neuroimaging (CT and MRI) fndings in presumed Zika virus related congenital infection and microcephaly: retrospective case series study. BMJ Clin Res. https://doi.org/10.1136/bmj.i1901
Ciobanu A, Khan N, Syngelaki A, Akolekar R, Nicolaides KH (2019) Routine ultrasound at 32 vs 36 weeks’ gestation: prediction of small-for-gestational-age neonates. Ultrasound Obstet Gynecol. https://doi.org/10.1002/uog.20258
Gaccioli F, Aye ILMH, Sovio U, Charnock-Jones DS, Smith GCS (2018) Screening for fetal growth restriction using fetal biometry combined with maternal biomarkers. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2017.12.002
Bahado-Singh RO, Yilmaz A, Bisgin H, Turkoglu O, Kumar P et al (2019) Artificial intelligence and the analysis of multi-platform metabolomics data for the detection of intrauterine growth restriction. PLoS One. https://doi.org/10.1371/journal.pone.0214121
Masino AJ, Harris MC, Forsyth D, Ostapenko S, Srinivasan L et al (2019) “Machine learning models for early sepsis recognition in the neonatal intensive care unit using readily available electronic health record data. PLoS One. https://doi.org/10.1371/journal.pone.0212665
Song W, Jung S, Baek H, Choi C, Jung Y, Yoo S (2020) Development of prediction model for the early detection of late-onset neonatal sepsis using machine learning. JMIR Med Inform. https://doi.org/10.2196/15965
Quiros LC, Kommers D, Wolvers MK, Oosterwijk L, Arents N et al (2021) Prediction of late-onset sepsis in preterm infants using monitoring signals and machine learning. Crit Care Explor. https://doi.org/10.1097/CCE.0000000000000302
Kopanitsa G, Metsker O, Paskoshev D, Greschischeva S (2021) Identification of risk factors and prediction of sepsis in pregnancy using machine learning methods. Procedia Comput Sci. https://doi.org/10.1016/j.procs.2021.10.040
Hsu JF, Chang YF, Cheng HJ, Yang C, Lin CY, Chu SM et al (2021) Machine learning approaches to predict in-hospital mortality among neonates with clinically suspected sepsis in the neonatal intensive care unit. J Personal Medicien, MDPI. https://doi.org/10.3390/jpm11080695
Li H, Luo M, Zheng J, Luo J, Zeng R, Feng N, Du Q, Fang J (2017) An artificial neural network prediction model of congenital heart disease based on risk factors. Medicine. https://doi.org/10.1097/MD.0000000000006090
Yoon SA, Hong WH, Cho H (2020) Congenital heart disease diagnosed with echocardiogram in newborns with asymptomatic cardiac murmurs: a systematic review. BMC Pediator. https://doi.org/10.1186/s12887-020-02212-8
Du Y, Huang S, Huang C, Maalla A, Lia H (2020) Recognition of child congenital heart disease using electrocardiogram based on residual of residual network. IEEE Int Conf Progress Inform Comput (PIC). https://doi.org/10.1109/pic50277.2020.9350802
Meda JT, Mushiri T (2020) Predicting Congenital Heart Diseases Using Machine Learning. Proceedings of the 2nd African International Conference on Industrial Engineering and Operations Management, pp. 1716–1725.
Arnaout R, Curran L, Zhao Y, Levine JC, Chinn E, Moon-Grady AJ (2021) An ensemble of neural networks provides expert-level prenatal detection of complex congenital heart disease. Nat Med. https://doi.org/10.1038/s41591-021-01342-5
Nurmaini S, Rachmatullah MN, Sapitri AI, Darmawahyuni A et al (2021) Deep learning-based computer-aided fetal echocardiography: application to heart standard view segmentation for congenital heart defects detection. Artif Intell-Based Appl Med Imag. https://doi.org/10.3390/s21238007
Ammarah UE, Bukhari F, Idrees M, Iqbal W (2021) Predictive analysis of congenital heart defects prior to birth. Int Conf Robot Automat Ind (ICRAI). https://doi.org/10.1109/ICRAI54018.2021.9651436
Truong VT, Nguyen BP, Nguyen-Vo TH, Mazur W, Chung ES et al (2022) Application of machine learning in screening for congenital heart diseases using fetal echocardiography. Int J Cardiovasc Imaging 38:1007–1015
Qu Y, Deng X, Lin S, Han F, Chang HH, Ou Y, Nie Z et al (2022) Using innovative machine learning methods to screen and identify predictors of congenital heart diseases. Front Cardiovasc Med. https://doi.org/10.3389/fcvm.2021.797002
Say L, Chou D, Gemmill A, Tunçalp O, Moller AB, Daniels J et al (2014) Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. https://doi.org/10.1016/S2214-109X(14)70227-X
Abu-Raya B, Maertens K, Edwards KM, Omer SB, Englund JA, Flanagan KL (2020) Global perspectives on immunization during pregnancy and priorities for future research and development: an international consensus statement. Front Immunol. https://doi.org/10.3389/fimmu.2020.01282
Shameer K, Johnson KW, Glicksberg BS, Dudley JT, Sengupta PP (2018) Machine learning in cardiovascular machine: are we there yet? Heart (Bristish Cardiac Society). https://doi.org/10.1136/heartjnl-2017-311198
Arumugam K, Naved M, Shinde PP, Leiva-Chauca O, Huaman-Osorio A, Yanac TG (2021) Multiple disease prediction using machine learning algorithms. Materials Today Proc. https://doi.org/10.1016/j.matpr.2021.07.361
Lin KH, Hu YJ (2018) Application of machine learning to immune disease prediction. Int J Eng Innov Technol. https://doi.org/10.1038/s41746-020-0229-3
Li H, Luo M, Zheng J, Luo J, Zeng R, Feng N, Du Q, Fang J (2017) An artificial neural network prediction model of congenital heart disease based on risk factors: A hospital-based case-control study. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000006090
Haghpanahi M, Borkholder DA (2014) Fetal QRS extraction from abdominal recordings via model-based signal processing and intelligent signal merging. Physiol Meas. https://doi.org/10.1088/0967-3334/35/8/1591
Abbasi H, Bennet L, Gunn AJ, Unsworth CP (2017) Robust wavelet stabilized “footprints of uncertainty” for fuzzy system classifiers to automatically detect sharp waves in the EEG after hypoxia ischemia. Int J Neural Syst. https://doi.org/10.1142/S0129065716500519
Miao JH, Miao KH (2018) Cardiotocographic diagnosis of fetal health based on multiclass morphologic pattern predictions using deep learning classification. International Journal of Advanced Computer Science and Application. https://doi.org/10.14569/IJACSA.2018.090501
Akbulut A, Ertugrul E, Topcu V (2018) Fetal health status prediction based on maternal clinical history using machine learning techniques. Computer Methods Progr Biomed. https://doi.org/10.1016/j.cmpb.2018.06.010
Ng K, Ghoting A, Steinhubl SR, Stewart WF, Malin B, Sun J (2014) PARAMO: a PARAllel predictive modeling platform for healthcare analytic research using electronic health records. J Biomed Inform. https://doi.org/10.1016/j.jbi.2013.12.012
Pisapia JM, Akbari H, Rozycki M, Goldstein H, Bakas S, Rathore S et al (2018) Use of fetal magnetic resonance image analysis and machine learning to predict the need for postnatal cerebrospinal fluid diversion in fetal ventriculomegaly. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2017.3993
Feng B, Samuel DC, Hoskins W, Guo Y, Zhang Y, Tang J, Meng Z (2017) Down syndrome prediction/screening model based on deep learning and illumina genoty** array. IEEE International Conference on Bioinformatics and Biomedicine (BIBM), pp. 347–352. https://doi.org/10.1109/BIBM.2017.8217674
Neocleous AC, Nicolaides KH, Schizas CN (2018) Two-stage approach for risk estimation of fetal trisomy 21 and other aneuploidies using computational intelligence systems. Ultrasound Obstet Gynecol. https://doi.org/10.1002/uog.17558
Somasundaram D (2018) Machine learning approach for homolog chromosome Classification. Int J Imaging Syst Technol. https://doi.org/10.1002/ima.22287
Neocleous AC, Nicolaides KH, Schizas CN (2017) Intelligent noninvasive diagnosis of aneuploidy: raw values and highly imbalanced dataset. IEEE J Biomed Health Informatics. https://doi.org/10.1109/JBHI.2016.2608859
Qin Y, Wen J, Zheng H, Huang X, Yang J, Song N, Zhu YM, et al. (2019) Varifocal-net: a chromosome classification approach using deep convolutional networks. Computer vision and pattern recognition IEEE TMI for future publication. https://doi.org/10.1109/TMI.2019.2905841
Jaganathan M, Gopal R, Kiruthika VR (2019) Modelling an effectual feature selection approach for predicting down syndrome using machine learning approaches. International Journal of Aquatic Science, pp. 1238–1249
Al-Kharraz MS, Elrefaei LA, Fadel MA (2020) Automated system for chromosome karyoty** to recognize the most common numerical abnormalities using deep learning. IEEE Access. https://doi.org/10.1109/ACCESS.2020.3019937
Xu X, Wang L, Cheng X, Ke W, Jie S, Lin S, Lai M, Zhang L, Li Z (2022) Machine learning-based evaluation of application value of the USM combined with NIPT in the diagnosis of fetal chromosomal abnormalities. Math Biosci Eng. https://doi.org/10.3934/mbe.2022197
Nimitha N, Abbiraamavallee S, Elakiya E, Harini J, Kotishree V (2022) Supervised chromosomal anomaly detection using VGG-16 CNN model. AIP Conf Proc. https://doi.org/10.1063/50072491
Bhardwaj P, Bhandari G, Kumar Y, Gupta S (2022) An investigational approach for the prediction of gastric cancer using artificial intelligence techniques: a systematic review. Arch Comput Methods Eng. https://doi.org/10.1007/s11831-022-09737-4
Luo Y, Li Z, Guo H, Cao H, Song C, Guo X, Zhang Y (2017) Predicting congenital heart defects: a comparison of three data mining methods. PLoS ONE. https://doi.org/10.1371/journal.pone.0177811
Gupta A, Koul A, Kumar Y (2022) Pancreatic Cancer Detection using Machine and Deep Learning Techniques. 2022 2nd International Conference on Innovative Practices in Technology and Management (ICIPTM), 2, 151–155. https://doi.org/10.1109/ICIPTM54933.2022.9754010
Buscema M, Grossi E, Montanini L, Street ME (2015) Data mining of determinants of intrauterine growth retardation revisited using novel algorithms generating semantic maps and prototypical discriminating variable profiles. PLoS ONE. https://doi.org/10.1371/journal.pone.0126020
Wosiak A, Zamecznik A, Jarosik KN (2016) Supervised and unsupervised machine learning for improved identification of intrauterine growth restriction types. Proceedings of the federated conference on computer science and information systems, https://doi.org/10.15439/2016F515
Bahado-Singh RO, Yilmaz A, Bisgin H, Turkoglu O, Kumar P et al (2019) Artificial intelligence and the analysis of multiplatform metabolomics data for the detection of intrauterine growth restriction. Metabol Anal Intrauter Growth Restrict. https://doi.org/10.1371/journal.pone.0214121
Sufriyana H, Wu YW, Su YCU (2020) Prediction of preeclampsia and intrauterine growth restriction: development of machine learning models on a prospective cohort. JMIR Med Inform. https://doi.org/10.2196/15411
Pini N, Lucchini M, Esposito G, Tagliaferri S, Campanile M et al (2021) A machine learning approach to monitor the emergence of late intrauterine growth restriction. Front Med Sci. https://doi.org/10.3389/frai.2021.622616
Crockart IC, Brink LT, Plessis CD, Odendaal HJ (2021) Classification of intrauterine growth restriction at 34–38 weeks gestation with machine learning models. Inform Med Unlocked. https://doi.org/10.1016/j.imu.2021.100533
Teng LY, Mattar CNZ, Biswas A, Hoo WL, Saw SN (2022) Interpreting the role of nuchal fold for fetal growth restriction prediction using machine learning. Sci Rep. https://doi.org/10.1038/s41598-022-07883-0
Aslam N, Khan IU, Aljishi RF, Alnamer ZM, Alzawad ZM et al (2022) Explainable computational intelligence model for antepartum fetal monitoring to predict the risk of IUGR. Defin Eng Govern Green Artif Intell. https://doi.org/10.3390/electronics11040593
Gupta S, Kumar Y (2022) Cancer prognosis using artificial intelligence-based techniques. SN Comput Sci 3(1):1–8. https://doi.org/10.1007/s42979-021-00964-3
Carnimeo L (2008) An Intelligent Analyzer for Supporting Diagnoses of Congenital CMV Infection. Advanced Intelligent Computing Theories and Applications With Aspects of Artificial Intelligence, Springer, pp. 1069–1076. https://doi.org/10.1007/978-3-540-85984-0_128
Koul A, Bawa RK, Kumar Y (2022) Artificial intelligence in medical image processing for airway diseases. Connected e-Health. Springer, Cham, pp 217–254
Boger RA, Boger YS, Foster CB, Boger Z (2008) The use of artificial neural networks in prediction of congenital CMV outcome from sequence data. Bioinform Biol Insights. https://doi.org/10.4137/bbi.s764
Tanimura K, Yamada H (2018) Potential biomarkers for predicting congenital cytomegalovirus infection. Int J Mol Sci. https://doi.org/10.3390/ijms19123760
Rogers R, Saharia K, Chandorkar A, Weiss ZF, Vieira K, Koo S, Farmakiotis D (2020) Clinical experience with a novel assay measuring cytomegalovirus (CMV)-specific CD4+ and CD8+ T-cell immunity by flow cytometry and intracellular cytokine staining to predict clinically significant CMV events. BMC Infect Dis. https://doi.org/10.1186/s12879-020-4787-4
Deepa K, Suganya S (2020) Multiple attribute feature extraction and high support vector classifier for identification of cytomegalovirus images. ICTACT journal on image and video processing. https://doi.org/10.21917/ijivp.2020.0324
Hu Z, Tanga A, Singha J, Bhattacharyaa S, Butte AJ (2020) A robust and interpretable end-to-end deep learning model for cytometry data. National Center of Biotechnology Information. https://doi.org/10.1073/pnas.2003026117
Lee JS, Yun J, Ham S, Park H, Lee H, Kim J, Byeon JS et al (2021) Machine learning approach for differentiating cytomegalovirus esophagitis from herpes simplex virus esophagitis. Sci Rep. https://doi.org/10.1038/s41598-020-78556-z
Eisenberg L, Brossette C, Rauch J, Grandjean A, Ottinger H, Rissland J, Schwarz U, Graf N et al (2022) Time-dependent prediction of mortality and cytomegalovirus reactivation after allogeneic hematopoietic cell transplantation using machine learning. MedRxiv. https://doi.org/10.1101/2021.09.14.21263446
Jiang D, Hao M, Ding F, Fu J, Li M (2018) Map** the transmission risk of Zika virus using machine learning models. Acta Trop. https://doi.org/10.1016/j.actatropica.2018.06.021
Mahalakshmi B, Suseendran G (2019) Prediction of zika virus by multilayer perceptron neural network (MLPNN) using cloud. International Journal of Recent Technology and Engineering (IJRTE). https://doi.org/10.35940/ijrte.B1041.0982S1119
Lusk R, Zimmerman J, Maldeghem KV, Kim S, Roth NM, Lavinder J et al (2020) Exploratory analysis of machine learning approaches for surveillance of Zika-associated birth defects. Birth Defects Res. https://doi.org/10.1002/bdr2.1767
Herry CL, Soares HMF, Faccini LS, Frasch MG (2021) Machine learning model on heart rate variability metrics identifies asymptomatic toddlers exposed to zika virus during pregnancy. Physiol Meas. https://doi.org/10.1088/1361-6579/ac010e
Veiga RV, Faccini LS, França GVA et al (2021) Classification algorithm for congenital Zika Syndrome: characterizations, diagnosis and validation. Sci Rep. https://doi.org/10.1038/s41598-021-86361-5
Dadheech P, Mehbodniya A, Tiwari S, Kumar S, Singh P, Gupta S (2022) Zika virus prediction using ai-driven technology and hybrid optimization algorithm in healthcare. J Healthcare Eng. https://doi.org/10.1155/2022/2793850
Tejera E, Areias MJ, Rodrigues A, Ramõa A, Nieto-villar JM, Rebelo I (2011) Artificial neural network for normal, hypertensive, and preeclamptic pregnancy classification usingmaternal heart rate variability Indexes. J Matern Neonatal Med. https://doi.org/10.3109/14767058.2010.545916
Moreira MWL, Rodrigues JLPC, Al-Muhtadi J, Korotaev VV, Albuquerque VHC (2018) Neuro-fuzzy model for HELLP syndrome prediction in mobile cloud computing environments. Concurrency Comput Pract Expert. https://doi.org/10.1002/cpe.4651
Tahir M, Badriyah T, Syarif I (2018) Classification algorithms of maternal risk detection for preeclampsia with hypertension during pregnancy using particle swarm optimization. Emitter Int J Eng Technol. https://doi.org/10.24003/emitter.v6i2.287
Bennett R, Mulla ZD, Parikh P, Hauspurg A, Razzaghi T (2022) An imbalance-aware deep neural network for early prediction of preeclampsia. PLoS ONE. https://doi.org/10.1371/journal.pone.0266042
Kumar Y, Gupta S (2022) Deep transfer learning approaches to predict glaucoma, cataract, choroidal neovascularization, diabetic macular edema, drusen and healthy eyes: an experimental review. Arch Comput Methods Eng. https://doi.org/10.1007/s11831-022-09807-7
Kumar Y, Gupta S, Singla R, Hu YC (2022) A systematic review of artificial intelligence techniques in cancer prediction and diagnosis. Arch Comput Methods Eng 29(4):2043–2070. https://doi.org/10.1007/s11831-021-09648-w
Kumar Y, Koul A, Mahajan S (2022) A deep learning approaches and fastai text classification to predict 25 medical diseases from medical speech utterances, transcription and intent. Soft Comput 26(17):8253–8272. https://doi.org/10.1007/s00500-022-07261-y
Kumar Y, Patel NP, Koul A, Gupta A (2022) Early Prediction of Neonatal Jaundice using Artificial Intelligence Techniques. 2022 2nd International Conference on Innovative Practices in Technology and Management (ICIPTM), 2, 222–226. https://doi.org/10.1109/ICIPTM54933.2022.9753884
Kumar Y, Singla R (2022) Effectiveness of machine and deep learning in iot-enabled devices for healthcare system. In: Ghosh U, Chakraborty C, Garg L, Srivastava G (eds) Intelligent internet of things for healthcare and industry. Springer, Cham, pp 1–19
Zhong H, **ao J (2019) Retracted: enhancing health risk prediction with deep learning on big data and revised fusion node paradigm. Hindawi. https://doi.org/10.1155/2019/9757658
Uddin S, Khan A, Hossain ME, Moni MA (2019) Comparing different supervised machine learning algorithms for disease prediction. BMC Med Inform Decis Mak. https://doi.org/10.1186/s12911-019-1004-8
Katarya R, Srinivas P (2020) Predicting heart disease at early stages using machine learning: A survey. In 2020 International Conference on electronics and sustainable communication systems (ICESC), pp. 302–305. https://doi.org/10.1109/ICESC48915.2020.9155586
Sharma M, Swati, Vig L (2018) Automatic Chromosome Classification using Deep Attention Based Sequence Learning of Chromosome Bands. in 2018 International Joint Conference on Neural Networks (IJCNN), IEEE. https://doi.org/10.1109/IJCNN.2018.8489321
Kohli PS, Arora S (2018) Application of machine learning in disease prediction. In 2018 4th International Conference on computing communication and automation (ICCCA), pp. 1–4. https://doi.org/10.1109/CCAA.2018.8777449
Yuan FQ (2016) Critical issues of applying machine learning to condition monitoring for failure diagnosis. IEEE International Conference on industrial engineering and engineering management (IEEM). https://doi.org/10.1109/IEEM.2016.7798209
Ismaeel S, Miri A, Chourishi D (2015) Using the extreme learning machine (elm) technique for heart disease diagnosis. IEEE Canada International humanitarian technology conference (IHTC2015). https://doi.org/10.1109/IHTC.2015.7238043
Dengju Y, Yang J, Zhan X (2013) A novel method for disease prediction: Hybrid of random forest and multivariate adaptive regression splines. Journal of Computers (Finland). https://doi.org/10.4304/jcp.8.1.170-177
Dessi A, Ottonello G, Fanos V (2012) Physiopathology of intrauterine growth retardation: from classic data to metabolomics. J Matern Fetal Neonatal Med. https://doi.org/10.3109/14767058.2012.714639
Lakshmi BN, Indumathi TS, Ravi N (2015) Prediction based health monitoring in pregnant women. International Conference on Applied and Theoreti- cal Computing and Communication Technology (iCATccT), IEEE. https://doi.org/10.1109/ICATCCT.2015.7456954
Zea-Vera A, Ochoa TJ (2015) Challenges in the diagnosis and management of neonatal sepsis. J Trop Pediatr. https://doi.org/10.1093/tropej/fmu079
Hou B, Khanal B, Alansary A, McDonagh S, Davidson A, Rutherford M, Hajnal JV et al (2018) 3-D reconstruction in canonical co-ordinate space from arbitrarily oriented 2-D images. IEEE Trans Med Imaging. https://doi.org/10.1109/TMI.2018.2798801
He F, Lin B, Mou K, ** L, Liu J (2021) A machine learning model for the prediction of down syndrome in second trimester antenatal screening. Clin Chim Acta. https://doi.org/10.1016/j.cca.2021.07.015
Jamshidnezhad A, Hosseini SM, Mohammadi-Asl J, Mahmudi M (2021) An intelligent prenatal screening system for the prediction of Trisomy-21. Inform Med Unlocked. https://doi.org/10.1016/j.imu.2021.100625
Bharti R, Khamparia A, Shabaz M, Dhiman G, Pande S, Singh P (2021) Prediction of heart disease using a combination of machine learning and deep learning. Comput Intell Neurosci. https://doi.org/10.1155/2021/8387680
Rani S, Masood S (2020) Predicting congenital heart disease using machine learning techniques. J Discret Math Sci Cryptogr. https://doi.org/10.1080/09720529.2020.1721862
Clifford GD, Silva I, Behar J, Moody GB (2017) Non-invasive fetal ECG analysis. Physiol Meas. https://doi.org/10.1088/0967-3334/35/8/1521
Bauer ME, Bateman BT, Bauer ST, Shanks AM, Mhyre JM (2013) Maternal sepsis mortality and morbidity during hospitalization for delivery: temporal trends and independent associations for severe sepsis. Anesth Analg. https://doi.org/10.1213/ANE.0b013e3182a009c3
Bansal K, Bathla RK, Kumar Y (2022) Deep transfer learning techniques with hybrid optimization in early prediction and diagnosis of different types of oral cancer. Soft Comput 26(21):11153–11184. https://doi.org/10.1007/s00500-022-07246-x
Khalilia M, Chakraborty S, Popescu M (2011) Predicting disease risks from highly imbalanced data using random forest. BMC Med Inform Decis Mak. https://doi.org/10.1186/1472-6947-11-51
Vinitha S, Sweetlin S, Vinusha H, Sa**i S (2018) Disease prediction using machine learning over big data. Int J Comput Sci Eng. https://doi.org/10.2139/ssrn.3458775
Patil M, Lobo VB, Puranik P, Pawaskar A, Pai A, Mishra R (2018) A proposed model for lifestyle disease prediction using support vector machine. In 2018 9th International Conference on computing, communication and networking technologies (ICCCNT). https://doi.org/10.1109/ICCCNT.2018.8493897
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaur, K., Singh, C. & Kumar, Y. Diagnosis and Detection of Congenital Diseases in New-Borns or Fetuses Using Artificial Intelligence Techniques: A Systematic Review. Arch Computat Methods Eng 30, 3031–3058 (2023). https://doi.org/10.1007/s11831-023-09892-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11831-023-09892-2