Abstract
Recombinant retroviruses, including lentiviruses, are the most widely used vectors for both in vitro and in vivo stable gene transfer. However, the inability to selectively deliver transgenes into cells of interest limits the use of this technology. Due to its wide tropism, stability and ability to pseudotype a range of viral vectors, vesicular stomatitis virus G protein (VSV-G) is the most commonly used pseudoty** protein. Here, we attempted to engineer this protein for targeting purposes. Chimaeric VSV-G proteins were constructed by linking a cell-directing single-chain antibody (scFv) to its N-terminal. We show that the chimaeric VSV-G molecules can integrate into retroviral and lentiviral particles. HIV-1 particles pseudotyped with VSV-G linked to an scFv against human Major Histocompatibility Complex class I (MHC-I) bind strongly and specifically to human cells. Also, this novel molecule preferentially drives lentiviral transduction of human cells, although the titre is considerably lower that viruses pseudotyped with VSV-G. This is likely due to the inefficient fusion activity of the modified protein. To our knowledge, this is the first report where VSV-G was successfully engineered to include a large (253 amino acids) exogenous peptide and where attempts were made to change the infection profile of VSV-G pseudotyped vectors.
Similar content being viewed by others
Background
Retroviruses, including lentiviruses, integrate into the genome of host cells, and the expression of the transduced genes can persist throughout cell divisions. Hence, murine leukemia virus (MLV)- and lentivirus-based vectors are among the most commonly used tools for gene transfer in eukaryotic cells in the laboratory, and may one day become clinically important. Lentiviral vectors have also the additional advantage of transducing non-dividing cells, which broadens their application to both resting and terminally differentiated cells.
Despite continuous improvement of retroviral and lentiviral gene transfer over the past years [1–3], the current inability to target infection to cells of interest remains a severe limitation, preventing the development of efficient, safe and cost-effective clinical application. A number of reports have already been published to this end (for review, see [4–6]). The majority of these studies were attempts to redirect the tropism of the ecotropic envelope glycoprotein (GP) of MLVs by the addition of ligand motifs, which bind to specific molecules associated with the cell membrane. However, these approaches generally met with limited success. Although the engineered viruses usually did bind to the new receptors, infection titres were low. Inefficient transduction was mostly due to diminished fusion activity of the engineered GP, which consequently prevented infectious translocation of the viral capsids into cells [7–9].
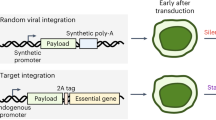
Retroviral and lentiviral GPs are made of two parts, produced from the same precursor following proteolytic maturation. SU, or surface protein, recognises the viral receptor, and TM, the transmembrane protein, carries the fusion activity and tethers the GP to virions [4–6]. However, retroviruses and lentiviruses can be pseudotyped by a number of GPs from other viruses, such as the hemagglutinin (HA) of influenza virus, the envelope proteins (E1 and E2) of Sindbis virus and the G protein of vesicular stomatitis virus (VSV-G). These have all higher fusion activity than the native GPs and remain tightly attached to virions. HA has already been engineered for targeting purposes through N-terminal addition of various ligands, of which one successfully redirected MLV tropism towards human melanoma cells [10]. E2 has also been genetically modified to display the immunoglobulin-binding domain of Staphylococcus aureus protein A [14, 15]. VSV-G is a trimerised transmembrane molecule, although its exact structure is not fully known. Moreover, its ligand has not been identified [16], which hampers rational design of targeting strategies. Additionally, only a few permissible sites for short (2–10 amino acids) peptide insertions have been isolated [17–20]. Nevertheless, these studies all confirmed that VSV-G might be amenable to genetic engineering for targeting purposes. Guibinga et al inserted a 10 amino acid collagen-binding peptide close to the N-terminal of VSV-G, and could show specific attachment of MLV- and HIV-1-based vectors to collagen matrix [17]. To date, however, no redirected cell transduction has been reported. We therefore attempted to target infection by attaching a large ligand binding domain, an scFv against MHC-I, directly in the N-terminal of the protein, a site that Yu and Schaffer confirmed permissive. We show that the novel GP, with its large exogenous peptide, (i) is processed and transported to the cell surface, (ii) provides a new binding specificity but (iv) transduces target cells very inefficiently, although better than control scFv/VSV-G. We speculate that this is due to an inefficient fusion activity, and discuss potential improvements.
Results and discussion
As a model system, we decided to target MHC-I molecules on human cells, as these membrane receptors can mediate cell infection by retroviral and lentiviral vectors [ The 1.6 kB HindIII-BamHI VSV-G fragment (serotype Indiana) was transferred from pFB. VSV-G into pcDNA3 (InVitrogen). To introduce a HA tag in the C terminal of VSV-G, the cDNA was amplified with a T7-specific sense primer (5' TAATACGATCACTTTAGGG) and an antisense oligo, including the HA sequence (in miniscule), a stopcodon and an Xho site (5' CCCCTCGAG TTA agcgtaatcaggaacatcataaggata CTTTCCAAGTCGGTTCATCTC). The product was digested with HindIII and XhoI, and reinserted into pcDNA3. To generate scFv/VSV-G molecules, the sequence for mature VSV-G (from amino acid 17) was amplified with a sense primer, also containing a NotI site and an additional nucleotide to retain the reading frame (5' CCCGCGGCCGC A AAGTTCACCATAGTTTTTCCACAC). The anti-sense primer hybridises to the HA sequence, contains a stopcodon and carries a Cla I site (5' CCCATCGAT TTA AGCGTAATCAGGAACATCATA). The NotI/ClaI restricted PCR product was ligated into NotI/ClaI-cleaved PM441 and PM442 plasmids [23]. These constructs originate from an MLV-derived plasmid (FBMOSALF [31]), modified to contain an scFv (αMHC and αHEL, [27]), upstream of the GP gene. Consequently, the resulting constructs (αMHC/VSV-G and αHEL/VSV-G) express the gene from the MLV LTR, with a MLV leader sequence and 6 additional amino acids from the virus (see Fig 1). Restriction enzymes were purchase from Roche or Invitrogene and all oligonucleotides were obtained from Sigma. HeLa [32], 293T [33], TelCeb6 [31], Cos-7 [34] and Mus Dunni cells [35] were grown at 37°C in Dulbecco's modified Eagle's medium (Sigma), supplemented with 10% heat inactivated foetal calf serum (Gibco), 100 units/ml streptomycin, 100 units/ml penicillin and 2 mM L-glutamine in a humified 5% CO2 incubator. HeLa or 293T cells were seeded on 6-well plate at 60% confluency. The following day, cells were transiently transfected using the classic CaPO4 co-precipitation method [36] with 5 μg DNA/well. The precipitate was removed and gene expression was confirmed 24–48 hours later by Western Blot, immunofluorescence or flow cytometry. To express HIV-1 particles, 293T cells (75% density) in a 10-cm culture plate were transiently transfected with 5 μg of an LTR-driven EGFP vector (pHRCMV-EGFP) and 4 μg of a helper plasmid (pCMV△8.2) [29]. 5 μg VSV-G or 30 μg scFv/VSV-G plasmids were also included. DNA precipitate was removed after 16 hours, and the viral supernatants were collected 24–48 hours later. For virion protein preparation, 1 ml of culture supernatant from virus producing cells were adjusted to 10 mM CaCl2 and left at room temperature for 30 minutes. Precipitated viruses were spun down at 13 k rpm at 4°C for 1 minute and resuspended in 50 μl of electrophoresis loading buffer. Cells were resuspended in triplex lysis buffer (50 mM Tris-HCl pH8.0, 150 mM NaCl, 0.2% NaN3, 0.1% SDS, 1% NP40, 0.5% Na-deoxycholate, 2 mg/ml leupeptin, 1 mM phenylmethyl sulfone fluoride) and left on ice for 30 minutes. Cell debris and nuclei were removed by centrifugation (13 k rpm at 4°C for 10 minutes). The samples were fractionated through SDS polyacrylamide (10%) gels (SDS-PAGE) and transferred to Protran nitrocellulose membranes (Schleicher and Schuell). VSV-G and scFv/VSV-G carry an HA tag, and were detected by a rat anti-HA antibody (Sigma), followed by a horseradish peroxidase (HPO) conjugated anti-RatIgG (Dako). p24Gag, detected by SF2 rabbit monoclonal antibody (NIH AIDS Research and Reference Reagent Program) and an anti-rabbit IgG/HPO (Santa Cruz), was used as an internal reference to normalise the virion proteins. The membranes were developed with Renaissance chemoluminescence kit (NEN Life Science Products), as recommended by the supplier. Transfected HeLa or 293T cells were incubated with a conformation specific anti-VSV-G antibody (5G8F11, a generous gift by Dr Douglas Lyles, Winston-Salem) for 30 minutes, washed and revealed by a fluorescein isothiocyanate conjugated anti-mouse IgG antibody (FITC-anti-MuIg; Sigma). VSV-G expressing cells were detected under a fluorescence microscope (Zeiss). Distribution of intracellular, HA-tagged VSV-G was assessed in paraformaldehyde-fixed, Triton-X permeabilised transfected HeLa cells, grown on cover slips. The proteins were visualised with a rat anti-HA antibody together with a FITC labelled anti-Rat IgG (both Sigma), and analysed with a confocal microscope (Leica). 2 × 105 transfected 293T cells were collected in phosphate buffered saline (PBS), incubated in block buffer (BB: 10% bovines serum albumin, 0.1 M Glycine in PBS) for 30 minutes on ice, which was replaced by 200 μl of 5G8F11 hybridoma supernatant. After 1 hour on ice, the cells were washed twice with BB and resuspended in 100 μl FITC-anti-MuIg. The cells were rinsed again after 1 hour, fixed with 0.2 % formaldehyde and analysed on a FACScalibur fluorescence-activated cell sorter (Becton Dickinson). 5 × 105 human 293T and HeLa cells, and Mus Dunni cells were incubated with 1 ml pseudotyped HIV-1 particles from transiently transfected 293T cells for 30 minutes on ice. Cells were washed two times with PBS. scFv/VSV-Gs or VSV-G, attached to the cell surfaces, were detected as previously described. Supernatant from HIV-1-producing 293T cells were passed through a 0.45 μm filter (Sarstedt). Some samples were concentrated 100 times by centrifugation (25 k rpm at 4°C for 2 hours in a BeckmanCoulter ultracentrifuge) and were carefully resuspended in 1% BSA. When required, the virus was stored at -80°C. 50% confluent target cells, either human 293T and HeLa cells, mouse Mus Dunni cells or monkey Cos-7 cells, were cultured with dilutions of virus for 16 hours in the presence of 5 mg/ml polybrene. 48 hours later, green fluorescent colonies were counted or cells were analysed by flow cytometry. To block αMHC/VSV-G driven infection, target cells were preincubated with the B9.12.1 (< 1 μg/ml, Beckman Coulters) for 30 minutes before addition of the virus.Materials and methods
Engineering of VSV-G and scFv/VSV-G expression plasmids
Cells and culture conditions
Transient expression of αMHC/VSV-G and αHEL/VSV-G
Production of VSV-G and scFv/VSV-G pseudotyped lentiviral particles
Immunoblotting assays of VSV-G and scFv/VSV-G
Detection of scFv/VSV-G by immunofluorescence assay
Detection of scFv/VSV-G by flow cytometry
VSV-G binding assays
Infection assays
References
Lundstrom K: Latest development in viral vectors for gene therapy. Trends Biotechnol 2003, 21: 117-122. 10.1016/S0167-7799(02)00042-2
Gould DJ, Favorov P: Vectors for the treatment of autoimmune disease. Gene Ther 2003, 10: 912-927. 10.1038/sj.gt.3302018
Sinn PL, Sauter SL, McCray PBJ: Gene therapy progress and prospects: development of improved lentiviral and retroviral vectors--design, biosafety, and production. Gene Ther 2005, 12: 1089-1098. 10.1038/sj.gt.3302570
Sandrin V, Russell SJ, Cosset FL: Targeting retroviral and lentiviral vectors. Curr Top Microbiol Immunol 2003, 281: 137-178.
Lavillette D, Russell SJ, Cosset FL: Retargeting gene delivery using surface-engineered retroviral vector particles. Curr Opin Biotechnol 2001, 12: 461-466. 10.1016/S0958-1669(00)00246-9
Karavanas G, Marin M, Salmons B, Gunzburg WH, Piechaczyk M: Cell targeting by murine retroviral vectors. Crit Rev Oncol Hematol 1998, 28: 7-30.
Zhao Y, Zhu L, Lee S, Li L, Chang E, Soong NW, Douer D, Anderson WF: Identification of the block in targeted retroviral-mediated gene transfer. Proc Natl Acad Sci U S A 1999, 96: 4005-4010. 10.1073/pnas.96.7.4005
Benedict CA, Tun RY, Rubinstein DB, Guillaume T, Cannon PM, Anderson WF: Targeting retroviral vectors to CD34-expressing cells: binding to CD34 does not catalyze virus-cell fusion. Hum Gene Ther 1999, 10: 545-557. 10.1089/10430349950018625
Karavanas G, Marin M, Bachrach E, Papavassiliou AG, Piechaczyk M: The insertion of an anti-MHC I ScFv into the N-terminus of an ecotropic MLV glycoprotein does not alter its fusiogenic potential on murine cells. Virus Res 2002, 83: 57-69. 10.1016/S0168-1702(01)00419-1
Hatziioannou T, Delahaye E, Martin F, Russell SJ, Cosset FL: Retroviral display of functional binding domains fused to the amino terminus of influenza hemagglutinin. Hum Gene Ther 1999, 10: 1533-1544. 10.1089/10430349950017860
Morizono K, Bristol G, **e YM, Kung SK, Chen IS: Antibody-directed targeting of retroviral vectors via cell surface antigens. J Virol 2001, 75: 8016-8020. 10.1128/JVI.75.17.8016-8020.2001
Morizono K, **e Y, Ringpis GE, Johnson M, Nassanian H, Lee B, Wu L, Chen IS: Lentiviral vector retargeting to P-glycoprotein on metastatic melanoma through intravenous injection. Nat Med 2005, 11: 346-352. 10.1038/nm1192
Aires da Silva F, Costa MJ, Corte-Real S, Goncalves J: Cell type-specific targeting with sindbis pseudotyped lentiviral vectors displaying anti-CCR5 single-chain antibodies. Hum Gene Ther 2005, 16: 223-234. 10.1089/hum.2005.16.223
Lu X, Humeau L, Slepushkin V, Binder G, Yu Q, Slepushkina T, Chen Z, Merling R, Davis B, Chang YN, Dropulic B: Safe two-plasmid production for the first clinical lentivirus vector that achieves >99% transduction in primary cells using a one-step protocol. J Gene Med 2004, 6: 963-973. 10.1002/jgm.593
Quinonez R, Sutton RE: Lentiviral vectors for gene delivery into cells. DNA Cell Biol 2002, 21: 937-951. 10.1089/104454902762053873
Coil DA, Miller AD: Phosphatidylserine is not the cell surface receptor for vesicular stomatitis virus. J Virol 2004, 78: 10920-10926. 10.1128/JVI.78.20.10920-10926.2004
Guibinga GH, Hall FL, Gordon EM, Ruoslahti E, Friedmann T: Ligand-modified vesicular stomatitis virus glycoprotein displays a temperature-sensitive intracellular trafficking and virus assembly phenotype. Mol Ther 2004, 9: 76-84. 10.1016/j.ymthe.2003.09.018
Li Y, Drone C, Sat E, Ghosh HP: Mutational analysis of the vesicular stomatitis virus glycoprotein G for membrane fusion domains. J Virol 1993, 67: 4070-4077.
Schlehuber LD, Rose JK: Prediction and identification of a permissive epitope insertion site in the vesicular stomatitis virus glycoprotein. J Virol 2004, 78: 5079-5087. 10.1128/JVI.78.10.5079-5087.2004
Yu JH, Schaffer DV: Selection of novel vesicular stomatitis virus glycoprotein variants from a peptide insertion library for enhanced purification of retroviral and lentiviral vectors. J Virol 2006, 80: 3285-3292. 10.1128/JVI.80.7.3285-3292.2006
Roux P, Jeanteur P, Piechaczyk M: A versatile and potentially general approach to the targeting of specific cell types by retroviruses: application to the infection of human cells by means of major histocompatibility complex class I and class II antigens by mouse ecotropic murine leukemia virus-derived viruses. Proc Natl Acad Sci U S A 1989, 86: 9079-9083. 10.1073/pnas.86.23.9079
Etienne-Julan M, Roux P, Carillo S, Jeanteur P, Piechaczyk M: The efficiency of cell targeting by recombinant retroviruses depends on the nature of the receptor and the composition of the artificial cell-virus linker. J Gen Virol 1992, 73 ( Pt 12): 3251-3255.
Marin M, Noel D, Valsesia-Wittman S, Brockly F, Etienne-Julan M, Russell S, Cosset FL, Piechaczyk M: Targeted infection of human cells via major histocompatibility complex class I molecules by Moloney murine leukemia virus-derived viruses displaying single-chain antibody fragment-envelope fusion proteins. J Virol 1996, 70: 2957-2962.
Rebai N, Malissen B: Structural and genetic analyses of HLA class I molecules using monoclonal xenoantibodies. Tissue Antigens 1983, 22: 107-117.
Briant L, Benkirane M, Girard M, Hirn M, Iosef C, Devaux C: Inhibition of human immunodeficiency virus type 1 production in infected peripheral blood mononuclear cells by human leukocyte antigen class I-specific antibodies: evidence for a novel antiviral mechanism. J Virol 1996, 70: 5213-5220.
Ward ES, Gussow D, Griffiths AD, Jones PT, Winter G: Binding activities of a repertoire of single immunoglobulin variable domains secreted from Escherichia coli. Nature 1989, 341: 544-546. 10.1038/341544a0
Russell SJ, Hawkins RE, Winter G: Retroviral vectors displaying functional antibody fragments. Nucleic Acids Res 1993, 21: 1081-1085.
Coll JM: The glycoprotein G of rhabdoviruses. Arch Virol 1995, 140: 827-851. 10.1007/BF01314961
Naldini L, Blomer U, Gallay P, Ory D, Mulligan R, Gage FH, Verma IM, D. T: In vivo gene delivery and stable transduction of nondividing cells by a lentiviral vector. Science 1996, 272: 263-267.
Schlegel R, Sue TT, Willingham MC, Pastan I: Inhibition of VSV binding and infectivity by phosphatidylserine: is phosphatidylserine a VSV-bidning site? Cell 1983, 32: 639-646. 10.1016/0092-8674(83)90483-X
Cosset FL, Takeuchi Y, Battini JL, Weiss RA, Collins MK: High-titer packaging cells producing recombinant retroviruses resistant to human serum. J Virol 1995, 69: 7430-7436.
Scherer WF, Syverton JT, Gey GO: Studies on the propagation in vitro of poliomyelitis viruses. IV. Viral multiplication in a stable strain of human malignant epithelial cells (strain HeLa) derived from an epidermoid carcinoma of the cervix. J Exp Med 1953, 97: 695-710. 10.1084/jem.97.5.695
Graham FL, Smiley J, Russell WC, Nairn R: Characteristics of a human cell line transformed by DNA from human adenovirus type 5. J Gen Virol 1977, 36: 59-74.
Gluzman Y: SV40-transformed simian cells support the replication of early SV40 mutants. Cell 1981, 23: 175-182. 10.1016/0092-8674(81)90282-8
Lander MR, Chattopadhyay SK: A Mus dunni cell line that lacks sequences closely related to endogenous murine leukemia viruses and can be infected by ectropic, amphotropic, xenotropic, and mink cell focus-forming viruses. J Virol 1984, 52: 695-698.
Sambrook J, Fritsch E, Maniatis T: Molecular cloning: a laboratory manual. In Cold Spring Harbor Laboratory Press. 2nd edition. Cold Spring Harbor, Cold Spring Harbor Laboratory Press; 1989.
Acknowledgements
HD was funded by a Marie Curie Individual Training Fellowship. Dr Douglas Lyles, Winston-Salem NC, US, kindly provided the 5G811 hybridoma. Dr Gordon Daly helped proof reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
HD participated in the design of the project, carried out the practical work and drafted the manuscript. MP conceived and managed the project.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Dreja, H., Piechaczyk, M. The effects of N-terminal insertion into VSV-G of an scFv peptide. Virol J 3, 69 (2006). https://doi.org/10.1186/1743-422X-3-69
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1743-422X-3-69