Abstract
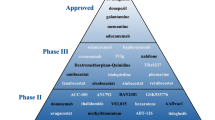
To date, symptomatic medications prevail as the mainstay of treatment options for Alzheimer’s disease (AD). There have been tremendous investments made to increase the numbers of drugs approved and the targets engaged, in an effort to alter the disease course or pathophysiology of AD. Unfortunately, almost all studies have not met expectations and no new drug (beyond medical foods) has been approved for the treatment of AD in the last decade. This review is a comparison of novel AD therapies in the late phases of clinical testing, including recent high-profile clinical failures, and agents in development with relatively unexplored mechanisms of action, with a focus on their potential as therapeutic agents and their proposed advantages over the treatments currently in use.
Similar content being viewed by others
References
Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60:1119–22.
Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM, Vogel FS, Hughes JP, van Belle G, Berg L. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology. 1991;41(4):479–86.
Atri A, Molinuevo JL, Lemming O, Wirth Y, Pulte I, Wilkinson D. Memantine in patients with Alzheimer’s disease receiving donepezil: new analyses of efficacy and safety for combination therapy. Alzheimers Res Ther. 2013;5(1):6.
Downing N, Aminawung A, Shah N, et al. Regulatory review of novel therapeutics—comparison of three regulatory agencies. N Engl J Med. 2012;366:2284–93.
Hock C, Konietzko U, Streffer JR, et al. Antibodies against beta-amyloid slow cognitive decline in Alzheimer’s disease. Neuron. 2003;38(4):547–54.
Alvarez X, Cacabelos R, Sampedro C, et al. Efficacy and safety of Cerebrolysin in moderate to moderately severe Alzheimer’s disease: results of a randomized, double-blind, controlled trial investigating three dosages of Cerebrolysin. Eur J Neurol. 2011;18(1):59–68.
Piette F, Belmin J, Vincent H, et al. Masitinib as an adjunct therapy for mild-to-moderate Alzheimer’s disease: a randomized, placebo-controlled phase 2 trial. Alzheimers Res Ther. 2011;3(2):16.
Landhuis L. Will tau drug show its true colors in phase 3 trials? Alzheimer Res Forum. October 2, 2012. http://www.alzforum.org/new/detail.asp?id=3283#ClaudeWischik.
Rinne JO, Brooks DJ, Rossor MN, et al. 11C-PiB PET assessment of change in fibrillar amyloid-beta load in patients with Alzheimer’s disease treated with bapineuzumab: a phase 2, double-blind, placebo-controlled, ascending-dose study. Lancet Neurol. 2010;9(4):363–72.
Juha RO, Brooks DJ, Rossor MN, et al. 11C-PiB PET assessment of change in fibrillar amyloid-β load in patients with Alzheimer’s disease treated with bapineuzumab: a phase 2, double-blind, placebo-controlled, ascending-dose study. Lancet Neurol. 2010;9(4):363–72.
Sperling R, Salloway S, Brooks DJ, et al. Amyloid-related imaging abnormalities in patients with Alzheimer’s disease treated with bapineuzumab: a retrospective analysis. Lancet Neurol. 2012;11(3):241–9.
Pfizer. Amyloid imaging and safety study of subcutaneous bapineuzumab in subjects with mild to moderate Alzheimer’s disease (SUMMIT AD). NCT01254773.
Imbimbo BP, Ottonello S, Frisardi V, et al. Solanezumab for the treatment of mild-to-moderate Alzheimer’s disease. Expert Rev Clin Immunol. 2012;8(2):135–49.
Goto T, Fujikoshi S, Uenaka K, et al. Solanezumab was safe and well-tolerated for Asian patients with mild-to-moderate Alzheimer’s disease in a multicenter, randomized, open-label, multi-dose study. Alzheimers Dement. 2012;6(4 Suppl):S308.
Gelinas DS, DaSilva K, Fenili D, et al. Immunotherapy for Alzheimer’s disease. PNAS. 2004;101(Suppl 2):14657–62.
Wilkinson K, El Khoury J. Microglial scavenger receptors and their roles in the pathogenesis of Alzheimer’s disease. Int J Alzheimer’s Dis. 2012;2012:Article ID 489456.
Willis B, Zhang W, Ayan-Oshodi M, et al. Semagacestat pharmacokinetics are not significantly affected by formulation, food, or time of dosing in healthy participants. J Clin Pharmacol. 2012;52(6):904–13.
Eriksen JL, Sagi SA, Smith TE, et al. NSAIDs and enantiomers of flurbiprofen target gamma-secretase and lower amyloid beta 42 in vivo. J Clin Investig. 2003;112(4):440–9.
Santa-Maria I, Hernández F, Del Rio J, et al. Tramiprosate, a drug of potential interest for the treatment of Alzheimer’s disease, promotes an abnormal aggregation of tau. Mol Neurodegener. 2007;6(2):17.
Gervais F, Paquette J, Morissette C, et al. Targeting soluble Aβ peptide with tramiprosate for the treatment of brain amyloidosis. Neurobiol Aging. 2007;28(4):537–47.
DeKosky S, Williamson J, Fitzpatrick A, et al. Ginkgo biloba for prevention of dementia: a randomized controlled trial. JAMA. 2008;300(19):2253–62.
Quinn J, Raman R, Thomas R, et al. Docosahexaenoic acid supplementation and cognitive decline in Alzheimer’s disease: a randomized trial. JAMA. 2010;304(17):1903–11.
Park S, Jung J, Lee H, et al. The memory ameliorating effects of INM-176, an ethanolic extract of Angelica gigas, against scopolamine- or AB(1–42)-induced dysfunction in mice. J Ethnopharmacol. 2012;143(2):611–20.
Salloway S, Sperling R, Keren R, et al. A phase 2 randomized trial of ELND005, scyllo-inositol, in mild to moderate Alzheimer’s disease. Neurology. 2011;77(13):1253–62.
Seo JS, Baek IS, Leem YH, et al. SK-PC-B70M alleviates neurologic symptoms in amyotrophic lateral sclerosis mice. Brain Res. 2011;12(1368):299–307.
Schmidt AM, Sahagan B, Nelson RB, et al. The role of RAGE in amyloid-beta peptide-mediated pathology in Alzheimer’s disease. Curr Opin Investig Drugs. 2009;10(7):672–80.
Yan SD, Chen X, Fu J, et al. RAGE and amyloid-beta peptide neurotoxicity in Alzheimer’s disease. Nature. 1996;382(6593):685–91.
Yan SD, Bierhaus A, Nawroth PP, Stern DM. RAGE and Alzheimer’s disease: a progression factor for amyloid-beta-induced cellular perturbation? J Alzheimers Dis. 2009;16(4):833–43.
Yan SD, Chen X, Walker DG. RAGE: a potential target for a-mediated cellular perturbation in Alzheimers disease. Curr Mol Med. 2007;7(8):735–42.
Carrano A, Hoozemans JJM, Van der Vies SM, et al. Amyloid beta induces oxidative stress-mediated blood–brain barrier changes in capillary amyloid angiopathy. Antioxid Redox Signal. 2011;15(5):1167–78.
Hartz AMS, Bauer B, Soldner ELB, et al. Amyloid-β contributes to blood–brain barrier leakage in transgenic human amyloid precursor protein mice and in humans with cerebral amyloid angiopathy. Stroke. 2012;43(2):514–23.
Kook S-Y, Hong HS, Moon M, et al. Ab1–42–RAGE interaction disrupts tight junctions of the blood–brain barrier via Ca2+–calcineurin signaling. J Neurosci. 2012;32(26):8845–54.
Deane R, Du Yan S, Submamaryan RK, et al. RAGE mediates amyloid-beta peptide transport across the blood–brain barrier and accumulation in brain. Nat Med. 2003;9(7):907–13.
Sabbagh MN, Agro A, Bell J, Aisen PS, et al. PF-04494700, an oral inhibitor of receptor for advanced glycation end products (RAGE), in Alzheimer disease. Alzheimer Dis Assoc Disord. 2011;25:206–12.
Chen M, Inestrosa NC, Ross GS, Fernandez HL. Platelets are the primary source of amyloid beta-peptide in human blood. Biochem Biophys Res Commun. 1995;213(1):96–103.
Evin G, Zhu A, Holsinger RM, Masters CL, Li QX. Proteolytic processing of the Alzheimer’s disease amyloid precursor protein in brain and platelets. J Neurosci Res. 2003;74(4):386–92.
Li QX, Fuller SJ, Beyreuther K, Masters CL. The amyloid precursor protein of Alzheimer disease in human brain and blood. J Leukoc Biol. 1999;66(4):567–74.
Pluta R. Astroglial expression of the beta-amyloid in ischemia–reperfusion brain injury. Ann N Y Acad Sci. 2002;977:102–8.
Burton T, Liang B, Dibrov A, Amara F. Transcriptional activation and increase in expression of Alzheimer’s beta-amyloid precursor protein gene is mediated by TGF-beta in normal human astrocytes. Biochem Biophys Res Commun. 2002;295(4):702–12.
Hartlage-Rubsamen M, Zeitschel U, Apelt J, Gartner U, Franke H, Stahl T, Gunther A, Schliebs R, Penkowa M, Bigl V, Rossner S. Astrocytic expression of the Alzheimer’s disease beta-secretase (BACE1) is stimulus-dependent. Glia. 2003;41(2):169–79.
Craft S, Baker L, Montine T, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment. Arch Neurol. 2012;69(1):29–38.
Delrieu J, Ousset PJ, Vellas B, et al. Gantenerumab for the treatment of Alzheimer’s disease. Expert Opin Biol Ther. 2012;12(8):1077–86.
Ostrowitzki S, Deptula D, Thurfiell L, et al. Mechanism of amyloid removal in patients with Alzheimer’s disease treated with gantenerumab. Arch Neurol. 2012;69(2):198–207.
Mangialasche F, Solomon A, Winblad B, Mecocci P, Kivipelto M. Alzheimer’s disease: clinical trials and drug development. Lancet Neurol. 2010;9(7):702–16. doi:10.1016/S1474-4422(10)70119-8 (Review. Erratum in: Lancet Neurol. 2011;10(6):501).
Boutajangout A, Sigurdsson E, Krishnamurthy P. Tau as a therapeutic target for Alzheimer’s disease. Curr Alzheimer Res. 2011;8(6):666–77.
Smith G, Laxton A, Tang-Wai D, et al. Increased cerebral metabolism after 1 year of deep brain stimulation in Alzheimer disease. Arch Neurol. 2012;69(9):1141-8.
Acknowledgments
Supported by the Banner Sun Health Research Institute, NIA P30 AG 019610 and the Arizona Alzheimer’s Research Consortium.
Disclosures
Camryn Berk has no disclosures relating to this manuscript. Dr Sabbagh receives contract/grant support from Lilly, Avanir, Pfizer, Eisai, Functional Neuromodulation, Genentech, Piramal, Avid and Elan. Dr Sabbagh is an advisor/consultant to Biogen, Piramal and Eisai. Dr Sabbagh receives royalties from Wiley and TenSpeed. Neither author received compensation in the drafting of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berk, C., Sabbagh, M.N. Successes and Failures for Drugs in Late-Stage Development for Alzheimer’s Disease. Drugs Aging 30, 783–792 (2013). https://doi.org/10.1007/s40266-013-0108-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-013-0108-6