Abstract
Background
Root cause analyses show that up to 70 % of adverse events are caused by human error. Strong non-technical skills (NTS) can prevent or reduce these errors, considerable numbers of which occur in the operating theatre. Minimally invasive surgery (MIS) requires manipulation of more complex equipment than open procedures, likely requiring a different set of NTS for each kind of team. The aims of this study were to identify the MIS teams’ key NTS and investigate the effect of training and assessment of NTS on MIS teams.
Methods
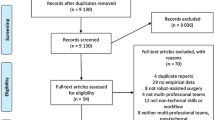
The databases of PubMed, Cochrane Library, Embase, PsycINFO, and Scopus were systematically searched according to Preferred Reporting Item for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Articles containing outcome measures related to MIS teams’ key NTS, training, or assessment of NTS were included.
Results
The search yielded 1984 articles, 11 of which were included. All were observational studies without blinding, and they differed in aims, types of evaluation, and outcomes. Only two studies evaluated patient outcomes other than operative time, and overall, the studies’ quality of evidence was low. Different communication types were encountered in MIS compared to open surgery, mainly due to equipment- and patient-related challenges. Fixed teams improved teamwork and safety levels, while deficient planning and poor teamwork were found to obstruct workflow and increase errors. Training NTS mitigates these issues and improves staff attitudes towards NTS.
Conclusions
MIS teams’ NTS are important for workflow and prevention of errors and can be enhanced by working in fixed teams. In the technological complex sphere of MIS, communication revolves around equipment- and patient-related topics, much more so than in open surgery. In all, only a few heterogeneous-design studies have examined this. In the future, the focus should shift to systematically identifying key NTS and develo** effective, evidence-based team training programmes in MIS.

Similar content being viewed by others
References
Vincent C, Neale G, Woloshynowych M (2001) Adverse events in British hospitals: preliminary retrospective record review. BMJ 322:517–519
de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA (2008) The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care 17:216–223
Gawande AA, Zinner MJ, Studdert DM, Brennan TA (2003) Analysis of errors reported by surgeons at three teaching hospitals. Surgery 133:614–621
Joint Commission on Accreditation of Health Care Organizations Sentinel Event Data Root Causes by Event Type 2004—2Q 2014—Root_Causes_by_Event_Type_2004-2Q_2014.pdf. http://www.jointcommission.org/assets/1/18/Root_Causes_by_Event_Type_2004-2Q_2014.pdf. Accessed 5 Feb 2015
Østergaard D, Dieckmann P, Lippert A (2011) Simulation and CRM. Best Pract Res Clin Anaesthesiol 25:239–249
Greenberg CC, Regenbogen SE, Studdert DM, Lipsitz SR, Rogers SO, Zinner MJ, Gawande AA (2007) Patterns of communication breakdowns resulting in injury to surgical patients. J Am Coll Surg 204:533–540
Calland JF, Guerlain S, Adams RB, Tribble CG, Foley E, Chekan EG (2002) A systems approach to surgical safety. Surg Endosc 16:1005–1014; discussion 1015
Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R (2015) SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc 29:3074–3085
Flin RH, O’Connor P, Crichton M (2008) Safety at the sharp end: a guide to non-technical skills. Ashgate, Burlington
Yule S, Flin R, Maran N, Rowley D, Youngson G, Paterson-Brown S (2008) Surgeons’ non-technical skills in the operating room: reliability testing of the NOTSS behavior rating system. World J Surg 32:548–556
Siu J, Maran N, Paterson-Brown S (2014) Observation of behavioural markers of non-technical skills in the operating room and their relationship to intra-operative incidents. Surg J R Coll Surg Edinb Irel. doi:10.1016/j.surge.2014.06.005
Schiøler T, Lipczak H, Pedersen BL, Mogensen TS, Bech KB, Stockmarr A, Svenning AR, Frølich A, Danish Adverse Event Study (2001) Incidence of adverse events in hospitals. A retrospective study of medical records. Ugeskr Laeger 163:5370–5378
Young-Xu Y, Neily J, Mills PD, Carney BT, West P, Berger DH, Mazzia LM, Paull DE, Bagian JP (2011) Association between implementation of a medical team training program and surgical morbidity. Arch Surg Chic Ill 1960 146:1368–1373
Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH, Mazzia LM, Paull DE, Bagian JP (2010) Association between implementation of a medical team training program and surgical mortality. JAMA 304:1693–1700
McCulloch P, Rathbone J, Catchpole K (2011) Interventions to improve teamwork and communications among healthcare staff. Br J Surg 98:469–479
Gordon M, Darbyshire D, Baker P (2012) Non-technical skills training to enhance patient safety: a systematic review. Med Educ 46:1042–1054
Dedy NJ, Bonrath EM, Zevin B, Grantcharov TP (2013) Teaching nontechnical skills in surgical residency: a systematic review of current approaches and outcomes. Surgery 154:1000–1008
Tan SB, Pena G, Altree M, Maddern GJ (2014) Multidisciplinary team simulation for the operating theatre: a review of the literature. ANZ J Surg 84:515–522
Cumin D, Boyd MJ, Webster CS, Weller JM (2013) A systematic review of simulation for multidisciplinary team training in operating rooms. Simul Healthc J Soc Simul Healthc 8:171–179
Gjeraa K, Møller TP, Østergaard D (2014) Efficacy of simulation-based trauma team training of non-technical skills. A systematic review. Acta Anaesthesiol Scand 58:775–787
Soot SJ, Eshraghi N, Farahmand M, Sheppard BC, Deveney CW (1999) Transition from open to laparoscopic fundoplication: The learning curve. Arch Surg 134:278–281
Hanna GB, Cresswell AB (1960) Cuschieri A (2002) Shadow depth cues and endoscopic task performance. Arch Surg Chic Ill 137:1166–1169
Zheng B, Fung E, Fu B, Panton NM, Swanström LL (2015) Surgical team composition differs between laparoscopic and open procedures. Surg Endosc 29:2260–2265
de Rooij T, Lu MZ, Steen MW, Gerhards MF, Dijkgraaf MG, Busch OR, Lips DJ, Festen S, Besselink MG, Dutch Pancreatic Cancer Group (2016) Minimally Invasive Versus Open Pancreatoduodenectomy: Systematic Review and Meta-analysis of Comparative Cohort and Registry Studies. Ann Surg. doi:10.1097/SLA.0000000000001660
Veldkamp R, Kuhry E, Hop WCJ, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM, COlon cancer Laparoscopic or Open Resection Study Group (COLOR) (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Graafland M, Schraagen JMC, Boermeester MA, Bemelman WA, Schijven MP (2015) Training situational awareness to reduce surgical errors in the operating room. Br J Surg 102:16–23
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R (2010) The impact of stress on surgical performance: a systematic review of the literature. Surgery 147(318–330):e1–e6
Silvennoinen M, Mecklin J-P, Saariluoma P, Antikainen T (2009) Expertise and skill in minimally invasive surgery. Scand J Surg 98:209–213
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Kirkpatrick DL (2005) Evaluating training programs: the four levels, 3rd edn. Berrett-Koehler, San Francisco
Ghaderi I, Manji F, Park YS, Juul D, Ott M, Harris I, Farrell TM (2015) Technical skills assessment toolbox: a review using the unitary framework of validity. Ann Surg 261:251–262
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL, Williams JW, Atkins D, Meerpohl J, Schünemann HJ (2011) GRADE guidelines: 4. Rating the quality of evidence-study limitations (risk of bias). J Clin Epidemiol 64:407–415
Paige JT, Kozmenko V, Yang T, Paragi Gururaja R, Hilton CW, Cohn I, Chauvin SW (2009) High-fidelity, simulation-based, interdisciplinary operating room team training at the point of care. Surgery 145:138–146
Al-Hakim L (2011) The impact of preventable disruption on the operative time for minimally invasive surgery. Surg Endosc 25:3385–3392
Catchpole K, Mishra A, Handa A, McCulloch P (2008) Teamwork and error in the operating room: analysis of skills and roles. Ann Surg 247:699–706
Guerlain S, Adams RB, Turrentine FB, Shin T, Guo H, Collins SR, Calland JF (2005) Assessing team performance in the operating room: development and use of a “black-box” recorder and other tools for the intraoperative environment. J Am Coll Surg 200:29–37
McCulloch P, Mishra A, Handa A, Dale T, Hirst G, Catchpole K (2009) The effects of aviation-style non-technical skills training on technical performance and outcome in the operating theatre. Qual Saf Health Care 18:109–115
Mishra A, Catchpole K, Dale T, McCulloch P (2008) The influence of non-technical performance on technical outcome in laparoscopic cholecystectomy. Surg Endosc 22:68–73
Mishra A, Catchpole K, McCulloch P (2009) The Oxford NOTECHS System: reliability and validity of a tool for measuring teamwork behaviour in the operating theatre. Qual Saf Health Care 18:104–108
Paige JT, Kozmenko V, Yang T, Gururaja RP, Hilton CW, Cohn I, Chauvin SW (2009) Attitudinal changes resulting from repetitive training of operating room personnel using of high-fidelity simulation at the point of care. Am Surg 75:584–590; discussion 590–591
Sevdalis N, Wong HWL, Arora S, Nagpal K, Healey A, Hanna GB, Vincent CA (2012) Quantitative analysis of intraoperative communication in open and laparoscopic surgery. Surg Endosc 26:2931–2938
Stepaniak PS, Heij C, Buise MP, Mannaerts GHH, Smulders JF, Nienhuijs SW (2012) Bariatric surgery with operating room teams that stayed fixed during the day: a multicenter study analyzing the effects on patient outcomes, teamwork and safety climate, and procedure duration. Anesth Analg 115:1384–1392
Zheng B, Martinec DV, Cassera MA, Swanström LL (2008) A quantitative study of disruption in the operating room during laparoscopic antireflux surgery. Surg Endosc 22:2171–2177
Sørensen SMD, Savran MM, Konge L, Bjerrum F (2015) Three-dimensional versus two-dimensional vision in laparoscopy: a systematic review. Surg Endosc. doi:10.1007/s00464-015-4189-7
Mentis HM, Chellali A, Manser K, Cao CGL, Schwaitzberg SD (2015) A systematic review of the effect of distraction on surgeon performance: directions for operating room policy and surgical training. Surg Endosc. doi:10.1007/s00464-015-4443-z
Alarcon A, Berguer R (1996) A comparison of operating room crowding between open and laparoscopic operations. Surg Endosc 10:916–919
Stavroulis A, Cutner A, Liao L-M (2013) Staff perceptions of the effects of an integrated laparoscopic theatre environment on teamwork. Gynecol Surg 10:177–180
Rodrigues SP, Kuile MT, Dankelman J, Jansen FW (2012) Patient safety risk factors in minimally invasive surgery: a validation study. Gynecol Surg 9:265–270
Buljac-Samardzic M, Dekker-van Doorn CM, van Wijngaarden JDH, van Wijk KP (2010) Interventions to improve team effectiveness: a systematic review. Health Policy Amst Neth 94:183–195
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Erwin PJ, Hamstra SJ (2011) Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA 306:978–988
Hull L, Arora S, Symons NRA, Jalil R, Darzi A, Vincent C, Sevdalis N, Delphi Expert Consensus Panel (2013) Training faculty in nontechnical skill assessment: national guidelines on program requirements. Ann Surg 258:370–375
Brunckhorst O, Shahid S, Aydin A, McIlhenny C, Khan S, Raza SJ, Sahai A, Brewin J, Bello F, Kneebone R, Khan MS, Dasgupta P, Ahmed K (2015) Simulation-based ureteroscopy skills training curriculum with integration of technical and non-technical skills: a randomised controlled trial. Surg Endosc 29:2728–2735
Thomas EJ, Sexton JB, Helmreich RL (2003) Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med 31:956–959
Bhangu A, Bhangu S, Stevenson J, Bowley DM (2013) Lessons for surgeons in the final moments of Air France Flight 447. World J Surg 37:1185–1192
Healey AN, Undre S, Vincent CA (2004) Develo** observational measures of performance in surgical teams. Qual Saf Health Care 13(Suppl 1):i33–i40
Undre S, Sevdalis N, Healey AN, Darzi SA, Vincent CA (2006) Teamwork in the operating theatre: cohesion or confusion? J Eval Clin Pract 12:182–189
Hull L, Sevdalis N (2015) Advances in teaching and assessing nontechnical skills. Surg Clin North Am 95:869–884
Acknowledgments
Funding was provided by The Danish Cancer Society (Grant number: R100-A7166).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. René Horsleben Petersen is a compensated speaker for Covidien, Ethicon, Medela, and Takeda. Drs. Kirsten Gjeraa, Lene Spanager, Lars Konge, and Doris Østergaard have no conflicts of interest or financial ties to disclose.
Appendix 1: Search terms and strategy
Appendix 1: Search terms and strategy
#1 | Non-technical |
#2 | Non technical |
#3 | Nontechnical |
#4 | Non-technical skill |
#5 | Non-technical skills |
#6 | Non-technical performance |
#7 | Teamwork |
#8 | Team intervention |
#8 | Team intervention |
#9 | Team interventions |
#10 | Team training |
#11 | Team development |
#12 | Team innovation |
#13 | Team program |
#14 | Team programs |
#15 | Team education |
#16 | Team improvement |
#17 | Team improvements |
#18 | Team improve |
#19 | Team management |
#20 | Crew resource management |
#21 | Crisis resource management |
#22 | Human factor |
#23 | Human factors |
#24 | Behaviour |
#25 | Behavior |
#26 | Behaviours |
#27 | Behaviors |
#28 | Error* |
#29 | Safety |
#30 | Risk assessment |
#31 | Impact prevent* |
#32 | Incident |
#33 | Adverse events |
#34 | Adverse event |
#35 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 |
#36 | Laparoscopy |
#37 | Laparoscopic |
#38 | Mediastinoscopy |
#39 | Mediastinoscopic |
#40 | Thoracoscopy |
#41 | Thoracoscopic |
#42 | Video-assisted surgery |
#43 | Video-assisted surgery |
#44 | Surgical endoscopy |
#45 | Minimal invasive surgery |
#46 | Minimal invasive surgical |
#47 | #36 or #37 or #38 or #39 or #40 or #41 or #43 or #44 or #45 or #46 |
#48 | Team |
#49 | Teams |
#50 | #48 or #49 |
#51 | #35 and #47 and #50 |
Rights and permissions
About this article
Cite this article
Gjeraa, K., Spanager, L., Konge, L. et al. Non-technical skills in minimally invasive surgery teams: a systematic review. Surg Endosc 30, 5185–5199 (2016). https://doi.org/10.1007/s00464-016-4890-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4890-1