Abstract
Background
Undeniably, robotic-assisted surgery (RAS) has become very popular in recent decades, but it has introduced challenges to the workflow of the surgical team. Non-technical skills (NTS) have received less emphasis than technical skills in training and assessment. The systematic review aimed to update the evidence on the role of NTS in robotic surgery, specifically focusing on evaluating assessment tools and their utilisation in training and surgical education in robotic surgery.
Methods
A systematic literature search of PubMed, PsycINFO, MEDLINE, and EMBASE was conducted to identify primary articles on NTS in RAS. Messick’s validity framework and the Modified Medical Education Research Study Quality Instrument were utilised to evaluate the quality of the validity evidence of the abstracted articles.
Results
Seventeen studies were eligible for the final analysis. Communication, environmental factors, anticipation and teamwork were key NTS for RAS. Team-related factors such as ambient noise and chatter, inconveniences due to repeated requests during the procedure and constraints due to poor design of the operating room may harm patient safety during RAS. Three novel rater-based scoring systems and one sensor-based method for assessing NTS in RAS were identified. Anticipation by the team to predict and execute the next move before an explicit verbal command improved the surgeon’s situational awareness.
Conclusion
This systematic review highlighted the paucity of reporting on non-technical skills in robotic surgery with only three bespoke objective assessment tools being identified. Communication, environmental factors, anticipation, and teamwork are the key non-technical skills reported in robotic surgery, and further research is required to investigate their benefits to improve patient safety during robotic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Undeniably robotic-assisted surgery (RAS) has become very popular in recent decades. So far, over 7.2 million RAS procedures have been performed by 2019 since the US Food and Drug Association (FDA) approval in 2000 [1]. In all the commercially available RAS systems today, the surgeon is physically disconnected from the patient and the rest of the surgical team, which is very different from the traditional operating theatre (OR) setup, and this has introduced several challenges to how surgeons and their teams’ function, especially to communication, teamwork and situational awareness. On certain platforms, the robotic surgeon may be working several meters away from the patient, which potentially places considerable limitations on their interactions with OR team. Moreover, robotic system components have a considerable footprint and can restrict movement and obstruct the direct line of sight between team members [2]. The immersive environment of the RAS inadvertently affects the surgeon’s situational awareness, which could negatively impact the surgeon’s decision-making [3] and preclude effective communication between operating staff.
Ever since a report by the Institute of Medicine in 1999 highlighting human errors and their consequences in healthcare, Non-Technical Skills (NTS) have been identified as an essential pillar of patient safety [4]. Studies suggest that up to 60% of surgical patients may be involved in adverse events and breakdown in communication was the cause of 43% of errors during surgery [5]. Flin et al. defined NTS as ‘the cognitive, social and personal resource skills that complement technical skills, and contribute to safe and efficient task performance [6]. While there has been a great emphasis on training, assessment and credentialling of surgeons’ technical competencies in RAS, Non-Technical Skills (NTS) have received less emphasis [7]. As with the introduction of any new medical technology, it is crucial to understand NTS specific to RAS and the state of NTS training for RAS teams. Particular emphasis should focus on preventing errors and response to emergency situations including device malfunction, major haemorrhage or air embolism which may require rapid conversion to open surgery.
In 2019, Kwong et al. reported a systematic review to understand NTS in RAS and how it could be assessed [8]. This review however was limited to robotic urological surgery and highlighted the paucity of tools available for assessing NTS in RAS, and most of them were not specific to robotics. Another older review identified key NTS and their assessment in minimally invasive surgery (MIS) teams but did not include RAS teams [9]. A recently published review by Cha et al. identified objective metrics for measurement in the surgical environment, including RAS, but focusing only on the physiological matrix without assessing NTS [10].
This systematic review aimed to update the evidence on the role of NTS in robotic surgery with a specific focus on evaluating assessment tools and their utilisation in training and surgical education in robotic surgery.
Methods
A systematic literature review was performed as per the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) Guidelines [11]. The study has been registered with Research Registry, identification number: review registry 1654.
Eligibility criteria
The PICOS (Population, Intervention, Comparator, Outcomes and Setting) framework was used to create a well-formulated research question to guide the systematic review (Table 1).
Studies written in the English language involving the identification, assessment or training of NTS skills in individuals and teams during live or simulated RAS procedures were included in the review. Study types included cross-sectional, cohort, qualitative studies, non-randomised and randomised control trials.
Minimally invasive surgery other than RAS, robotic surgery without general anaesthesia (as they would not involve the entire team) and studies solely on the evaluation of technical skills, were excluded. Articles without empirical evidence, abstracts without full-text articles, duplicate publications and articles without an English translation were also excluded from the review.
A search of the PubMed, PsychINFO, Medline and Embase databases was conducted in December 2022. Studies up to 1985 were included when a robot was first used in a surgical procedure [12]. Key concepts used in the search were ‘Non-Technical Skills’, ‘Robotic Surgery’, ‘Subjective Assessment’, ‘Objective Assessment’, ‘Robotic Surgery Team’ and ‘Outcome’. Table 2 shows the search terms and strategy used.
Screening
Two independent reviewers searched the databases, selected titles, reviewed abstracts and short-listed studies which met the inclusion criteria. Any disagreements during study selection were resolved by consensus between the two reviewers.
Full-text review of all the studies which meet met the inclusion criteria were reviewed independently by both reviewers and data extracted. The following data fields were extracted:
-
1.
Study characteristics—Authors, year, single or multi-centre, registration/ID, country, name of article, study design, meets the inclusion criteria (yes/no), study setting (dry simulation lab, wet simulation lab, simulated OR, intra-operative), the total number of participants, participant level of experience (Novice, Intermediate, Expert, Unspecified), study funding sources and possible conflicts of interest of the authors.
-
2.
Evaluation and outcome characteristics—Name of the assessment tool, type (subjective or objective), NTS domain or construct tested, evaluator type (Self-rated, Novice, Expert, Crowd-sourced, Not applicable/ other), the content of the intervention, duration, intensity and timing, effects of NTS training/ assessment on staff’s knowledge, attitude, behaviour and patient outcomes.
Data analysis and quality of literature and validity evidence
-
1.
Selected articles were judged on their level of evidence using the OCEBM (Modified Oxford Centre for Evidence-Based Medicine) Working Group Level of Evidence [13].
-
2.
MMERSQI (Modified Medical Education Research Study Quality Instrument) was used to appraise the methodological quality of the studies. Studies have scored a minimum of 23.5 and a maximum of 100 based on 12 outcomes based on the domains of design, sampling, setting, type of data, the validity of assessment, data analysis and outcomes [14].
-
3.
Validity of the judgements made by different NTS assessment tools was evaluated using Messick’s validity framework [15]. Validity evidence was categorised into content, response process, internal consistency, relationship to other variables and consequences [15].
Data management: Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia, a. Available at www.covidence.org was used for deduplication, screening, full-text review, and data extraction. The data synthesised here was then exported to Excel files.
Results
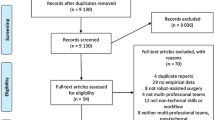
The search databases yielded 27,824 studies, and seven more were added manually. 17 studies met the inclusion criteria and were fully analysed (PRISMA diagram—Fig. 1).
Twelve were cohort studies; two were cross-sectional studies (surveys), one was a qualitative study (focussed interviews), one was a randomised control trial (RCT), and another involved multiple methods. Eight were performed in a live operating room (OR), seven in a simulated OR and one was performed in a simulation lab using a dry model. Seven of the eight studies performed in the live OR were based on urological procedures, one was performed on gynaecological procedures and in two studies observations included general and colorectal surgeries. In four studies, participants were all experts, two involved only novices, six involved participants with different levels of experience (novice, intermediate and expert), and the experience level was unspecified in five studies (Table 3).
Domains of non-technical skills
Cognitive load
Four studies reported on the use of NASA-TLX (National Aeronautics and Space Administration-Task Load Index) to assess cognitive workload across multiple professions [16,17,18,19,3], therefore, representing potential novel challenges or resolutions to effective NTS. RAS is a highly complex environment; hence it is essential to evaluate the NTS of the entire multi-professional team comprehensively [29].
Limitations of this systematic review include the possibility of missing some unpublished literature and 31 articles were removed as the full text was unavailable. A search of the “grey” literature was not performed due to the large number of titles for screening and time constraints. As a result, publication bias could not be convincingly excluded. Further examination into the implementation of sensor-based measurements utilising distinct physiological parameters with increasingly miniaturised measurement devices will provide a more objective and immediate assessment of NTS. Progression in the design of systems and instruments will facilitate communication between the surgeon and the rest of the team, promoting the formation of a shared mental model during the procedure. The development of telesurgery necessitates the formation of a global, high-fidelity, emergency robotic undocking curriculum, akin to the ATLS (Advanced Trauma Life Support) [34]. Investigating the most advantageous theatre design and set-up, which can diminish crowding and enhance productivity (Refer Fig. 2—Key takeaway).
Conclusion
This systematic review has highlighted multiple non-technical skills tools, with three main ones, most of which are under evaluated. Whilst promising, increased awareness and widespread use across multiple specialities is lacking. Further evaluative research is required to report on incorporating non-technical skills training and assessment in robotic surgery curricula, to demonstrate the potential benefits and improve patient safety in robotic surgery.
References
Koukourikis P, Rha KH (2021) Robotic surgical systems in urology: What is currently available? Investig Clin Urol 62(1):14
Kanji F, Catchpole K, Choi E, Alfred M, Cohen K, Shouhed D, Anger J, Cohen T (2021) Work-system interventions in robotic-assisted surgery: a systematic review exploring the gap between challenges and solutions. Surg Endosc 35:1976–1989
Randell R, Honey S, Alvarado N, Pearman A, Greenhalgh J, Long A, Gardner P, Gill A, Jayne D, Dowding D (2016) Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cogn Technol Work 18:423–437
Kohn LT, Kohn LT, Corrigan JM, Donaldson MS et al (eds) (2000) To Err is human: building a safer health system. National Academies Press, US
Gawande AA, Zinner MJ, Studdert DM, Brennan TA (2003) Analysis of errors reported by surgeons at three teaching hospitals. Surgery 133(6):614–621
Flin RH, O’Connor P, Crichton M (2008) Safety at the sharp end: a guide to non-technical skills. Ashgate Publishing, London
Chen R, Rodrigues Armijo P, Robotic KC, Task Force SAGES, Siu KC, Oleynikov D (2020) A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc 34(1):361–367
Kwong JC, Lee JY, Goldenberg MG (2019) Understanding and assessing nontechnical skills in robotic urological surgery: a systematic review and synthesis of the validity evidence. J Surg Educ 76(1):193–200
Gjeraa K, Spanager L, Konge L, Petersen RH, Østergaard D (2016) Non-technical skills in minimally invasive surgery teams: a systematic review. Surg Endosc 30:5185–5199
Cha JS, Yu D (2022) Objective measures of surgeon non-technical skills in surgery: a sco** review. Hum Factors 64(1):42–73
Moher D, Liberati A, Tetzlaff J, Altman DG et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269
Leal Ghezzi T, Campos Corleta O (2016) 30 years of robotic surgery. World J Surg 40(10):2550–2557. https://doi.org/10.1007/s00268-016-3543-9
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H (2011) The 2011 Oxford CEBM evidence levels of evidence (introductory document). Oxford Center for Evidence Based Medicine
Al Asmri M, Haque MS, Parle J (2023) A Modified Medical Education Research Study Quality Instrument (MMERSQI) developed by Delphi consensus. BMC Med Educ 23(1):1–8
Messick S (1994) Validity of psychological assessment: validation of inferences from persons’ responses and performances as scientific inquiry into score meaning. ETS Research Report Series 1994(2):i–28
Klein MI, Lio CH, Grant R, Carswell CM, Strup S (2009) A mental workload study on the 2d and 3d viewing conditions of the da Vinci surgical robot. Proc Human Factors Ergonom Soc Annu Meet 53(18):1186–1190
Ahmed Y, Lone Z, Hussein AA, Feng Y, Khan H, Broad S, Kannappan R, Skowronski A, Cole A, Wang D, Stone K (2019) Do surgeon non-technical skills correlate with teamwork-related outcomes during robot-assisted surgery? BMJ Lead 3:69–74
Sexton K, Johnson A, Gotsch A, Hussein AA, Cavuoto L, Guru KA (2018) Anticipation, teamwork and cognitive load: chasing efficiency during robot-assisted surgery. BMJ Qual Saf 27(2):148–154
AlJamal YN, Baloul MS, Mathis KL, Dozois EJ, Kelley SR (2021) Evaluating non-operative robotic skills in colorectal surgical training. J Surg Res 260:391–398
Norasi H, Tetteh E, Law KE, Ponnala S, Hallbeck MS, Tollefson M (2022) Intraoperative workload during robotic radical prostatectomy: comparison between multi-port da Vinci ** and single port da Vinci SP robots. Appl Ergon. https://doi.org/10.1016/j.apergo.2022.103826
Hart SG (2006) NASA-task load index (NASA-TLX); 20 years later. Proc Human Factors and Ergonom Soc Annu Meet 50(9):904–908
Boles DB, Bursk JH, Phillips JB, Perdelwitz JR (2007) Predicting dual-task performance with the Multiple Resources Questionnaire (MRQ). Hum Factors 49(1):32–45
Tiferes J, Hussein AA, Bisantz A, Kozlowski JD, Sharif MA, Winder NM, Ahmad N, Allers J, Cavuoto L, Guru KA (2016) The loud surgeon behind the console: understanding team activities during robot-assisted surgery. J Surg Educ 73(3):504–512
Schiff L, Tsafrir Z, Aoun J, Taylor A, Theoharis E, Eisenstein D (2016) Quality of communication in robotic surgery and surgical outcomes. JSLS. https://doi.org/10.4293/JSLS.2016.00026
Onofrio R, Trucco P (2020) A methodology for dynamic human reliability analysis in robotic surgery. Appl Ergon. https://doi.org/10.1016/j.apergo.2020.103150
Zattoni F, Guttilla A, Crestani A, De Gobbi A, Cattaneo F, Moschini M, Vianello F, Valotto C, Dal Moro F, Zattoni F (2015) The value of open conversion simulations during robot-assisted radical prostatectomy: implications for robotic training curricula. J Endourol 29(11):1282–1288
Melnyk R, Saba P, Holler T, Cameron K, Mithal P, Rappold P, Wu G, Cubillos J, Rashid H, Joseph JV, Ghazi AE (2022) Design and implementation of an emergency undocking curriculum for robotic surgery. Simul Healthc 17(2):78–87
Raison N, Wood T, Brunckhorst O, Abe T, Ross T, Challacombe B, Khan MS, Novara G, Buffi N, Van Der Poel H, McIlhenny C (2017) Development and validation of a tool for non-technical skills evaluation in robotic surgery—the ICARS system. Surg Endosc 31:5403–5410
Schreyer J, Koch A, Herlemann A, Becker A, Schlenker B, Catchpole K, Weigl M (2022) RAS-NOTECHS: validity and reliability of a tool for measuring non-technical skills in robotic-assisted surgery settings. Surg Endosc 36:1916–1926
Manuguerra A, Mazeaud C, Hubert N, Eschwège P, Roumiguié M, Salleron J, Hubert J (2021) Non-technical skills in robotic surgery and impact on near-miss events: a multi-center study. Surg Endosc 35:5062–5071
Cha JS, Athanasiadis DI, Peng Y, Wu D, Anton NE, Stefanidis D, Yu D (2022) Objective nontechnical skills measurement using sensor-based behavior metrics in surgical teams. Hum Factors. https://doi.org/10.1177/00187208221101292
Szold A, Bergamaschi R, Broeders I, Dankelman J, Forgione A, Langø T, Melzer A, Mintz Y, Morales-Conde S, Rhodes M, Satava R (2015) European Association of Endoscopic Surgeons (EAES) consensus statement on the use of robotics in general surgery. Surg Endosc 29:253–288
Zattoni F, Morlacco A, Cattaneo F, Soligo M, Meggiato L, Modonutti D, Valotto C, Dal Moro F, Zattoni F (2017) Development of a surgical safety training program and checklist for conversion during robotic partial nephrectomies. Urology 109:38–43
Carmont M (2005) The advanced trauma life support course: a history of its development and review of related literature. Postgrad Med J 81(952):87
Myklebust MV, Storheim H, Hartvik M, Dysvik E (2020) Anesthesia professionals’ perspectives of teamwork during robotic-assisted surgery. AORN J 111(1):87–96
Raison N, Ahmed K, Abe T, Brunckhorst O, Novara G, Buffi N, McIlhenny C, van der Poel H, van Hemelrijck M, Gavazzi A, Dasgupta P (2018) Cognitive training for technical and non-technical skills in robotic surgery: a randomised controlled trial. BJU Int 122(6):1075–1081
Acknowledgements
This research was undertaken as part of the third year of the MSc in PSCHF.
Funding
None received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Vimaladhithan Mahendran, Laura Turpin, Matthew Boal and Nader K. Francis have no conflict of interests or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahendran, V., Turpin, L., Boal, M. et al. Assessment and application of non-technical skills in robotic-assisted surgery: a systematic review. Surg Endosc 38, 1758–1774 (2024). https://doi.org/10.1007/s00464-024-10713-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10713-1