Abstract
Purpose
Magnetic resonance imaging (MRI) signal intensity is correlated to structural postoperative changes of the anterior cruciate ligament (ACL) autograft. The purpose of this study was to investigate the ACL autograft maturation process via MRI over 2 years postoperatively, compare it to a native ACL signal and correlate the results with clinical outcome, return to preinjury sports levels, and knee laxity measurements.
Methods
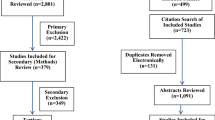
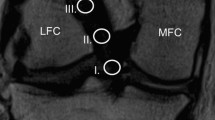
ACL autograft signal intensity was measured in 17 male patients (age, 28.3 ± 7.0 years) who underwent ACL reconstruction with hamstring autograft at 6 weeks, 3-, 6-, 12-, and 24 months postoperatively by 3 Tesla MRI. Controls with an intact ACL served as control group (22 males, 8 females; age, 26.7 ± 6.8 years). An ACL/PCL ratio (APR) and ACL/muscle ratio (AMR) was calculated to normalize signals to soft tissue signal. APR and AMR were compared across time and to native ACL signal. Clinical outcome scores (IKDC, Lysholm), return to preinjury sports levels (Tegner activity scale), and knee laxity measurement (KT-1000) were obtained and correlated to APR and AMR at the respective time points.
Results
The APR and AMR of the ACL graft changed significantly from the lowest values at 6 weeks to reach the highest intensity after 6 months (p < 0.001). Then, the APR and AMR were significantly different from a native ACL 6 months after surgery (p < 0.01) but approached the APR and AMR of the native ACL at 1- and 2 years after surgery (p < 0.05). The APR changed significantly during the first 2 years postoperatively in the proximal (p < 0.001), mid-substance (p < 0.001), and distal (p < 0.01) intraarticular portion of the ACL autograft. A hypo-intense ACL MRI signal was associated with return to the preinjury sports level (p < 0.05). No correlation was found between ACL MRI graft signal and clinical outcome scores or KT-1000 measurements.
Conclusion
ACL grafts undergo a continuous maturation process in the first 2 years after surgery. The ACL graft signals became hyper-intense 6 months postoperatively and approximated the signal of a native intact ACL at 12- and 24 months. Patients with a hypo-intense ACL graft signal at 2 years follow-up were more likely to return to preinjury sports levels. The results of the present study provide a template for monitoring the normal ACL maturation process via MRI in case of prolonged clinical symptoms. However, subjective outcome and clinical examination of knee laxity remain important to assess the treatment success and to allow to return to sports.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction aims to restore knee stability and regain normal knee function. This allows safe return to activity and reduce the risk of re-injuries. Despite advances in surgical techniques, early ACL re-tears are still a major concern [30, 32, 37]. One reason for early re-ruptures is biological failure due to the remodelling process [29]. The graft maturation process (also known as ligamentization) during the early postoperative phase negatively affects the biomechanical properties of the graft [36, 41, 46]. The decrease of mechanical strength during the first period is of clinical importance as it puts the graft at risk of not meeting its demands [2, 18, 21, 23, 40, 46, 47]. Hence, assessing ACL graft maturity before returning to sports is of high clinical interest and magnetic resonance imaging (MRI) has been shown to be a feasible option [11, 12]. Animal models showed that MRI signal intensity is significantly correlated to structural properties of the ACL graft [5, 46]. A high signal intensity on MRI has been linked to decreased mechanical properties such as low load to failure [46]. In recent years, several MRI studies showed that signal intensity changes of the ACL graft are correlated with the progress of graft maturation in human patients [9, 11, 27, 43]. ACL graft MRI signal intensity increases during the first 6 months followed by a subsequent decline [Full size image
The proximal ACL graft underwent a significant MRI signal change from 6 weeks to 6 months after surgery and showed the highest signal intensity at this time point (p < 0.001). The APR subsequently declined to approximate the APR of a native proximal ACL at 1 and 2 years. The proximal APR was significantly lower than a native ACL at 6 weeks (p < 0.001) and higher at 6 months (p < 0.05) after surgery.
Similarly, the APR of the mid-substance ACL graft ran through a significant transformation from 6 weeks to 2 years postoperatively. While the APR 6 months after ACL-R is significantly different from a native mid-substance ACL (p < 0.01), the APR after 1 and 2 years showed a similar MRI signal compared with a native ACL.
APR of the distal section of the ACL graft showed a significant rise within the first 6 months postoperatively (p < 0.05) before drop** gradually at 1 and 2 years. The APR of distal section of the ACL autograft was significantly lower than the native ACL at all time points except from 6 months postoperatively (all p < 0.01).
AMR measurements
The AMR of the ACL autograft over the postoperative period is shown in Fig. 2B. The AMR changed significantly at the proximal (p < 0.001), mid-substance (p < 0.001), and distal (p < 0.05) part of the ACL graft.
AMR of the proximal ACL portion rose significantly from 6 weeks to 6 months (p < 0.001) after surgery and was by then significantly different to a native ACL (p < 0.001). Subsequently, the AMR started to decline to reach a similar AMR of the native proximal ACL at 1 and 2 years.
The mid-substance AMR increased significantly from 6 weeks to 6 months postoperatively (p < 0.001) before decreasing at 1 year and 2 years postoperatively (p < 0.01). The AMR was significant higher at 3- and 6 months after ACL-R compared with a native ACL (p < 0.001) but was not different from a native mid-substance ACL at 1 and 2 years.
The distal AMR rose significantly between 6 weeks and 6 months postoperatively (p < 0.05). It then dropped slowly to the lowest AMR at 2 years postoperatively. AMR of the distal intraarticular graft section was significantly lower than a native ACL at 2 years after surgery (p < 0.05, Fig. 3).
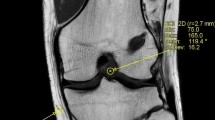
The maturation process of the anterior cruciate ligament autograft exhibits a significant MRI signal change from hypo-intense at (A) 6 weeks postoperatively to more hyper-intense at (B) 3- and (C) 6-months after ACL-R indicating greater disorganization of collagen tissue and higher water content. The MRI signal intensity decreases thereafter at (D) 1- and (E) 2-years post ACL reconstruction to approximate the signal of a native ACL (F). The distal native ACL revealed a more hyper-intense signal compared to the proximal and mid-substance ACL
Correlation to clinical outcome, knee stability, and return to sports
Anterior knee laxity measured by KT-1000 device was 1.9 ± 1.7 mm and 2.4 ± 2.3 mm higher compared to the healthy contralateral knee at 1 and 2 years postoperatively, respectively. For neither APR nor AMR a significant correlation with KT-1000 measurements at the respective time points could be identified.
IKDC and Lysholm score improved significantly from preoperative values to postoperative values at 6 months, 1-, and 2 years postoperatively (all p < 0.001, Fig. 4). There was also a significant increase in clinical outcome scores between 6 months and 1 year postoperatively but not from 1 to 2 years (IKDC: p < 0.001, Lysholm score p < 0.05). APR and AMR were not associated with IKDC and Lysholm score at any time point.
Return to preinjury sports levels
94% (16/17) of the patients returned to sports within 2 years after ACL-R. One patient suffered a contralateral ACL injury 1.5 years after initial ACL-R and could therefore not RTS at final follow-up. Median TAS was 6 (range 4–9) before injury, 4 (range 3–6) after 6 months, 5 (range 1–7) after 1 year and 6 (range 1–9) at final follow up. At 1 year and 2 years follow-up, 41% (7/17 patients) and 65% (11/17) achieved the preinjury TAS level, respectively. TAS was not correlated with APR or AMR at any time point within the small patients’ cohort. However, APR and AMR of the ACL mid-substance were significantly lower (hypo-intense) in patients who could return to the preinjury sports level compared to those who did not achieve the same sports level (p < 0.05).