Abstract
Aims/hypothesis
Ethnicity and gestational diabetes mellitus (GDM) are both risk factors for the development of type 2 diabetes. However, it is uncertain whether ethnicity modifies the effect of GDM on diabetes risk. We aimed to determine the risk of diabetes following pregnancy with and without GDM for Chinese and South Asian women compared with white women.
Methods
Using healthcare databases, all 1,050,108 women aged 20–49 with live births between January 1995 and June 2008 in Ontario were identified. They were followed for up to 15 years for the diagnosis of diabetes.
Results
The age-standardised prevalences of GDM were 4.1%, 7.1% and 2.9% for Chinese, South Asian and white women, respectively. The cumulative incidence of diagnosed diabetes at the median follow-up time of 7.6 years was 16.5% and 1.8% for Chinese women with and without GDM, 31.8% and 3.6% for South Asian women with and without GDM, and 25.7% and 1.8% for white women with and without GDM. The presence of GDM conferred an increase in the risk for diabetes after pregnancy of more than 13-fold in white women, but only a nine- to tenfold increase among Chinese and South Asian women.
Conclusions/interpretation
Although one-third of South Asian women with GDM were diagnosed with diabetes within 8 years postpartum, the incremental impact of GDM on diabetes risk was not as strong among Chinese and South Asian women as it was among white women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM) is defined as an abnormal carbohydrate tolerance diagnosed or first recognised in pregnancy, and it affects between 2% and 7% of pregnant women [1, 2]. This antepartum glucose intolerance is a marker of insulin resistance that can persist into the postpartum period [3, 4], and increases the risk of develo** type 2 diabetes [5, 6].
While ethnicity is another well-recognised risk factor for type 2 diabetes [7–10], less is known about its role in GDM. A 1992 US study showed that white women had a lower prevalence of GDM than all other racial groups [11]. More recent data have corroborated this observation [12–14]. Furthermore, there are data suggesting that women from some minority groups may be at increased risk of glucose intolerance or diabetes following pregnancy complicated by GDM [15–17]. However, these earlier studies were small, and they did not include patients without GDM, so whether the observed ethnic differences in diabetes risk after GDM differed from baseline ethnic differences in diabetes risk could not be evaluated. One recent study examined 13,000 Californian women with GDM, and found marked variation between ethnic groups in diabetes incidence, ranging from 15.8 per 1,000 person-years in white women to 29.0 per 1,000 person-years in black women [18]. Notably, this study did not disaggregate Asian populations, despite the known heterogeneity in diabetes risk in Asian subgroups [19, 20].
The two largest minority ethnic groups in Canada are Chinese (people with Chinese, Hong Kong or Taiwanese ancestry) and South Asians (people with Indian [subcontinent] ancestry) [21]. Two-stage universal screening for GDM is recommended for all pregnant women by Canadian clinical practice guidelines [22]. The objective of this study was to determine whether the incremental impact of GDM on the risk for subsequent diabetes after pregnancy differed between Chinese and South Asian women compared with white women. We hypothesised that minority ethnicity and GDM would act synergistically as risk factors for incident diabetes after pregnancy.
Methods
Study design and data sources
We conducted a population-based cohort study using healthcare databases from the government-funded health insurance programme of the Ontario Ministry of Health and Long-Term Care. This programme is available to all permanent residents of Ontario, Canada's most populous and most ethnically diverse province. These databases include hospital-discharge data, which provide detailed information on all hospitalisations in the province, and the Registered Persons Database, which includes demographic information on all Ontario residents. We also used the Ontario Diabetes Database (ODD), a validated registry of all people diagnosed with non-gestational diabetes in Ontario, derived from healthcare databases [23]. Though the database cannot distinguish between types of diabetes, most incident diabetes in this age group would be of type 2 diabetes. Individuals are linked between these databases and across time by their unique health card number.
Study population
All women aged 20–49 years with in-hospital live births between 1 January 1995 and 30 June 2008 were identified. For women with multiple deliveries during the study period, one delivery was selected at random as the index delivery. Women with pre-existing diabetes were excluded. Women were defined as having GDM if diabetes was coded on the hospitalisation record for the delivery.
Measured baseline characteristics were age at delivery, socioeconomic status (measured ecologically as the neighbourhood household income, divided into province-wide quintiles), the presence of chronic comorbidities (measured using the Charlson comorbidity index) [24], urban vs rural residence, antenatal ambulatory visits with an obstetrician, and ambulatory visits with a primary care physician in the 2 years preceding delivery (as a baseline measure of intensity of health service use). Women with missing address information, for whom some of these baseline characteristics could not be determined, were excluded.
The cohort was subdivided based on ethnicity. As there are no ethnic identifiers in Canadian healthcare data, assignment of people to Chinese and South Asian ethnic groups was based on their surnames, using two lists of surnames validated to identify people with Chinese and South Asian origins in Ontario [25]. Both lists demonstrate excellent positive predictive values when compared with self-reported ethnicity (91.9% for Chinese and 89.3% for South Asian) [25]. Women whose surnames were not on either list were defined as white, as whites make up approximately 87% of the non-Chinese/non-South Asian population of Ontario [21].
Outcome of interest and statistical analysis
Both crude and age-standardised prevalences of GDM were determined for each population.
The primary outcome of interest was diagnosis of diabetes after pregnancy, determined by entry into the ODD postpartum. All women were followed until 31 March 2010. Cumulative incidence curves were constructed for diagnosed diabetes after pregnancy, stratified by ethnic group and by GDM status. Cox proportional hazards regression models were fitted in which individuals were censored at death: both an unadjusted model and a model adjusting for age, socioeconomic status and comorbidity. The independent variables of interest were GDM status and ethnicity. An interaction term between GDM status and ethnicity was included to test for effect modification. The assumption of proportionality was confirmed for all models by plotting log(−log[survival]) vs log(time) to assess parallelism.
All statistical analyses were performed using SAS version 9.2.
Ethics approval
The study was approved by the Research Ethics Board of Sunnybrook Health Sciences Centre, Toronto, ON, Canada.
Results
There were 1,069,098 women with live births during the study period. Of these, 14,591 (1.4%) were excluded because of pre-existing diabetes, and a further 4,399 (0.4%) were excluded because of missing address information. The baseline characteristics of the final 1,050,108 individuals are shown in Table 1.
GDM occurred in 33,203 (3.2%) pregnancies. The crude prevalence of GDM was higher for both minority groups: 5.0% for Chinese and 6.5% for South Asian compared with 2.9% for white women. When standardised for age, the prevalence of GDM among Chinese women was attenuated but remained higher than in white women (4.1%; 95% CI 3.9%, 4.3%; p < 0.0001), whereas the age-standardised prevalence of GDM among South Asian women was even higher than the crude prevalence (7.1%; 95% CI 6.8%, 7.4%; p < 0.0001 vs white women).
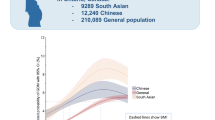
Diabetes was diagnosed in 30,234 of the women in the cohort: 7,755 of the women with GDM at index (39.8 cases per 1,000 person-years), and 22,479 of the women without GDM (2.8 cases per 1,000 person-years). Incidence rates were 2.7, 5.3 and 2.7 cases per 1,000 person-years for Chinese, South Asian and white women without GDM, respectively, and 25.8, 54.7 and 39.7 cases per 1,000 person-years for Chinese, South Asian and white women with GDM, respectively. The cumulative incidence of diagnosed diabetes after pregnancy is shown in Fig. 1. At the median follow-up time of 7.6 years, 1.8% of Chinese women, 3.6% of South Asian women and 1.8% of white women without GDM were diagnosed with diabetes, compared with 16.5% of Chinese women, 31.8% of South Asian women and 25.7% of white women with GDM.
Both GDM status and ethnicity were independently associated with diabetes diagnosis in the Cox proportional hazard models, and a statistically significant interaction term between the two indicated that effect modification was present. Table 2 shows the HRs and 95% CIs for specific comparisons of interest from both the unadjusted and adjusted models. Compared with white women with GDM, Chinese women with GDM were at decreased risk of being diagnosed with diabetes, whereas South Asian women with GDM were at increased risk. When compared with their counterparts without GDM, white women with GDM were at greater risk of being diagnosed with diabetes (adjusted HR 13.6; 95% CI 13.2, 14.0) than either Chinese women with GDM (adjusted HR 9.2; 95% CI 8.1, 10.3) or South Asian women with GDM (adjusted HR 9.6; 95% CI 8.8, 10.5).
Discussion
In this large population-based study of over 1 million women followed for up to 15 years, we observed ethnic differences in the prevalence of GDM and in the incremental impact of GDM on the risk of diabetes after pregnancy. The age-adjusted prevalence of GDM was 41% higher among Chinese and 145% higher among South Asians compared with white women. Among women with GDM, incident diabetes increased most rapidly in the first 4 to 6 months postpartum, with many of these cases probably representing previously undiagnosed type 2 diabetes that was first recognised during screening in pregnancy. Of note, previous data have shown that undiagnosed diabetes is not associated with minority ethnicity in Canada [26], so it is unlikely to bias the results. South Asians with GDM had the greatest risk of being subsequently diagnosed with diabetes, with a cumulative incidence of 50% by 12.5 years postpartum. In contrast, despite having a higher prevalence of GDM than white women, Chinese women with GDM had a lower risk of being diagnosed with diabetes after pregnancy, suggesting that the metabolic abnormalities and insulin resistance leading to GDM in Chinese women are unique to pregnancy and do not persist postpartum to the same degree as in white women. In fact, notwithstanding the differences in the absolute risk, the relative incremental impact of GDM on future diabetes risk was lower among both minority groups than in white women: the presence of GDM in the index pregnancy led to a >13-fold increase in the risk of a subsequent diagnosis of diabetes for white women, but conferred only a nine- to tenfold increase in risk for both Chinese and South Asian women.
This study confirms the results of two prior population-based studies that showed that Chinese and South Asian women have a higher prevalence of GDM than white women. A large Australian study demonstrated that women born in East or South Asia had an increased risk of develo** GDM relative to women born in Australia (ORs 3.2 and 4.2, respectively) [27]. Similarly, a smaller study in New York City demonstrated an increased risk of GDM among virtually all minority populations compared with whites, including an adjusted relative risk of 2.3 for Chinese women and 4.7 for South Asian women [28]. The high risk of subsequent diabetes after GDM among South Asians has been previously described in a small UK study, where the cumulative diabetes incidence at 4.4 years after pregnancy was 49% among South Asians but only 25% among whites [17]. Other studies have similarly described ethnic variation in the risk of subsequent diabetes after GDM [6, 37–39]. This study suggests that ethnic-specific thresholds for the diagnosis of GDM may be needed to more accurately reflect differences in the risk of diabetes and to help identify those patients requiring more intensive follow-up and intervention postpartum.
Abbreviations
- GDM:
-
Gestational diabetes mellitus
- ODD:
-
Ontario Diabetes Database
References
Jovanovic L, Pettitt DJ (2001) Gestational diabetes mellitus. JAMA 286:2516–2518
Ferrara A (2007) Increasing prevalence of gestational diabetes mellitus. Diabetes Care 30:S141–S146
Catalano PM, Huston L, Amini SB, Kalhan SC (1999) Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. Am J Obstet Gynecol 180:903–916
Homko C, Sivan E, Chen X, Reece EA, Boden G (2001) Insulin secretion during and after pregnancy in patients with gestational diabetes mellitus. J Clin Endocrinol Metab 86:568–573
Feig DS, Zinman B, Wang X, Hux JE (2008) Risk of development of diabetes mellitus after diagnosis of gestational diabetes. CMAJ 179:229–234
Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 25:1862–1868
Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27:1047–1053
Anand SS, Yusuf S, Vuksan V et al (2000) Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet 356:279–284
Narayan KMV, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF (2003) Lifetime risk for diabetes mellitus in the United States. JAMA 290:1884–1890
Creatore MI, Moineddin R, Booth G et al (2010) Age- and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. CMAJ 182:781–789
Berkowitz GS, Lapinski RH, Wein R, Lee D (1992) Race/ethnicity and other risk factors for gestational diabetes. Am J Epidemiol 135:965–973
Ferrara A, Kahn HS, Quesenberry CP, Riley C, Hedderson MM (2004) An increase in the incidence of gestational diabetes mellitus: Northern California, 1991–2000. Obstet Gynecol 103:526–533
Lawrence JM, Contreras R, Chen W, Sacks DA (2008) Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999−2005. Diabetes Care 31:899–904
Hedderson MM, Darbinian JA, Ferrara A (2010) Disparities in the risk of gestational diabetes by race-ethnicity and country of birth. Paediatr Perinat Epidemiol 24:441–448
Sinha B, Brydon P, Taylor RS et al (2003) Maternal ante-natal parameters as predictors of persistent postnatal glucose intolerance: a comparative study between Afro-Caribbeans, Asians and Caucasians. Diabet Med 20:382–386
Lee AJ, Hiscock RJ, Wein P, Walker SP, Permezel M (2007) Gestational diabetes mellitus: clinical predictors and long-term risk of develo** type 2 diabetes. Diabetes Care 30:878–883
Oldfield MD, Donley P, Walwyn L, Scudamore I, Gregory R (2007) Long term prognosis of women with gestational diabetes in a multiethnic population. Postgrad Med J 83:426–430
**ang AH, Li BH, Black MH et al (2011) Racial and ethnic disparities in diabetes risk after gestational diabetes. Diabetologia 54:3016–3021
Kanaya AM, Adler N, Moffet HH et al (2011) Heterogeneity of diabetes outcomes among Asians and Pacific Islanders in the U.S. Diabetes Care 34:930–937
Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV (2011) Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care 34:1741–1748
Statistics Canada. (2008) Ethnocultural portrait of Canada Highlight tables, 2006 Census. 97-562-XWE2006002. Ottawa, Statistics Canada.
Canadian Diabetes Association Clinical Practice Guidelines Expert Committee (2008) Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 32:S1–S201
Hux JE, Ivis F, Flintoft V, Bica A (2002) Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 25:512–516
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Shah BR, Chiu M, Amin S, Ramani M, Sadry S, Tu JV (2010) Surname lists to identify South Asian and Chinese ethnicity from secondary data in Ontario, Canada: a validation study. BMC Med Res Methodol 10:42
Leiter LA, Barr A, Bélanger A et al (2001) Diabetes screening in Canada (DIASCAN) study. Diabetes Care 24:1038–1043
Anna V, van der Ploeg HP, Cheung NW, Huxley RR, Bauman AE (2008) Sociodemographic correlates of the increasing trend in prevalence of gestational diabetes mellitus in a large population of women between 1995 and 2005. Diabetes Care 31:2288–2293
Savitz DA, Janevic TM, Engel SM, Kaufman JS, Herring AH (2008) Ethnicity and gestational diabetes in New York City, 1995–2003. BJOG 115:969–978
Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373:1773–1779
Retnakaran R, Hanley AJG, Connelly PW, Sermer M, Zinman B (2006) Ethnicity modifies the effect of obesity on insulin resistance in pregnancy: a comparison of Asian, South Asian, and Caucasian women. J Clin Endocrinol Metab 91:93–97
O'Sullivan JB, Mahan CM (1964) Criteria for the oral glucose tolerance test in pregnancy. Diabetes 13:278–285
Snyder J, Shrim A, Nudi M, Meltzer SJ (2010) Ethnic differences in gestational diabetes testing results, prevalence and perinatal outcomes. Can J Diabetes 34:250
Wilson S, Rosella L, Lipscombe L, Manuel D (2010) The effectiveness and efficiency of diabetes screening in Ontario, Canada: a population-based cohort study. BMC Publ Health 10:506
Ng E, Dasgupta K, Johnson JA (2008) An algorithm to differentiate diabetic respondents in the Canadian Community Health Survey. Health Reports 19:71–79
Maddigan SL, Feeny DH, Majumdar SR, Farris KB, Johnson JA (2006) Understanding the determinants of health for people with type 2 diabetes. Am J Public Health 96:1649–1655
Brar S, Tang S, Drummond N et al (2009) Perinatal care for South Asian immigrant women and women born in Canada: telephone survey of users. J Obstet Gynaecol Can 31:708–716
Alberti KGMM, Zimmet P, Shaw J (2006) Metabolic syndrome: a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 23:469–480
WHO expert consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163
Razak F, Anand SS, Shannon H et al (2007) Defining obesity cut points in a multiethnic population. Circulation 115:2111–2118
Acknowledgements
The authors would like to thank F. Wu for assistance with the statistical analysis of the data, and P. Austin and D. Redelmeier for their comments on earlier drafts of the manuscript.
Funding
B. R. Shah is supported by the Canadian Institutes of Health Research and the Canadian Diabetes Association. The Institute for Clinical Evaluative Sciences is funded, in part, by the Ontario Ministry of Health and Long-Term Care.
Duality of interest statement
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
BRS and GM participated in the conception and design of the study, and drafted the article. All authors contributed to the analysis and interpretation of data, and the revision of the manuscript for important intellectual content. All authors gave final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mukerji, G., Chiu, M. & Shah, B.R. Impact of gestational diabetes on the risk of diabetes following pregnancy among Chinese and South Asian women. Diabetologia 55, 2148–2153 (2012). https://doi.org/10.1007/s00125-012-2549-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2549-6