Abstract
Aims/hypothesis
To investigate racial/ethnic disparities in diabetes risk after gestational diabetes mellitus (GDM).
Methods
This is a retrospective cohort study of women enrolled in the Kaiser Permanente Southern California health plan from 1995 to 2009. GDM status was identified on the basis of plasma glucose levels during pregnancy. The incidence of diabetes after the first delivery complicated by GDM before 31 December 2009 (n = 12,998) was compared with the experience for women without GDM (n = 64,668) matched on maternal age at delivery, race/ethnicity and year of delivery (1:5 ratio). Matched Cox regression was used to compare the RRs of diabetes associated with GDM within and across racial/ethnic groups.
Results
Compared with the women without GDM, the HRs (95% CI) of diabetes for women after GDM were 6.5 (5.2, 8.0) in non-Hispanic white, 7.7 (6.8, 8.7) in Hispanic, 9.9 (7.5, 13.1) in black and 6.3 (5.0, 7.9) in Asian/Pacific Islanders after adjustment for parity, maternal education, comorbidity and number of outpatient visits before the index pregnancy. The HR of diabetes for black women was significantly higher than that for non-Hispanic white women (p = 0.032). Further adjustment for prepregnancy BMI reduced the diabetes risk association with GDM for each racial/ethnic group, but did not explain the risk differences across groups.
Conclusions/interpretations
Racial/ethnic disparities exist in risk of diabetes after GDM. Black women with GDM had the highest risk of develo** diabetes. This highlights the importance of develo** an effective diabetes screening and prevention programme in women with GDM, particularly black women with GDM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM) is a state of glucose intolerance first detected during pregnancy [1, 8, 10]. Moreover, the authors concluded that such risk appeared to be similar across all ethnic groups despite large variations in the RR among studies.
To address whether differences in GDM prevalence across race/ethnicity translate into similar disparities in overt diabetes conversion after GDM across race/ethnicity, we conducted a large retrospective matched cohort study in a racially/ethnically diverse population. The purpose of this study was to investigate racial/ethnic disparities in diabetes risk after GDM.
Methods
Population and data sources
The study cohort comprised women who had a singleton delivery at ≥20 weeks gestation in Kaiser Permanente Southern California (KPSC) hospitals between 1 January 1995 and 31 December 2008. KPSC is an integrated healthcare system that provides comprehensive prepaid health services for its over 3 million members in 2011. Members are demographically/socioeconomically diverse. Study data were extracted from multiple clinical and administrative data systems and from infant birth certificates. Pregnancy and delivery-related information (maternal age, education and race/ethnicity; last menstrual period [LMP], parity and date of delivery) were obtained from the infant birth certificates. Maternal race/ethnicity was categorised as Hispanic (regardless of race), non-Hispanic white (NHW), black, API and ‘other’, which included women with other, multiple or unknown race. Maternal comorbidity was defined as one or more diagnoses of heart, lung, kidney or liver disease or cancer based on inpatient and outpatient encounter codes before index delivery. Prepregnancy medical utilisation was defined as the number of outpatient visits in the year before the LMP of the index pregnancy. Prepregnancy height and weight, when available, were extracted from the electronic health record. This study was approved by the KPSC Institutional Review Board.
Identification of women with GDM
Women who had known type 1 diabetes (ICD-9 [www.icd9data.com/2007/Volume1/240-279/250-259/250/default.htm] of 250.X1 and 250.X3) or existing diabetes before the study entry were excluded. Women were classified as having GDM on the basis of their plasma glucose levels during pregnancy according to the following hierarchy: (1) at least two levels meeting or exceeding the Carpenter and Coustan threshold values [11] (fasting ≥5.3, 1 h ≥ 10.0, 2 h ≥ 8.6 and 3 h ≥ 7.8 mmol/l) during the 100 g, 3 h OGTT; or (2) at least two levels during the 75 g, 2 h OGTT greater than or equal to the same threshold values [11]; or (3) a single level of 1 h, 50 g glucose challenge test (GCT) ≥11.1 mmol/l.
Identification of incident diabetes
Non-pregnant women were classified as having diabetes if they met at least one of the following criteria after the index pregnancy: (1) plasma glucose levels meeting the American Diabetes Association diabetes diagnosis criteria (fasting ≥7.0 mmol/l or 2 h ≥ 11.1 mmol/l from 75 g OGTT, or a random level ≥11.1 mmol/l, where fasting and 2 h were confirmed on a separate day with a repeat test within 6 months) [11]; or (2) HbA1c level ≥7.0% (53 mmol/mol) or (3) a prescription of insulin or other oral glucose-lowering drugs; or (4) an ICD-9 code of 250.xx from one or more inpatient encounters, or two or more outpatient encounters within 2 years. Women who took metformin who were also diagnosed as having polycystic ovary syndrome (ICD-9 256.xx) and had no other indicator of diabetes were not considered to have diabetes.
Subject selection and follow-up
Women were followed passively through their electronic health records for a diagnosis of diabetes. Follow-up started on the index delivery date for women with and without GDM. To minimise bias due to disenrollment and to assess relatively long-term diabetes risk, all women were required to have at least 1 year of continuous health plan membership (allowing gaps for up to 90 days) before the LMP before the index pregnancy and at least 1 year of continuous membership (allowing gaps for up to 90 days) after their index delivery. Follow-up ended on the first date that any one of the following criteria was met: (1) a diagnosis of diabetes; (2) death from any cause; (3) last date where a gap of greater than 4 months of inactive health plan membership occurred; or (4) 31 December 2009, the end of the study period. A total of 139,344 women met these continuous membership criteria, from which a matched-pair cohort was derived. Each woman with GDM was matched to five women without GDM by random sampling of all eligible women without GDM matching on race/ethnicity, age (±3 years) and calendar year of study entry. Women with GDM who could not be matched to any suitable women without GDM were not included. Overall, 91% of women with GDM were included in the matched cohort.
Statistical data analysis
Parity at the time of the index pregnancy was categorised into 0, 1, ≥2 or missing. Education was classified into ≤high school graduate, some college, ≥college graduate, or missing. History of any comorbid condition was classified as present or absent (yes/no). Crude incidence of diabetes was calculated by number of women who developed diabetes divided by the total number of person-years of follow-up. Crude rate ratio and 95% CI comparing women with and without GDM by race/ethnicity were computed and tested for statistical significance by Poisson regression. Cumulative incidence rates of diabetes by race/ethnicity and maternal GDM status were estimated by the Kaplan–Meier method. Matched Cox regression models were used to estimate the adjusted (for parity, education, presence of comorbidity and prepregnancy medical utililsation) HRs of develo** diabetes after GDM. The few women with missing parity and/or education data were included in all data analyses by including missing indicator variables as covariates in the adjusted analyses. The Cox regression analyses were first performed within each racial/ethnic group to estimate the covariate-adjusted racial/ethnic specific HR of develo** diabetes associated with GDM. To assess whether HRs differed across racial/ethnic groups, Cox regression analyses were then performed by combining data from all groups with NHW women as the reference group and testing for significant first-order interaction between GDM status and other racial/ethnic group indicator.
We performed additional analyses to assess whether obesity could explain the racial/ethnic disparities in the risk of develo** diabetes after GDM. Index prepregnancy BMI data were available for only 13,118 (16.7%) of the women in the matched cohort because of the roll-out of the electronic health record across the region starting in 2006. We imputed missing BMI by multiple imputations where known index pregnancy characteristics were incorporated with the Markov Chain Monte Carlo approach. This is a simulation-based approach for estimating the missing data from the predicted distributions on the basis of available observed data. The approach produces valid estimates when data are missing at random. Twenty imputed datasets were created. Matched Cox regression was performed for each of the imputed datasets, with prepregnancy BMI included in the models in addition to other index pregnancy characteristics. The results were combined using Rubin’s rule to incorporate the variations across the 20 imputed datasets [12].
SAS Enterprise Guide 4.3 (SAS Institute Inc, Cary, NC, USA) was used for data analysis. PROC MI and PROC MIANALYZE were used for multiple imputations. All statistical tests were two-sided, and statistical significance was defined as p ≤ 0.05.
Results
Characteristics of women with and without GDM
A total of 139,334 women met the singleton pregnancy and KPSC membership duration criteria for consideration for the study; 14,299 (10.3%) were identified as having GDM (81.6% by 100 g 3 h OGTT, 9.0% by 75 g 2 h OGTT, and 9.4% by 50 g 1 h GCT). GDM was most prevalent in API (17.1%) and Hispanic (11.4%) women, while GDM prevalence was comparable among NHW (7.4%), black (6.9%) and other (7.7%) women. Across all racial/ethnic groups, women with GDM were older and had higher parity than women without GDM (data not shown).
Of the 14,299 eligible women with GDM, 12,998 (91%) were successfully matched by age, race/ethnicity and calendar year of entry to a total of 64,668 women without GDM (i.e. 52% of the eligible controls). The remaining 9% of women with GDM could not be matched to appropriate controls. In the matched cohort (Table 1), there were small but statistically significant differences between GDM exposed and unexposed in parity, education, presence of comorbidities, and prepregnancy visits. Age differed by only 0.1 year. Race/ethnicity was well matched between the two groups.
Incident diabetes
In the matched cohort, a total of 2,657 women developed diabetes during 439,584 person-years of follow-up, which included 456 NHW, 1,464 Hispanic, 309 black, 403 API and 25 women of other race/ethnicity. The corresponding median years of follow-up were 4.5, 5.2, 4.4, 4.8 and 3.9, respectively. The crude incidences of diabetes, stratified by GDM status and race/ethnicity, along with the corresponding rate ratios comparing women with and without GDM, are presented in Table 2. The diabetes incidence rates varied by race/ethnicity and GDM status. Black women with GDM had the highest rate of develo** diabetes (29 cases per 1,000 person-years of follow-up). This rate was 9.2-fold higher (95% CI 7.2, 11.7, p < 0.001) than in the similar age black women without GDM (3.2 cases per 1,000 person-years of follow-up), representing the highest RR of diabetes associated with GDM among all racial/ethnic groups.
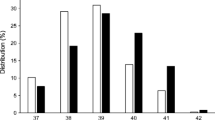
Figure 1a depicts the Kaplan–Meier plot of cumulative risk of diabetes in women stratified by GDM status and race/ethnicity. HRs from matched Cox regression analysis with adjustment for parity, education, presence of comorbidity and number of prepregnancy outpatient visits are shown in Fig. 1b. After adjustment for these covariates, the HRs (95% CI) of develo** diabetes after GDM were 6.5 (5.2, 8.0) in NHW, 7.7 (6.8, 8.7) in Hispanic, 9.9 (7.5, 13.1) in black, 6.3 (5.0, 7.9) in API, and 10.5 (3.3, 33.3) in other women. The risk in black women was 52% higher than that in NHW (p = 0.032 from the interaction term testing for difference in HRs). The RR in Hispanic, API and other women was not significantly different from the RR for NHW women (p = 0.21, 0.76 and 0.54, respectively).
Kaplan–Meier plot of diabetes cumulative incidence rates stratified by GDM status and race/ethnicity (a) and adjusted HR of develo** diabetes comparing GDM with non-GDM by race/ethnicity (b). The horizontal line in b is the 95% CI. The p value tests whether the HR in other racial/ethnic groups is significantly different from that in NHW. All p values for comparison with NHW are not significant (p > 0.05) except for Black without (p = 0.032) and with (p = 0.028) BMI adjustment. Black, NHW; blue, Hispanic; red, black; green, API; purple, other
Impact of obesity on the disparities in risk of diabetes associated with GDM
Table 3 presents the number of women with measured prepregnancy BMI data and differences in mean observed BMI between women with and without GDM by racial/ethnic group. The average prepregnancy BMI was lowest in API women and highest in black women. In addition, BMI in women with GDM was 2–4 units higher than in women without GDM across all racial/ethnic groups (p ≤ 0.0004). After imputation of missing BMI data, the matched Cox regression models further adjusted for maternal BMI demonstrated that the association between GDM and diabetes was attenuated in all racial/ethnic groups (Fig. 1b). However, the difference in BMI did not account for the entire excess risk of diabetes associated with GDM, and it did not account for the difference in RR across racial/ethnic groups. GDM remained a significant risk factor for diabetes in every racial/ethnic group with HRs ranging from 4.4 to 7.6. The RR in black women remained significantly higher than that in NHW women (7.6 vs 4.4, p = 0.028). The corresponding p values comparison of Hispanic, API and other women with NHW women were 0.20, 0.70 and 0.88, respectively.
Discussion
In this systematic assessment of racial/ethnic disparities in the development of diabetes after GDM in a large diverse cohort of insured women, diabetes risk associated with GDM was shown to vary by maternal race/ethnicity. Despite the fact that the prevalence of GDM in black women was low relative to women from other racial/ethnic minority groups, as demonstrated in other studies [4, 6, 7], black women who developed GDM had the highest risk of develo** diabetes after GDM, independent of age, parity, education, comorbidity status, prepregnancy medical utilisation and BMI. Similarly, although the GDM prevalence was the highest among API women, the risk of develo** diabetes after GDM was comparable to that in NHW women.
The overall RR of develo** diabetes associated with GDM in our study was 7.3, which is consistent with the meta-analysis result of Bellamy et al. [10], which included 20 studies published from 1960 through January 2009 that included 675,455 women with and without GDM and 10,859 diabetes events. The pooled estimate of RR of diabetes associated with GDM was 7.4 with variation across studies. However, as the authors pointed out, they had little capability to evaluate the variations across race/ethnicity because they did not have individual-level data. Our study is based on individual-level data collected uniformly across women in a large multi-ethnic cohort. We demonstrated that there is significant variation in the RR and absolute risk of develo** diabetes after GDM across racial/ethnic groups, where risk is the highest in black women. Another large sample population-based study assessing RR of develo** diabetes associated with GDM was based on the Ontario Diabetes Database by Feig et al. [13]. The authors reported an adjusted HR of 37.3 (95% CI 35.0, 40.9) associated with GDM. However, much of the high risk was due to the greatest risk in the first year post partum, which may also include pre-existing undiagnosed diabetes from women with GDM (Fig. 2 of Feig et al.). After the first year, the unadjusted RR is ~7.2 (estimated from their Fig. 2), which is similar to our estimate. Race/ethnicity distribution was not reported in that study.
We acknowledge several potential limitations of our study. First, pre-index pregnancy BMI data were available for only ~17% of the cohort because of the timing of electronic health record implementation across medical centres within KPSC. It is likely that the data were missing at random, and our use of multiple imputations should provide valid estimates. In addition, follow-up time was truncated by health plan disenrollment, at which point subjects were censored in the survival analysis. However, it is reasonable to assume that disenrollment is unrelated to diabetes risk in this relatively young cohort of women of reproductive age. Thus, censoring was non-informative and the use of survival analysis was appropriate. Finally, diabetes incidence rates may be underestimated because of sub-clinical diabetes which would not be found in the medical record. The diabetes incidence rate was 2.5%/year in Hispanic women with GDM in this cohort (Table 2), which was much lower than the 7.2%/year or the 11%/year observed previously in smaller cohort studies of Hispanic women with GDM [ Asian/Pacific Islanders Glucose challenge test Gestational diabetes mellitus Kaiser Permanente Southern California Last menstrual period Non-Hispanic white American Diabetes Association (2011) Standards of medical care in diabetes—2011. Diabetes Care 34(Suppl 1):S11–S61 Buchanan TA, **ang A, Kjos SL, Watanabe R (2007) What is gestational diabetes? Diabetes Care 30(Suppl 2):S105–S111 Berkowitz GS, Lapinski RH, Wein R, Lee D (1992) Race/ethnicity and other risk factors for gestational diabetes. Am J Epidemiol 135:965–973 Lawrence JM, Contreras R, Chen W, Sacks DA (2008) Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999–2005. Diabetes Care 31:899–904 Hedderson MM, Darbinian JA, Ferrara A (2010) Disparities in the risk of gestational diabetes by race–ethnicity and country of birth. Paediatr Perinat Epidemiol 24:441–448 Ferrara A, Kahn HS, Quesenberry CP, Riley C, Hedderson MM (2004) An increase in the incidence of gestational diabetes mellitus: Northern California, 1991–2000. Obstet Gynecol 103:526–533 Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS (2005) Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care 28:579–584 Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 25:1862–1868 Kjos SL, Peters RK, **ang A, Henry OA, Montoro M, Buchanan TA (1995) Predicting future diabetes in Latino women with gestational diabetes. Utility of early postpartum glucose tolerance testing. Diabetes 44:586–591 Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373:1773–1779 Association AD (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33(Suppl 1):S62–S69 Rubin DB (1987) Multiple imputation for nonresponse in surveys. Wiley, New York Feig DS, Zinman B, Wang X, Hux JE (2008) Risk of development of diabetes mellitus after diagnosis of gestational diabetes. CMAJ 179:229–234 **ang AH, Kjos SL, Takayanagi M, Trigo E, Buchanan TA (2010) Detailed physiological characterization of the development of type 2 diabetes in Hispanic women with prior gestational diabetes mellitus. Diabetes 59:2625–2630 This work was supported by Kaiser Permanente Southern California Direct Community Benefit funds. All authors contributed to the conception and design, or analysis and interpretation of data; drafted the article or revised it critically for important intellectual content; and have final approval of the version to be published. All the authors declare that they have no duality of interest associated with this manuscript. **ang, A.H., Li, B.H., Black, M.H. et al. Racial and ethnic disparities in diabetes risk after gestational diabetes mellitus.
Diabetologia 54, 3016–3021 (2011). https://doi.org/10.1007/s00125-011-2330-2 Received: Accepted: Published: Issue Date: DOI: https://doi.org/10.1007/s00125-011-2330-2Abbreviations
References
Acknowledgements
Contribution statement
Duality of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keywords