Abstract
Purpose
Our previous studies have demonstrated that human parvovirus B19 (B19V) is involved in the pathogenesis of thymic hyperplasia-associated myasthenia gravis (MG). However, more cases need to be assessed to further elucidate the relationship between this virus and thymoma-associated MG.
Materials and Methods
The clinicopathological characteristics, presence of B19V DNA, and B19V VP2 capsid protein expression of 708 cases of thymomas were investigated using nested polymerase chain reaction (PCR), TaqMan quantitative (q) PCR, immunohistochemistry, fluorescent multiplex immunohistochemistry, and electron microscopy.
Results
Patients with MG or ectopic germinal centers (GCs) were significantly younger than those without MG (P < 0.0001) or GCs (P = 0.0001). Moreover, significantly more GCs were detected in thymomas associated with MG than in those without MG (P < 0.0001). The results of nested PCR and TaqMan qPCR were consistent, and B19V DNA positivity was only associated with presence of GCs (P = 0.011). Immunohistochemically, positive staining was primarily detected in neoplastic thymic epithelial cells (TECs) and ectopic GCs. The positive rate of B19V VP2 was significantly higher in thymoma with MG or GCs than in thymoma without MG (P = 0.004) or GCs (P = 0.006). Electron microscopy showed B19V particles in the nuclei of neoplastic TECs and B cells from GCs.
Conclusions
We conclude that the pathogenesis of MG is closely associated with the presence of GCs, and B19V infection is plausibly an essential contributor to formation of ectopic GCs in thymoma. To the best of the authors’ knowledge, this is the first study to elucidate the role of B19V in thymoma-associated MG and provide new ideas for exploring the etiopathogenic mechanism of MG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Myasthenia gravis (MG) is an autoimmune disease characterized by skeletal muscle fatigue and is directly mediated by different autoantibodies against various components of the neuromuscular junction, primarily the anti-acetylcholine receptor (anti-AChR) antibody. The thymus of individuals with MG contains numerous B-lymphocytes producing antibodies. Thymic abnormalities including thymic hyperplasia and thymoma may contribute to the pathophysiology of MG, in view of the fact that > 80% of patients with early-onset MG present thymic hyperplasia, particularly thymic follicular hyperplasia with ectopic germinal centers (GCs), and 10–15% of MG patients present with comorbid thymoma.1,2 Thymic hyperplasia is characterized by the organization of B-lymphocytes into ectopic GCs or their distribution throughout the thymic medulla. Thymic follicular hyperplasia with GCs significantly contributes to MG pathogenesis.3,4 Thymoma is the most frequent anterior mediastinal tumor originating from thymic epithelial cells (TECs) in adults. Histologically, it is primarily classified in accordance with World Health Organization (WHO) guidelines as type A, AB, B1, B2, and B3 thymoma in addition to other rare types. In general, immature T cells are the most common cell types in thymoma, while B cells are present in small numbers and are less prominent in the thymus. However, ectopic GCs resulting from B-cell infiltration are usually found in thymoma during routine pathological diagnosis; this phenomenon attracts our interest. Similarly, Lefeuvre et al. have reported that presence of GCs in thymoma is a risk factor facilitating the evaluation of the risk of MG,5 but the cause of GCs formation has not been elucidated.
In general, chronic inflammation of the thymus caused by a viral or bacterial infection may trigger the development of autoimmunity, generally by activating the host immune system and molecular mimicry, thereby contributing to the pathogenesis of MG. Some studies have demonstrated that intrathymus Epstein–Barr virus (EBV) infection is an environmental risk factor for MG.6,7 However, an increasing number of studies have reported a lack of evidence for EBV infection in the thymus of patients with MG.8,9,10 Hence, the role of EBV in the pathogenesis of MG remains controversial.
Human parvovirus B19 (B19V) is a small, nonenveloped, single-stranded DNA virus that is a member of the genus Erythroparvovirus in the family Parvoviridae.11 It has been reported that B19V is associated with various autoimmune diseases, including systemic lupus erythematosus, Hashimoto’s thyroiditis, and rheumatoid arthritis.12,13,14,15 We have previously reported that B19V is closely associated with thymic B-cell hyperplasia, the presence of GCs, and thymic hyperplasia-associated MG. Moreover, the B19V DNA or B19V capsid proteins VP1 and VP2 have been detected in only a few cases of thymoma as the control group.16 Simultaneously, anti-B19V IgG antibodies are associated with MG in the serum of patients with thymoma.17 Based on the aforementioned findings and the vast diagnostic resources available on thymoma, we aim to investigate the clinicopathological characteristics of thymoma, especially the presence of GCs, the expression of human B19V DNA and protein in thymoma, and its association with MG.
Materials and Methods
Tissue Samples
A total of 708 surgically resected specimens with thymoma were retrieved from the Department of Pathology between January 2014 and December 2019. The study protocol was approved by the Medical Ethics Commission of Tangdu Hospital. Informed verbal or written consent was obtained from all patients before surgery. Sixty-six cases of normal thymus tissues were obtained as controls from thymic tissue surgically resected for intrathoracic nodular goiter, congenital heart disease, and thymic cyst. All samples were fixed in 10% neutral formalin and embedded in paraffin. All sections with thymoma were carefully reviewed and diagnosed by three pathologists in accordance with WHO guidelines. Furthermore, their clinicopathological data including sex, age, presence of GCs, and occurrence of MG were documented. MG was clinically diagnosed by physicians, primarily on the basis of the following characteristics: typical clinical manifestation, positive response to cholinesterase inhibitors, and decreased response to repetitive electrical stimulation of the motor nerve.
DNA Extraction, Nested PCR, and TaqMan qPCR
Five 5-µm-thick tissue sections obtained from representative paraffin blocks were deparaffinized in xylene and rehydrated in a graded ethanol series. Subsequently, genomic DNA was extracted using the TIANamp FFPE DNA Kit (Tiangen, DP331, China) in accordance with the manufacturer’s instructions and stored at − 20 °C until use. Nested PCR was performed to amplify a region of the B19V genome as previously described.15 Finally, the PCR products were visualized by electrophoresis using a 4% polyacrylamide gel, and a band at 173 bp was considered to indicate a positive reaction.
TaqMan qPCR was performed as described by Knoll Antje et al.18 using a method calibrated on the basis of serial plasmid dilutions and tested with an international B19V standard to confirm the results of nested PCR. The sequences for two sets of primers and probes were from two conserved regions of the B19V genome coding for NS1 and VP2 proteins. Amplification was performed in a 20 µL reaction volume using 2× TaqMan Fast qPCR Master Mix (Sangon Biotech, Shanghai, B639274).The two reactions were carried out separately on a Cobas Z 480 system (Roche, USA). A sharp exponential rise of the sigmoid curve compared with the relative horizontal line was considered to indicate positive amplification in fluorescence.
Nested PCR and TaqMan qPCR were performed in triplicate and included negative and positive controls.
Immunohistochemical Staining
Immunohistochemistry (IHC) was performed according to the manufacturer’s instructions, and included primary antibodies against mouse anti-B19V VP2 (1:50, Clone R92F6, Merck Millipore/Abcam, USA/UK), CD20 (L26, MXB®, China; 1:400, Clone EP459Y, Abcam, UK), CK19 (A53-B/A2.26, MXB®, China), CD4 (SP35, MXB®, China), and Ki-67 (MIB-1, MXB®, China). Brown staining of nuclei indicated positivity toward B19V VP2. Double immunoenzyme staining was performed for CD20, CK19, CD4, and B19V VP2 to identify the exact phenotype of B19V VP2-positive cells. Red staining of nuclei indicated positivity toward B19V VP2, and brown coloration at the cell membrane indicated positivity for CD20, CK19, and CD4.
Fluorescent Multiplex Immunohistochemistry
To further highlight cells with B19V VP2 positivity, two cases of thymoma were analyzed using an AlphaTSA Multiplex IHC Kit (Alpha X Biotech CO., LTD, Bei**g, China) according to the manufacturer’s manual. The main procedures were as follows: first, after the slides were deparaffinized in xylene, rehydrated in graded alcohol, washed in distilled water, and retrieved in EDTA buffer, the slides were blocked using antibody diluent/block; second, the slides were incubated with primary antibody for 1 h and AlphaX Polymerase HRP Ms+Rb for 10 min at 37 °C; third, the fluorescent dyes included in the kit were used for visualization. After each cycle of staining, heat-induced epitope retrieval was performed to remove the former antibodies. The labeling of CK19, CD20, and B19V VP2 was completed using the methods described above. Finally, the slides were counterstained with DAPI for 5 min and enclosed in Antifade Mounting Medium. The correspondence between primary antibodies and fluorophores was CK19 (XTSA520, Green), CD20 (XTSA570, Red), and B19V VP2 (XTSA690, White).
ISH for Epstein–Barr Virus (EBV)
To determine whether EBV infection occurs in the thymus of MG patients, EBV was detected via ISH for EBV-encoded RNA (EBER) as gold standard,19 using the Slide Denaturation & Hybridization System (ThermoBrite, S500-24, USA) in accordance with the manufacturer’s instructions (ZSGB-BIO, ISH-7001, China). EBER staining was considered positive if granular, brown reaction products were found in the nucleus. EBER-positive nasal NK/T-cell lymphoma tissue was used as a positive control.
Electron Microscopy
To provide more evidence for B19V infection in thymoma associated with MG, we randomly selected five diffusely and strongly positive cases of thymoma and two cases of thymoma negative for B19V VP2 to determine the presence of B19V in TECs and/or B cells by electron microscopy. In detail, a piece of tissue approximately 1 mm × 1 mm × 1 mm in size from the paraffin-embedded tissue was first obtained. Then, the tissue was sequentially deparaffinized in xylene, rehydrated in a graded ethanol series, and washed in PB buffer. Finally, the cells were fixed in 4% glutaraldehyde buffer for transmission electron microscopy (Hitachi, HT7800, Japan).
Statistical Analysis
Data were analyzed using IBM SPSS 25.0 software for Windows (SPSS Inc., Chicago, IL, USA). Differences in clinical parameters between groups were analyzed using Pearson’s chi-squared test and Fisher’s exact test. A two-tailed P value < 0.05 was considered to indicate statistically significant difference.
Results
Clinicopathological Characteristics of 708 Cases of Thymoma
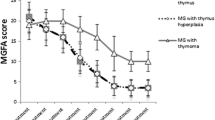
In total, 708 patients with thymoma, including 361 men and 347 women aged 15–77 years (mean age, 52 years; peak, 50–59 years), were recruited from seven provinces in China. Among these, 416 patients were aged ≥ 50 years, and 292 patients were aged < 50 years (Supplementary Table 1; Fig. 1A). The most common histological subtypes of thymoma were AB, B2, B1, B3, and A, accounting for 35.6% (252/708), 28.4% (201/708), 16% (113/708), 8.6% (61/708), and 8.6% (61/708) of the cases, respectively (Supplementary Table 2; Fig. 1B). MG occurred in 33.2% (235/708) of all the thymoma patients; these patients (52.8%, 124/235) were significantly younger than those without MG (35.5%, 168/473) (P < 0.0001) (Supplementary Table 3; Fig. 2). MG occurrence peaked at 40–49 years (Supplementary Table 1; Fig. 1A). Furthermore, the incidence ratio was highest for type B2 thymoma among all subtypes (47.2%, 111/235) (Supplementary Table 2; Fig. 1B). Ectopic GCs were detected in 238 cases (33.6%, 238/708) and were localized in intratumor and/or tumor-adjacent thymus tissues. The GCs occurrence ratio was highest for type B2 thymoma (42.4%, 101/238). Furthermore, patients with GCs (51.3%, 122/238) were significantly younger than those without GCs (36.2%, 170/470) (P = 0.0001). The presence of GCs in thymoma patients with MG comorbidity (51.1%, 120/235) was significantly higher than in those without MG (25%, 118/473) (P < 0.0001) (Supplementary Table 3; Figs. 1B and 2). These results indicated that both MG and GCs primarily occurred among thymoma patients aged < 50 years and that MG was associated with presence of ectopic GCs.
Percentage of patients with and without each parameter in different age groups and subtypes of thymoma. A peak was observed for patients with thymoma, thymoma-associated MG, and presence of GCs in the 50–59, 40–49, and 40–49 year groups, respectively (A); a peak was observed for patients with thymoma-associated MG, GCs, B19V DNA positivity, and B19V VP2 positivity in type B2 thymoma (B)
Differences in clinical parameters in thymoma patients with and without MG, GCs, and B19V DNA amplification. Patients with MG or ectopic GCs were significantly younger than those without MG (P < 0.0001) or GCs (P = 0.0001). In addition, significantly more GCs were detected in thymoma patients with MG than in those without MG (P < 0.0001). The positivity rate of B19V DNA was only associated with presence of GCs (P = 0.011). The positivity rate of B19V VP2 was significantly higher in thymoma patients with MG or GCs than in those without MG (P = 0.004) or GCs (P = 0.006)
Detection of B19V DNA through Nested PCR and TaqMan qPCR
A DNA fragment (predicted size 173 bp) corresponding to B19V DNA was amplified as a marker of B19V infection in 38 (5.4%) of 708 thymomas (Supplementary Tables 1, 2; Supplementary Fig. 1); however, no such fragment was amplified in 66 normal thymus tissue samples. Furthermore, the positivity rate of B19V DNA was significantly higher in thymoma harboring GCs (8.4%, 20/238) than among those without GCs (3.8%, 18/470) (P = 0.011) (Supplementary Table 3; Fig. 2). However, no significant difference was noted in MG, sex, or age of the patients (Supplementary Tables 3, 4; Fig. 2). These results indicated that B19V DNA was only associated with presence of ectopic GCs. In other words, B19V infection in the thymus potentially contributed to the formation of ectopic GCs, subsequently inducing MG.
The results of TaqMan qPCR were consistent with those of nested PCR. In detail, 38 cases with nested PCR positive amplification were positive for the VP2 genomic region but negative for the NS1 genomic region. However, 66 normal thymus tissue samples were negative for the VP2 and NS1 genomic regions.
Detection of B19V VP2 Proteins via IHC and Fluorescent Multiplex IHC
IHC staining results demonstrated that 135 thymoma specimens (19.1%, 135/708) were positive for B19V VP2, with positive staining primarily observed in neoplastic TECs and ectopic GCs located in tumors and/or tumor-adjacent thymic tissues (Supplementary Tables 1, 2; Figs. 1 and 3). Of course, only thymomas with neoplastic TEC staining were considered positive. Moreover, the positivity ratio was highest for type B2 thymoma, followed by types B1, B3, and AB thymoma (Supplementary Table 2; Fig. 1B). However, only neoplastic TECs from type A thymoma were negative (Fig. 4A), as were 66 samples of normal thymus tissue. In addition, the positivity rate was significantly higher in thymoma with MG (25.1%, 59/235) than in thymoma without MG (16.1%, 76/473) (P = 0.004). Similarly, the positivity rate was significantly higher in thymoma patients with GCs (24.8%, 59/238) than in those without GCs (16.2%, 76/470) (P = 0.006) (Supplementary Table 3; Fig. 2). The positivity rate was slightly, but not significantly, higher among patients aged < 50 years (22.3%, 65/292) than among those aged ≥ 50 years (16.83%, 70/416) (P = 0.070). Furthermore, no significant difference in sex was observed (P = 0.118). However, the positivity ratio of B19V VP2 was not associated with positivity (23.7%, 9/38) or negativity (18.8%, 126/670) for B19V DNA (P = 0.457) (Supplementary Table 4). These results indicate that B19V VP2 is associated with MG and/or presence of GCs, further indicating that B19V infection in the thymus potentially contributes to the formation of ectopic GCs, subsequently promoting MG pathogenesis.
Expression and cellular distribution of B19V VP2 protein in different subtypes of thymomas and germinal centers (GCs). The nuclei positive for the B19V VP2 protein were mainly found in ectopic GCs (A, 100×; B, 400×) and neoplastic TECs in the different subtypes of thymoma: type B1 (C, 400×), type B2 (D, 400×), type B3 (E, 400×), and type AB (F, 400×)
Results of IHC, double-labeled IHC, and ISH. Neoplastic TECs from type A thymoma were negative for B19V VP2 (A, 400×). Double-labeled immunohistochemical staining for CD20, CK19, CD4, and B19V VP2 showed that the nuclei of B cells from ectopic GCs (B, 400×) and neoplastic TECs (C, 400×) were strongly and diffusely positive for B19V VP2. Simultaneously, the cell membrane of B cells from ectopic GCs and neoplastic TECs was positive for CD20 (B, 400×) and CK19 (C, 400×) but negative for CD4 (D, 400×). In addition, no positive cases were obtained for EBER (E, 400×), the positive control of EBER (F, 400×)
Double-labeled immunohistochemical staining using CD20, CK19, CD4, and B19V VP2 showed that the nuclei of B cells from ectopic GCs and neoplastic TECs were strongly positive for B19V VP2. Simultaneously, the cell membranes of B cells from ectopic GCs and neoplastic TECs were positive for CD20 (Fig. 4B) and CK19 (Fig. 4C), respectively, but negative for CD4 (Fig. 4D). However, only a very few thymus reticular epithelial cells were weakly positive for B19V VP2 in normal thymus tissues. Similarly, the results of fluorescent multiplex IHC were consistent with those of double-labeled immunohistochemical staining using CD20, CK19, and B19V VP2 (Fig. 5A–J).
Results of fluorescent multiplex IHC. Similarly, the results of fluorescent multiplex IHC were consistent with those of double-labeled immunohistochemical staining using CD20, CK19, and B19V VP2 (A–J). Namely, the nuclei of B cells (C) and neoplastic TECs (H) were positive for B19V VP2. Simultaneously, the cell membrane of B cells from ectopic GCs and neoplastic TECs was positive for CD20 (B, G) and CK19 (A, F), respectively. Panels E and J showed that some cells were positive for both B19V VP2 and CD20, and other cells were positive for both B19V VP2 and CK19
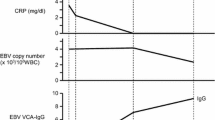
Detection of EBV via ISH
To elucidate whether EBV infection exists in thymoma tissues, we observed the expression of EBER in 708 thymoma samples via ISH. The results demonstrated that none of the cases were positive for EBER compared with the positive control (Fig. 4E, F).
Electron Microscopy
Electron microscopy showed the presence of B19V particles (diameter range 19.7–25.6 nm) in the nuclei of TECs and B cells from GCs in all five cases of thymoma with diffuse and strong positivity for B19V VP2 (Fig. 6A–F) but not in two cases of thymoma with immunohistochemical negativity for B19V VP2 (Fig. 6G–I), confirming B19V infection.
Electron microscopy of seven cases of thymoma. B19V particles were found in the nuclei of TECs (A, ×21.0k; B, ×70.0k; C, ×170k) and B cells (D, ×21.0k; E, ×70.0k; F, ×170k) from GCs in five thymomas that were diffusely and strongly positive for B19V VP2, but no B19V particles were found in the nuclei of TECs (G, ×21.0k; H, ×170k; I, ×170k) in two thymomas that were immunohistochemically negative for B19V VP2, further confirming the presence of B19V infection
Discussion
Thymic abnormalities including thymic hyperplasia and thymoma play a crucial role in MG pathogenesis, and approximately 30% of patients with thymoma have comorbid MG; however, this rate varies widely from 17% to 67%.20,21 Recently, Lefeuvre et al. reported an extraordinarily high rate (78.7%) of MG among patients with thymoma. Moreover, 58.8% of the patients presented ectopic GCs. Thus, they conclude that the presence of ectopic GCs is a potential risk factor for MG occurrence.5 In this study, we found that the positivity rate of MG was 33.2% in thymoma, which is consistent with that reported in most studies. Simultaneously, we noticed that the presence of GCs in patients with MG comorbidity (51.1%) was significantly higher than in those without MG (25%), confirming the above conclusion. Namely, the presence of ectopic GCs may contribute to the occurrence of thymoma-associated MG. In addition, we found that patients with MG or GCs were significantly younger than those without MG or GCs. More interestingly, type B2 thymoma registered the highest incidence ratio of MG and GCs among all types of thymoma. However, the causes of abnormal B-cell proliferation and the formation of ectopic GCs in thymoma remain unknown.
This is the primary feature of target organs characterized by chronic inflammation with B-cell infiltration, especially ectopic GCs formation, in numerous organ-specific autoimmune diseases, and it is also a significant feature of the thymus of MG patients.22,23 Infection with pathogens such as viruses or bacteria is the primary factor leading to chronic thymus inflammation. EBV is one of the most concerning viruses in the literature regarding the correlation between viruses and MG with thymus abnormalities, but the role of EBV in the pathogenesis of MG remains controversial.6,7,8,9,10 Thus, in this study, we mainly explored the role of B19V, a virus playing a similar role to EBV in autoimmune diseases, in thymoma, and further investigated EBV status. B19V was first discovered by Cossart et al. in 1975.24 However, its effect on humans can be traced back hundreds or even thousands of years.25 Moreover, despite their strong erythroid tropism and related acute disease association, B19V RNA or capsid proteins have been reported in many other nonerythroid tissues, including thymus tissues.13,14,15,16 The expression of B19V in the above tissues was also associated with specific changes in the expression of inflammatory genes, demonstrating that persistent B19V expression can impact the cellular microenvironment. In addition, an increasing number of studies have demonstrated that B19V is associated with various autoimmune diseases.12,13,14,15 Simultaneously, based on our previous findings, including the relationship between anti-B19V IgG antibodies in the serum of patients with thymoma and MG and the presence of B19V DNA and B19V VP2 in a few cases of thymoma,16,17 we performed further research with an abundant number of samples using nested PCR, TaqMan qPCR, immunohistochemistry, fluorescent multiplex immunohistochemistry, and electron microscopy. The results demonstrated that the pathogenesis of MG is closely associated with the presence of GCs, and B19V infection is a plausible essential contributor to formation of ectopic GCs in thymoma. Concordant with the results of a previous study that virus RNA might persist in lymphoid tissue accompanied by ongoing proliferation of GCs,26 we found the presence of both B19V DNA and protein in the proliferative GCs of thymoma-associated MG. These results further indicate that B19V infection might cause B-cell proliferation and formation of ectopic GCs, subsequently leading to thymoma-associated MG. Moreover, it has recently been reported that formation of GCs markedly antagonizes other viral infections, such as influenza vaccines and coronavirus disease 2019 (COVID-19) antibodies.27,28,29 Thus, B19V infection of B cells and ectopic GCs in the thymus with MG provides another robust example of the association between viral infection and formation of GCs and extends current understanding of the pathogenesis of this autoimmune disease.
Surprisingly, neoplastic TECs from type A thymoma displayed negative staining for B19V VP2; however, types B2, B1, B3, and AB thymoma were positive, and the results were confirmed by electron microscopy. Moreover, the positivity ratio peaked for type B2 thymoma, followed by types B1, B3, and AB thymoma. These results indicate that B19V VP2 expression is primarily associated with thymoma originating in cortical epithelial cells. In other words, B19V potentially affects TECs in addition to B cells in ectopic GCs. However, further studies are required to elucidate the underlying mechanism.
Of course, our studies present some unexplained results and limitations. For example, B19V messenger RNA (mRNA) expression levels were not provided in the study. In fact, we have tried our best to observe it by various methods described in literature, but they do not seem feasible. In addition, the positivity rate of B19V DNA and protein expression is inconsistent. We speculate that there may be two possible explanations. One is that this may be due to clearance of B19V owing to superinfection with a second virus or because of the persistence of viral antigens in lymphoid tissues during the immunological memory phase, as previously described by Wietzke et al. and Klenerman et al.30,31 The other is that B19V may cause MG only when viral replication and/or load reaches a certain threshold. In fact, this phenomenon was noted not only in studies of B19V but also in those of other viruses, especially hepatitis B virus.32,33,34,35,36,37 Thus, more research is required to elucidate this phenomenon.
In conclusion, this study shows that B19V infection may cause B-cell proliferation and formation of ectopic GCs, subsequently leading to thymoma-associated MG. To the best of the authors’ knowledge, this is the first report of the presence of B19V in TECs and ectopic GCs, revealing an unrecognized etiopathogenic mechanism for thymoma-associated MG. However, further studies are required to elucidate the role of B19V in thymic abnormalities with MG.
Change history
22 December 2022
A Correction to this paper has been published: https://doi.org/10.1245/s10434-022-13017-7
References
Leite MI, Jones M, Ströbel P, et al. Myasthenia gravis thymus: complement vulnerability of epithelial and myoid cells, complement attack on them, and correlations with autoantibody status. Am J Pathol. 2007;171:893–905.
Cavalcante P, Bernasconi P, Mantegazza R. Autoimmune mechanisms in myasthenia gravis. Curr Opin Neurol. 2012;25:621–9.
Berrih-Aknin S, Ruhlmann N, Bismuth J, et al. CCL21 overexpressed on lymphatic vessels drives thymic hyperplasia in myasthenia. Ann Neurol. 2009;66:521–31.
Fujii Y, Monden Y, Nakahara K, Hashimoto J, Kawashima Y. Antibody to acetylcholine receptor in myasthenia gravis: production by lymphocytes from thymus or thymoma. Neurology. 1984;34:1182–6.
Lefeuvre CM, Payet CA, Fayet OM, et al. Risk factors associated with myasthenia gravis in thymoma patients: The potential role of thymic germinal centers. J Autoimmun. 2020;106:102337.
Cavalcante P, Maggi L, Colleoni L, et al. Inflammation and epstein-barr virus infection are common features of myasthenia gravis thymus: possible roles in pathogenesis. Autoimmune Dis. 2011;2011:213092.
Cavalcante P, Serafini B, Rosicarelli B, et al. Epstein-Barr virus persistence and reactivation in myasthenia gravis thymus. Ann Neurol. 2010;67:726–38.
Meyer M, Höls AK, Liersch B, et al. Lack of evidence for Epstein-Barr virus infection in myasthenia gravis thymus. Ann Neurol. 2011;70:515–8.
Kakalacheva K, Maurer MA, Tackenberg B, Münz C, Willcox N, Lünemann JD. Intrathymic Epstein-Barr virus infection is not a prominent feature of myasthenia gravis. Ann Neurol. 2011;70:508–14.
**g F, Wei D, Wang D, et al. Lack of Epstein-Barr virus infection in Chinese myasthenia gravis patients. Acta Neurol Scand. 2013;128:345–50.
Cotmore SF, Agbandje-McKenna M, Chiorini JA, et al. The family Parvoviridae. Arch Virol. 2014;159:1239–47.
Hsu TC, Tsay GJ. Human parvovirus B19 infection in patients with systemic lupus erythematosus. Rheumatology (Oxford). 2001;40:152–7.
Takahashi Y, Murai C, Shibata S, et al. Human parvovirus B19 as a causative agent for rheumatoid arthritis. Proc Natl Acad Sci USA. 1998;95:8227–32.
Adamson LA, Fowler LJ, Clare-Salzler MJ, Hobbs JA. Parvovirus B19 infection in Hashimoto’s thyroiditis, papillary thyroid carcinoma, and anaplastic thyroid carcinoma. Thyroid. 2011;21:411–7.
Wang J, Zhang W, Liu H, et al. Parvovirus B19 infection associated with Hashimoto’s thyroiditis in adults. J Infect. 2010;60:360–70.
Gong L, Li Y, Li X, et al. Detection of human parvovirus B19 infection in the thymus of patients with thymic hyperplasia-associated myasthenia gravis. Clin Microbiol Infect. 2019;25:109.e7-e12.
Jia X, Gong L, Zhang J, et al. Detection of IgM and IgG antibodies to human parvovirus B19 in sera of patients with thymoma-associated myasthenia gravis. Viral Immunol. 2021;34(4):213–7.
Knöll A, Louwen F, Kochanowski B, et al. Parvovirus B19 infection in pregnancy: quantitative viral DNA analysis using a kinetic fluorescence detection system (TaqMan qPCR). J Med Virol. 2002;67:259–66.
Gulley ML, Tang W. Laboratory assays for Epstein-Barr virus-related disease. J Mol Diagn. 2008;10:279–92.
Padda SK, Yao X, Antonicelli A, et al. Paraneoplastic syndromes and thymic malignancies: an examination of the International Thymic Malignancy Interest Group Retrospective Database. J Thorac Oncol. 2018;13:436–46.
Maggi G, Casadio C, Cavallo A, Cianci R, Molinatti M, Ruffini E. Thymoma: results of 241 operated cases. Ann Thorac Surg. 1991;51:152–6.
Cron MA, Maillard S, Villegas J, et al. Thymus involvement in early-onset myasthenia gravis. Ann N Y Acad Sci. 2018;1412:137–45.
Truffault F, de Montpreville V, Eymard B, Sharshar T, Le Panse R, Berrih-Aknin S. Thymic germinal centers and corticosteroids in myasthenia gravis: an immunopathological study in 1035 cases and a critical review. Clin Rev Allergy Immunol. 2017;52:108–24.
Cossart YE, Field AM, Cant B, Widdows D. Parvovirus-like particles in human sera. The Lancet. 1975;305:72–3.
Mühlemann B, Margaryan A, Damgaard PB, et al. Ancient human parvovirus B19 in Eurasia reveals its long-term association with humans. Proc Natl Acad Sci USA. 2018;115:7557–62.
Tian M, Hua Z, Hong S, et al. B Cell-intrinsic MyD88 signaling promotes initial cell proliferation and differentiation to enhance the germinal center response to a virus-like particle. J Immunol. 2018;200:937–48.
Turner JS, Zhou JQ, Han J, et al. Human germinal centres engage memory and naive B cells after influenza vaccination. Nature. 2020;586:127–32.
Kaneko N, Kuo HH, Boucau J, et al. Loss of Bcl-6-expressing T follicular helper cells and germinal centers in COVID-19. Cell. 2020;183:143-157.e13.
Fallet B, Hao Y, Florova M, et al. Chronic viral infection promotes efficient germinal center B cell responses. Cell Rep. 2020;30:1013-1026.e7.
Wietzke P, Schott P, Braun F, Mihm S, Ramadori G. Clearance of HCV RNA in a chronic hepatitis C virus-infected patient during acute hepatitis B virus superinfection. Liver. 1999;19:348–53.
Klenerman P, Hengartner H, Zinkernagel RM. A non-retroviral RNA virus persists in DNA form. Nature. 1997;390:298–301.
Ye X, Li T, Zhang R, et al. Comprehensive analysis of hepatitis B virus infections in blood donors in southern China that are surface antigen positive but nucleic acid testing negative. Transfusion. 2020;60:1476–82.
Arase Y, Suzuki F, Suzuki Y, et al. Long-term presence of HBV in the sera of chronic hepatitis B patients with HBsAg seroclearance. Intervirology. 2007;50:161–5.
Lee HS, Yoon JH, Kim CY. Frequent reactivations of anti-HBe-positive chronic hepatitis B in patients with no demonstrable HBV DNA in serum by polymerase chain reaction. Korean J Intern Med. 1995;10:103–7.
Moestrup T, Hansson BG, Widell A, Blomberg J, Nordenfelt E. Hepatitis B virus-DNA in the serum of patients followed-up longitudinally with acute and chronic hepatitis B. J Med Virol. 1985;17:337–44.
Kido S, Ito Y, Nishimura N, Kajita Y, Ozaki T. Human parvovirus B19-associated thrombocytopenic purpura. Acta Paediatr Jpn. 1998;40:486–8.
Rao SP, Miller ST, Cohen BJ. Transient aplastic crisis in patients with sickle cell disease. B19 parvovirus studies during a 7-year period. Am J Dis Child. 1992;146:1328–30.
Acknowledgment
This work was supported by the Natural Science Research Project of Shaanxi Province (no. 2022JM-497)
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
The authors have declared no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The y axis of middle graph of Fig. 2 was corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gong, L., Tian, J., Zhang, Y. et al. Human Parvovirus B19 May Be a Risk Factor in Myasthenia Gravis with Thymoma. Ann Surg Oncol 30, 1646–1655 (2023). https://doi.org/10.1245/s10434-022-12936-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12936-9