Abstract
Although infections are a significant cause of mortality and long-term morbidity of newborns, the early diagnosis of neonatal infections remains difficult. It has been shown recently that up-regulation of CD45RO expression on umbilical cord lymphocytes might be a good indicator for intrauterine viral infections. To evaluate clinical relevance of changes in CD45 isoforms to the diagnosis of neonatal infections, we examined CD45RA and CD45RO expression on total, CD4+, and CD8+ lymphocytes from newborns. Lymphocytes from 55 newborns who were hospitalized in Kiyose Metropolitan Children's Hospital or Yamanashi Medical University Hospital were analyzed. Newborns were classified into three groups according to the possibility of bacterial or viral infection; I (“no” infection, n = 24), II(“possible” infection, n = 17), and III(“definite” infection, n = 14). Results were compared between two of three groups. The CD45RO expression on total or CD4+ lymphocytes in group III (bacterial 12, viral 2) was significantly higher than that in group I or II. Particularly, the CD45RO expression on CD4+ lymphocytes was always greater than 10% in group III, and showed no overlap with the respective value in group I. After termination of infection, the increased CD45RO expression in group III gradually returned to normal levels. These results indicate that not only viral but also bacterial infections trigger transient and reversible changes in CD45 isoform expression by neonatal CD4+ T lymphocytes. This may be a novel marker for the early diagnosis of neonatal infections.
Similar content being viewed by others
Main
The CD45 (leukocyte common antigen) is a family of membrane glycoproteins that are densely expressed by cells of hematopoietic origin(1, 2). At least five human isoforms, ranging in molecular mass from 180 to 220 kD, have been identified(3–11). These isoforms are produced by alternative mRNA splicing of three exons encoded by a single leukocyte common antigen gene(12). Each isoform shares a common intracellular domain having protein tyrosine phosphatase activity, which is involved in T cell activation(13). However, differences in the amino-terminal region of their extracellular domains create unique antigenic determinants. For example, the CD45RA antigen, encoded by exon A, is present in the two largest isoforms with a relative molecular mass of 220 and 205 kD. In contrast, the CD45RO antigen, which is 180 kD in size, lacks sequences encoded by exons A, B, and C(7, 9, 10). Although individual lymphocytes simultaneously express more than one CD45 isoform, the CD45RA and CD45RO antigens are largely reciprocally expressed by subsets of T cells with distinct functions and activation requirements(4, 13–16).
When stimulated with mitogens such as phytohemagglutinin or concanavalin A in vitro, CD45RA+ T cells lose CD45RA expression and gain CD45RO expression(5, 8, 17, 18). In vivo, the vast majority (>90%) of T lymphocytes present in umbilical cord blood express CD45RA antigen, but not CD45RO antigen. During childhood, the relative frequency of circulating CD45RA+ cells gradually declines, and the frequency of CD45RO+ cells increases, reaching 40-60% in adults(19, 20). Based on these in vitro and in vivo data, it has been proposed that CD45RA expression is characteristic of unprimed or naive T lymphocytes, whereas the CD45RO expression is characteristic of primed or memory T lymphocytes(1–22). However, several works(8, 17, 21, 23) have demonstrated that CD45 isoform expression does not directly correlate with maturational status of T lymphocytes, both in vitro and in vivo, and that individual T lymphocytes alter their isoform expression in a highly regulated manner during thymic selection and upon antigen exposure in the periphery.
Regardless, it has been clinically shown that the proportion of CD45RO+ T lymphocytes markedly increases in association with several specific viral infections, autoimmune diseases, or granulomatosis processes(24–30). Furthermore, it was recently suggested that up-regulation of CD45RO expression on umbilical cord lymphocytes might be a good indicator of congenital viral infections(31).
Infections are a significant cause of mortality and long-term mobility of newborns, which occur during intrauterine development, in association with the birth process, or in the first postnatal days or weeks. The prognosis of these diseases can be improved if recognized early and if appropriate therapy is promptly instituted, particularly in the case of bacterial infections. However, successful therapy, at least in part, must depend upon the physicians' clinical experience, because the early diagnosis of neonatal infections is often difficult(32–37). Thus, a novel marker for the early diagnosis of neonatal infections is needed.
In the present study, we examined the CD45RA and CD45RO expression on total, CD45+, and CD8+ lymphocytes from newborns, and found a significant increase in CD45RO expression, particularly on CD4+ T lymphocytes, in neonatal infections. This change was transient and returned to normal levels after recovery from the disease. Clinical relevance of transient changes in CD45 isoform expression to the early diagnosis of neonatal infection is discussed.
METHODS
Patients and samples. Studies were made of 55 newborns who were hospitalized in Kiyose Metropolitan Children's Hospital or Yamanashi Medical University Hospital. None of the newborns showed severe fetal distress or neonatal asphyxia. These newborns were classified into three groups according to the possibility of bacterial or viral infection, based on the following criteria: I, “no” infection group: showed neither clinical symptoms suspicious of infection such as fever, hypothermia, dyspnea, tachypnea, cyanosis, vomiting, abdominal distention, poor sucking, and petechiae, nor laboratory data suspicious of infection such as CRP ≥ 0.3 and/or IgM ≥ 20 mg/dL; II, “possible” infection group: showed symptoms and/or laboratory and radiographic findings suspicious of infection, but no causative agent was isolated from blood, CSF, urine, intratracheal or gastric aspirate, or stool; and III, “definite” infection group: showed symptoms and/or laboratory and radiographic findings suspicious of infection, and a causative agent was isolated. The case in which CSF showed pleocytosis but no pathogen was isolated was also included in group III(aseptic meningitis). The bacteria isolated were considered as the causative pathogen when colonies were formed of more than 105/mL in urine, and when a single agent was exclusively isolated from intratracheal or gastric aspirate, or stool. A total 63 peripheral blood samples from 55 newborns were collected according to the informed consent guidelines of the medical ethics committee of both hospitals. First samples were obtained 7 d or less after birth. In some patients, samples were obtained at various intervals.
MAbs. PE-conjugated MAb reactive with CD3 (T3), CD4 (T4), CD8(T8), and FITC-conjugated mAbs reactive with CD45RA (2H4) and CD45RO (UCHL-1) were used. All mAbs were purchased from Coulter Immunology (Hialah, FL), except for UCHL-1, which was from DAKO A/S (Glostrup, Denmark).
Phenotypic analysis. PBMC were separated by Ficoll-Hypaque density gradient sedimentation from 1 mL of heparinized blood, obtained by routine venipuncture, and were incubated with FITC- and PE-conjugated MAb for 30 min on ice. After washing with PBS, reactivity of MAb was analyzed on the gated lymphocyte population using a flow cytometer (EPICS Profile Analyzer, Coulter Electronics) as shown in Figure 1A. The method of two-color analysis (PE on the vertical axis versus FITC on the horizontal axis) have been described previously(21).
Flow cytometric analysis. (A) The forward× side plot on the gated lymphocyte population. PBMC obtained from peripheral blood by Ficoll-Hypaque density gradient sedimentation were applied to a flow cytometer. Reactivity of mAbs was analyzed on the gated lymphocyte population as shown in the forward scatter (FS) × the lateral side scatter (LSS) plot. (B) Two-color fluorescence histogram of CD4 and CD45RO. PBMC of case 20 from group I (left) and case 52 from group III (right) were stained with anti-CD4-PE and anti-CD45RO-FITC, and analyzed on a flow cytometer. (CD4 expression on the vertical axis vs CD45RO expression on the horizontal axis.)
Western blot analysis. The procedure has been described previously(38, 39). Briefly, PBMC obtained from several newborns were lysed in buffer (50 mM Tris-HCl, pH 8.0, containing 1% Nonidet P-40, 150 mM NaCl, 0.05% NaN3, 5 mM EDTA, 1 mM phenylmethylsulfonyl fluoride, 0.2 trypsin-inhibiting unit/mL aprotinin, 1μg/mL pepstatin A, and 10 mM iodoacetamide) for 30 min on ice. The lysates were run on a 5.5% SDS-polyacrylamide gel under reducing conditions and transferred to nitrocellulose membranes. Membranes were incubated overnight at room temperature with anti-CD45RO MAb (UCHL-1, 1 μg/mL), and then incubated with alkaline phosphatase-labeled rabbit anti-mouse IgG (Promega, Madison, WI) for 1 h. The bands were developed with nitro blue tetrazolium and 5-bromo-4-chloro-3-indolyl phosphate (Promega).
Statistical analysis. Comparison between two of three groups was performed using a χ2 test or ANOVA in Stat-View programs(Abacus Concepts, Inc., Berkeley, CA). A value (Fisher's exact test or Scheffe's F) of p < 0.05 was considered as significant.
RESULTS
Clinical and laboratory features. Twenty-four newborns (male 13, female 11) were classified into group I (no infection; cases 1-24), 17 newborns (male 9, female 8) into group II (possible infection; cases 25-41), and 14 newborns (male 5, female 9) into group III (definite infection; cases 42-55) according to the criteria described in “Methods.” In group III, 12 newborns were diagnosed as having bacterial infection (sepsis 4, colitis 3, meningitis 2, pneumonia 2, urinary tract infection 1) and two as having viral infection (Coxsackie virus B3 1, unknown 1). Etiologic pathogens in bacterial infection were as follows: Staphylococcus aureus 4,γ-streptococcus 2, Escherichia coli 2, Pseudomonas aeruginosa 1, Staphylococcus epidermidis 1, Staphylococcus faecalis 1, and Listeria monocytogenes 1. As summarized in Table 1, there was no significant difference between two of three groups in sex, gestational age, body weight, APGAR score, incidence of small for dates, and sampling day. However, incidence of premature rupture of the membranes was significantly higher in group II than in group I(p = 0.04). Regarding hematologic data, Hb and platelets were significantly decreased in group III (Hb, I versus III: p= 0.04; platelets, I versus III: p < 0.01), whereas there was no significant difference in white blood cells, neutrophil (%), lymphocytes (%), IgG, IgA, and IgM between two of three groups. CRP was significantly increased in group III (versus I or II, p< 0.01). These results suggest that low Hb and platelet in addition to high CRP might be useful for laboratory evaluation of neonatal infection. However, it should be noted that decrease in Hb was very small in almost all cases, and an apparent decrease in platelet count (<100 × 109/L) was observed only in half of the cases in group III, and that elevated CRP levels were not always observed in group III (cases 44 and 49).
The expression of surface antigens. First, CD3, CD4, and CD8 expression were compared between two of three groups as shown in Figure 2. The CD3 expression (I: 74.6 ± 13.3%, II: 69.1 ± 14.1%, III: 74.5 ± 13.9%), the CD4 expression (I: 62.1± 15.7%, II: 56.6 ± 22.8%, III: 65.2 ± 15.2%), and the CD8 expression (I: 20.9 ± 8.4%, II: 24.1 ± 12.7%, III: 27.2± 9.2%) showed no significant difference. There was also no significant difference in the CD4/CD8 ratio between two of three groups (I: 4.0 ± 2.9%, II: 3.5 ± 3.5%, III: 2.8 ± 1.3%).
Next, the CD45RA expression on total, CD4+, and CD8+ lymphocytes was compared. As shown in Figure 3, the CD45RA expression on total lymphocytes in group III (65 ± 8.8%) was significantly lower than that in group I (80.6 ± 8.6%) or group II(75.0 ± 13.9%). However, the CD45RA expression on CD4+ or CD8+ lymphocytes showed no statistical difference between two of three groups (CD4, I: 50.4 ± 16.5%; II: 42.7 ± 20.3%; III: 41.1± 16.5%; CD8, I: 17.4 ± 6.9%; II: 18.1 ± 8.8%; III: 18.5± 6.2%). These results suggest that low CD45RA expression on total lymphocytes in group III may reflect a decrease in CD45RA expression on CD4-CD8- T lymphocytes, natural killer cells, or B cells.
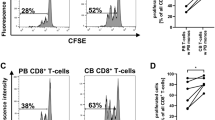
Third, the CD45RO expression on total, CD4+, and CD8+ lymphocytes was evaluated. As shown in Figure 4, the CD45RO expression on total lymphocytes in group III (27.1 ± 14.0%) was significantly higher than that in group I (7.1 ± 2.7%) or group II(13.5 ± 8.9%). The CD45RO expression on CD4+ or CD8+ lymphocytes was also significantly highest in group III (CD4, I: 4.5 ± 2.2%, II: 9.1 ± 6.5%, III: 18.6 ± 9.6%; CD8, I: 1.1 ± 0.7%, II: 3.1 ± 4.4%, III: 7.9 ± 10.1%). It should be noted that the CD45RO expression on CD4+ lymphocytes was always greater than 10% in group III, and showed no overlap with the respective value in group I. Representative two-color analysis on CD45RO versus CD4 expression in groups I and III is shown in Figure 1B. Of clinical importance, among newborns belonging to group II, the CD45RO expression on CD4+ T lymphocytes from six cases was markedly increased and was almost similar to that of the mean in group III as shown in Figure 4, suggesting “definite” infection in these cases.
Finally, there was no difference in each antigen expression between small for date and appropriate for date newborns, which was statistically confirmed in newborns belonging to group I (data not shown). No significant changes were also demonstrated in group I when the CD45 isoform expression was compared between newborns of early sampling <3 d and those of later sampling ≥3 d(data not shown).
The temporal changes in CD45RA and CD45RO expression on total lymphocytes along the clinical course was evaluated in three and five newborns from groups II and III, respectively. Second samples were obtained 14 d or more after birth, at a time they were recovered and showed few clinical symptoms. As shown in Figure 5, the decreased CD45RA expression seen 7 d or less after birth in the three newborns belonging to group III (cases 43, 50, and 51) increased back toward normal levels after recovery from infection. Conversely, the increased CD45RO expression in five newborns from group III returned toward normal levels 14 d or more after birth. There were no significant changes in either CD45RA or CD45RO expression in three newborns from group II over the same time period (although a small increase in CD45RA expression was observed in case 26). These results suggested that a decrease in CD45RA expression and an increase in CD45RO expression in group III are transient.
Temporal changes in CD45RA and CD45RO expression on total lymphocytes. CD45RA and CD45RO expression on total lymphocytes 7 d or less and 14 d or more after birth was compared in three newborns from groups II (open symbols) and five newborns from group III (filled symbols). Thre were no significant changes in the CD45RA and CD45RO expression over time in group II except for a small increase in CD45RA expression in case 26.
To further evaluate changes in CD45RO expression, lysates from PBMC obtained from several newborns were run on a 5.5% SDS-polyacrylamide gel and blotted to nitrocellulose. CD45RO expression was analyzed using anti-CD45RO MAb as described in “Methods.” As shown in Figure 6, the CD45RO antigen (180 kD) was not visualized in the lysates from newborns belonging to group I (cases 19, 22, and 24), whereas the 180-kD band was clearly detected in the lysates from those belonging to group III (cases 50 and 51) on d 2 and 6 after birth, but almost disappeared in lysates on d 18 and 14, respectively. It appears that this Western blot analysis can detect the population expressing CD45RO only at high levels. Similar experiments examining CD45RA expression could not be performed due to the inability of anti-CD45RA MAb to recognize its antigen on Western blots.
Analysis of CD45RO expression on Western blot. The CD45RO expression in cell lysates from PBMC of three neonates from group I(lanes 1-3) and two newborns from group III (lanes 4-7) was analyzed as described in “Methods.” Samples were obtained 7 d or less (lanes 1-4 and 6) and 14 d or more (lanes 5 and 7) after birth.
As a representative example, the clinical course and changes in surface antigen expression of a female newborn (case 43) from group III is shown in Figure 7. She developed frequent apnea within a few hours of birth. Laboratory data revealed high white blood cells (32.7 × 109/L) and CRP (2.5 mg/dL), but no elevation of IgM. The leukocyte count in CSF was 8.0 × 109/L, and Listeria monocytogenes was subsequently demonstrated in both blood and CSF. Intravenous administration of ampicillin, gentamicin, and vancomycin was started, and she recovered completely at 1 mo from the onset of symptoms. Serial examination of surface antigens expression revealed that the CD45RA expression on total lymphocytes was only 24.0% on d 2, but gradually increased throughout the clinical course, reaching 82.5% on d 50. In contrast, CD45RO expression was markedly up-regulated (48.6%) on d 2, but decreased to 12.0% on d 50.
Representative clinical course and changes in surface antigens in a neonate (case 43) from group III. Laboratory examination, CSF analysis, and analysis of surface antigen expression on lymphocytes were performed serially. Abbreviations: VCM, vancomycin; GM, gentamicin; AB-PC, ampicillin; WBC, white blood cell.
DISCUSSION
Diagnosis of neonatal infection is generally known to be difficult because newborns suffering from infections show few specific symptoms, and because availability of samples for laboratory diagnosis is limited. Moreover, although peripheral blood cell counts, IgM, CRP, granulocyte/colony-stimulating factor, and so forth have been used as tools for laboratory evaluation of neonatal infection, these are not always reliable and satisfactory as reported previously(32–37). Thus, the transient changes in CD45 isoforms, in particular the increased CD45RO expression on CD4+ T lymphocytes presented in this study, might shed new insights into evaluation of neonatal infection and possibly provide a useful tool for the early diagnosis of neonatal infection.
Recently, there have been a number of reports describing changes in the CD45 isoform expression in association with specific viral infections. It was reported that the percentage of CD45RA+ T lymphocytes decreased and the percentage of CD45RO+ T lymphocytes, particularly CD4+ lymphocytes, increased, when cultured in vitro with human cytomegalovirus(40). Clinically, the CD8+ CD45RO+ population was reported to markedly expand in peripheral blood from patients with infection due to EBV, HIV-1, or hepatitis B virus(24, 26, 29). Thus, it is now evident that the CD45RO expression on T lymphocytes is up-regulated after particular viral infections. We showed that neonatal CD45RO+ T lymphocytes increased by not only viral but also bacterial infections. Concomitantly, CD45RA expression on neonatal lymphocytes was significantly decreased. It is thought that, in adults, a small increase in CD45RO expression after bacterial infection is difficult to detect because the CD45RO antigen is highly expressed on T lymphocytes before the present infection. On the other hand, a small increase in CD45RO expression is expected to more easily be detected in neonatal T lymphocytes because of its low basal levels of expression. Similarly, because the vast majority of T lymphocytes from newborns express the CD45RA antigen, a small decrease in CD45RA expression might be detected after infection. Of clinical importance, there was no overlap of CD45RO on CD4+ T lymphocytes expression between groups I and III. Further examination in additional newborns will be required to confirm its clinical utility.
Our data demonstrated that neonatal T lymphocytes underwent phenotypic conversion from CD45RA+ to CD45RO+ after infectious“stimulation.” Of interest, changes in the CD45RA and CD45RO expression were transient and reversible in infected newborns. Although its precise process is unclear at present, both or either mechanisms,“clonal reconstitution” and “phenotypic reconversion,” can be postulated because it is reported that the life span of CD45RO+ lymphocytes is shorter than that of CD45RA+ lymphocytes, presumably due to the apoptotic process(41, 42). Furthermore, the population originally CD45RA+ can reconvert from the CD45RO phenotype to the CD45RA phenotype after the stage of stimulation(8, 21, 43).
The mechanisms by which the T cell receptor triggering affects the negative regulatory splicing factors that regulate CD45 alternative splicing is unknown(16). It is also unclear what influences the alternative splicing pattern in T lymphocytes during the process of infection. In addition to T cell receptor triggering, changes in levels and repertoire of cytokines and intercellular ligand counter-ligand interactions induced by infection may be involved in this process. Newborn PBMC are known to produce equivalent amounts of IL-2, but less interferon-γ and IL-4, than adult PBMC in response to polyclonal activators, such as staphylococcal enterotoxin B(44, 45). It is also reported that exposure of purified CD45RA+ T lymphocytes to IL-2 promotes their phenotypic conversion to CD45RO+(46), suggesting a crucial role of IL-2 in infection-associated phenotypic conversion of neonatal T lymphocytes. Thus, it is conceivable that the transient expression of particular CD45 isoforms plays an important role in development of the functional repertoire required for appropriate regulatory or effector functions of the immune responses after infections.
Abbreviations
- PE:
-
phycoerythrin
- PBMC:
-
peripheral blood mononuclear cell
- CRP:
-
C-reactive protein
References
Thomas ML, Lefrancois L 1988 Differential expression of the leukocyte-common antigen family. Immunol Today 9: 320–326.
Thomas ML 1989 The leukocyte common antigen family. Annu Rev Immunol 7: 339–369.
Pulido R, Sanchez MF 1989 Biochemical nature and topographic localization of epitopes defining four distinct CD45 antigen specificities. Conventional CD45 CD45R, 180 kDa (UCHL1) and 220/205/190 kDa. J Immunol 143: 1930–1936.
Smith SH, Brown MH, Rowe D, Callard RE, Beverley PCL 1986 Functional subsets of human helper-inducer cells defined by a new monoclonal antibody, UCHL-1. Immunology 58: 63–70.
Akbar AN, Terry L, Timms A, Beverley PC, Janossy G 1988 Loss of CD45R and gain of UCHL1 reactivity is a feature of primed T cells. J Immunol 140: 2171–2178.
Rudd CE, Morimoto C, Wong LL, Schlossman SF 1987 The subdivision of the T4 (CD4) subset on the basis of the differential expression of L-C/T200 antigens. J Exp Med 166: 1758–1773.
Streuli M, Matsuyama T, Morimoto C, Schlossman SF, Saito H 1987 Identification of the sequence required for expression of the 2H4 epitope on the human leukocyte common antigens. J Exp Med 166: 1567–1572.
Rothstein DM, Yamada A, Schlossman SF, Morimoto C 1991 Cyclic regulation of CD45 isoform expression in a long term human CD4+CD45RA+ T cell line. J Immunol 146: 1175–1183.
Streuli M, Hall LR, Saga Y, Schlossman SF, Saito H 1987 Differential usage of three exons generates at least five different mRNAs encoding human leukocyte common antigens. J Exp Med 166: 1548–1566.
Streuli M, Morimoto C, Schrieber M, Schlossman SF, Saito H 1988 Characterization of CD45 and CD45R monoclonal antibodies using transfected mouse cell lines that express individual human leukocyte common antigens. J Immunol 141: 3910–3914.
Terry LA, Brown MH, Beverley PC 1988 The monoclonal antibody, UCHL1, recognizes a 180:000 MW component of the human leucocyte-common antigen, CD45. Immunology 64: 331–336.
Akao Y, Utsumi KR, Naito K, Ueda R, Takahashi T, Yamada K 1987 Chromosomal assignments of genes coding for human leukocyte common antigen, T-200, and lymphocyte function-associated antigen 1, LFA 1 β submit. Somat Cell Mol Genet 13: 273–278.
McKenney DW, Onodera H, Gorman L, Mimura T, Rothstein DM 1995 Distinct isoforms of the CD45 protein-tyrosine phosphatase differentially regulate interleukin 2 secretion and activation signal pathways involving. J Biol Chem 270: 24949–24954.
Morimoto C, Letvin NL, Distaso JA, Aldrich WR, Schlossman SF 1985 The isolation of characterization of the human suppresser inducer T cell subset. J Immunol 134: 1508–1515.
Onodera H, Motto DG, Koretzky GA, Rothstein DM 1996 Differential regulation of activation-induced tyrosine phosphorylation and recruitment of SLP-76 to vav by distinct isoforms of the CD45 protein-tyrosine phosphatase. J Biol Chem 271: 22225–222230.
Rothstein DM, Saito H, Streuli M, Schlossman SF, Morimoto C 1992 The alternative splicing of CD45 tyrosine phosphatase is controlled by negative regulatory transcting splicing factors. J Biol Chem 267: 7139–7147.
Rothstein DM, Sohen S, Daley JF, Schlossman SF, Morimoto C 1990 CD4+CD45RA+ and CD4+CD45RA- T cell subsets in man maintain distinct function and CD45RA expression persists on a subpopulation of CD45RA+ cells after activation with Con A. Cell Immunol 129: 449–467.
Newman I, Wilkinson PC 1993 Locomotor responses of human CD45 lymphocyte subsets: preferential locomotion of CD45RO+ lymphocytes in response to attractants and mitogens. Immunology 78: 92–98.
Tedder TF, Clement LT, Cooper MD 1985 Human lymphocyte differentiation antigen HB-10 and HB-11.I. Ontogeny of antigen expression. J Immunol 134: 2983–2988.
De PP, Battistin S, Santini GF 1988 Age-related changes in human lymphocyte subsets: progressive reduction of the CD4 CD45R(suppresser inducer) population. Clin Immunol Immunopathol 48: 290–296.
Sugita K, Hirose T, Rothstein DM, Donahue C, Schlossman SF, Morimoto C 1992 CD27, a member of the nerve growth factor receptor family, is preferentially expressed on CD45RA+ CD4 T cell clones and involved in distinct immunoregulatory functions. J Immunol 149: 3208–3216.
Ikeda M, Takahashi H, Yoshida S 1994 HLA-DR+CD3+ and CD8+ cells are increased but CD4+CD45RA+ cells are reduced in the peripheral blood in human scrub typhus. Clin Immunol Immunopathol 72: 402–404.
Bell EB, Sparshott SM 1990 Interconversion of CD45R subsets of CD4 T cells in vivo. Nature 348: 163–166.
Miyawaki T, Kasahara Y, Kanegane H, Ohta K, Yokoi T, Yachie A, Taniguchi N 1991 Expression of CD45R0 (UCHL1) by CD4+ and CD8+ T cells as a sign of in vivo activation in infectious mononucleosis. Clin Exp Immunol 83: 447–451.
Pinto L, Covas MJ, Victorino RM 1991 Loss of CD45RA and gain of CD45RO after in vitro activation of lymphocytes from HIV-infected patients. Immunology 73: 147–150.
Jung MC, Schraut W, Santantonio T, Spengler U, Eichenlaub D, Eisenburg J, Zachoval R 1993 Increased frequency of CD8+ CD45R0+ memory T lymphocytes in acute hepatitis B virus infection. J Hepatol 18: 295–300.
Fiszer U, Mix E, Fredrikson S, Kostulas V, Link H 1994 Parkinson's disease and immunological abnormalities: increase of HLA-DR expression on monocytes in cerebrospinal fluid and of CD45RO+ T cells in peripheral blood. Acta Neurol Scand 90: 160–166.
Karlsson MG, Davidsson A, hellquist HB 1994 Increase in CD4+ and CD45RO+ memory T cells in the nasal mucosa of allergic patients. APMIS 102: 753–758.
Kestens L, Vanham G, Vereecken C, Vandenbruaene M, Vercauteren G, Colebunders RL, Gigase PL 1994 Selective increase of activation antigens HLA-DR and CD38 on CD4+ CD45RO+ T lymphocytes during HIV-1 infection. Clin Exp Immunol 95: 436–441.
Fazel SB, Howie SE, A. Krajewski S, Lamb D 1994 Increased CD45RO expression on T lymphocytes in mediastinal lymph node and pulmonary lesions of patients with pulmonary sarcoidosis. Clin Exp Immunol 95: 509–513.
Michie C, Harvey D 1994 Can expression of CD45RO, a T-cell surface molecule, be used to detect congenital infection? [see Comments]. Lancet 343: 1259–1260.
Klaus MH, Avroy A 1986 Care of the High Risk Neonate. Ardmore Medical Books, Philadelphia, pp 262–285.
Philip AG, Hewitt JR 1980 Early diagnosis of neonatal sepsis. Pediatrics 65: 1036–1041.
Kennon C, Overturf G, Bessman S, Sierra E, Smith KJ, Brann B 1996 Granulocyte colony-stimulating factor as a marker for bacterial infection in neonates. J Pediatr 128: 765–769.
Squire E, Favara B, Todd J 1979 Diagnosis of neonatal bacterial infection: hematologic and pathologic findings in fatal and non fatal cases. Pediatrics 64: 60–64.
Jahnk S, Bartiromo G, Maiseles MJ 1985 The peripheral white blood cell count in the diagnosis of neonatal infection. J Pediatr 5: 50–56.
Greenberg DN, Yoder BA 1990 Changes in differential white blood cell count in screening for group B streptococcal sepsis. Pediatr Infect Dis J 9: 886–889.
Kojika S, Sugita K, Inukai T, Saito M, Iijima K, Tezuka T, Goi K, Shiraishi K, Mori T, Okazaki T, Kagami K, Ohyama K, Nakazawa S 1996 Mechanisms of glucocorticoid resistance in human leukemic cells: implication of abnormal 90 and 70 kDa heat shock protein. Leukemia 10: 994–999.
Inukai T, Sugita K, Suzuki T, Iijima K, Goi K, Tezuka T, Kojika S, Hatakeyama K, Kagami K, Mori T, Okazaki T, Mizutani S, Nakazawa S 1993 A novel 203 kD aberrant BCR-ABL product in a girl with Philadelphia chromosome positive acute lymphoblastic leukemia. Br J Hematol 85: 823–825.
Nakano T, Ito M, Mizuno T, Mizutani K, Ihara T, Kamiya H, Sakurai M 1993 Increase of interleukin 2 receptor and CD45RO antigen on lymphocytes cultured with human cytomegalovirus. Cell Immunol 147: 73–80.
Michie CA, McLean A, Alcock C, Beverley PC 1992 Lifespan of human lymphocyte subsets defined by CD45 isoforms. Nature 360: 264–265.
Uehara T, Miyawaki T, Ohta K, Tamura Y, Yokoi T, Nakamura S, Taniguchi N 1992 Apoptotic cell death of primed CD45RO+ T lymphocytes in Epstein-Barr virus-induced infectious mononucleosis. Blood 80: 452–458.
Morimoto C, Schlossman SF 1993 P. Rambotti Lecture. Human naive and memory T cells revisited: new markers (CD31 and CD27) that help define CD4+ T cell subsets. Clin Exp Rheumatol 11: 241–247.
Anthony H, Mary C 1994 Proliferative and Cytokine Responses by Human Newborn T Cells stimulated with staphylococcal enterotoxin B. Pediatr Res 35: 293–298.
Wilson CB, Westall J, Johnston L, Lewis DB, Dower SK, Alpert AR 1986 Decreased production of interferon-γ by human neonatal cells. Intrinsic and regulatory deficiencies. J Clin Invest 77: 860–867.
Michael DR 1994 Interleukin 2 induces the expression of CD45RO and the memory phenotype by CD45RA+ peripheral blood lymphocytes. J Exp Med 179: 857–864.
Acknowledgements
The authors thank Dr. David M. Rothstein(Department of Internal Medicine, Section of Nephrology, Yale University School of Medicine, New Haven, CT) for critical reading of the manuscript and for helpful suggestions.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tezuka, T., Sugita, K., Mizobe, N. et al. Transient Increase in CD45RO Expression on T Lymphocytes in Infected Newborns. Pediatr Res 43, 283–290 (1998). https://doi.org/10.1203/00006450-199802000-00021
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199802000-00021
- Springer Nature America, Inc.