Abstract
Background
Among various body weight-supported locomotor training methods for neurological patients, some studies have recognized the lower body positive pressure (LBPP) treadmill as superior for gait training in neurological patients. The aim of this study is to explore the clinical use and efficacy of LBPP treadmill gait training in neurological patients.
Methods
A systematic review was performed following PRISMA guidelines. The inclusion criteria were studies published in English using LBPP with neurological patients were included from the database's inception to March 2023 to avoid misinterpretation of translation. The search was conducted in multiple databases, including Google Scholar, PubMed, Scopus, PEDro, and the Cochrane Database. To improve accuracy and comprehensiveness, studies mentioned in the main articles were also evaluated.
Results
The search identified 16 articles that use LBPP with neurological patients. Only a few randomized control studies on the use of LBPP after stroke have been reported. For neurological rehabilitation, LBPP treadmill gait training is safe and feasible. Current research suggests that using the LBPP treadmill in conjunction with traditional rehabilitation treatment has a successively beneficial impact on motor function, particularly in patients with subacute to chronic stroke and Parkinson’s disease. There are no studies that compare the LBPP to the body weight supported treadmill (BWST). Furthermore, to the best of our knowledge, the LBPP treadmill has not yet been evaluated on for its effectiveness in treating traumatic brain injury (TBI) or spinal cord injury (SCI).
Conclusion
There was insufficient evidence to support the claim that LBPP is effective and superior to other gait training methods. Larger randomized control studies with sufficient sample sizes are needed to better understand the potential effects of the LBPP treadmill intervention on the functional performance of people with neurological disorders.
Similar content being viewed by others
Introduction
Individuals with neurological impairments, such as stroke, Parkinson’s disease (PD), spinal cord injury (SCI), multiple sclerosis (MS), cerebral palsy (CP), or traumatic brain injury (TBI), often experience lasting locomotor deficits, including decreased gait speed and endurance as well as increased gait energy cost [1]. The consequences of immobility for individuals with neurological impairments are numerous. Patients with neurological impairments have an increased risk of severe restrictions on daily life, an increased risk of falling, and a diminished quality of life [1]. Therefore, improving walking ability is a major goal in neurological rehabilitation [2, 3]. In the twenty-first century, several novel locomotor training tools were developed to provide task-oriented practice with high repetitions for individuals with neurological impairments [4]. These tools have the potential to enhance recovery of locomotion and physical and cardiorespiratory fitness [5], reduced spasticity, improved balance, and increased bone density [6].
Locomotor training can be performed in a variety of sitting including overground [7], underwater [8], on a robot [9, 10], or on a treadmill [11, 12]. Treadmill and robotic gait training allow for greater repetition of step** in a safe, controlled environment and with greater intensity than overground gait training [13]. However, it is important to perform symmetrical and physiological walking to appropriately stimulate the locomotor centers and, consequently, activate the paralyzed muscle [14]. Most often, a body weight supported treadmill (BWST) utilizes an overhead harness to unload the patient’s weight. Two to three physical therapists are needed for gait training with a BWST. However, patients often do not feel comfortable using the overhead harness due to the straps’ pressure points, which may reduce the duration of the training sessions [15].
BWST and the robotic exoskeleton have been shown to improve gait function compared to overground. However, the effects of these interventions are still being debated [16, 17]. Recently, a new gait training method called lower body positive pressure (LBPP) treadmill gait training has been developed. LBPP treadmill (Fig. 1) has been extensively investigated as a method of gait training [18,19,20]. LBPP treadmills use air pressure to support the patient's weight, allowing them to walk with less effort [15]. One of the advantages of LBPP treadmill gait training is that it applies even air pressure to the lower extremity. This helps to maintain normal muscle activation and gait patterns [20, 21]. LBPP has the potential to be a superior gait training method compared to other body weight supported locomotor training methods [20, 21].
National Aeronautics and Space Administration (NASA) develop the antigravity treadmill as a technique for astronauts to maintain fitness in space [22]. In January 2008, the U.S. Food and Drug Administration (FDA) approved the G-Trainer (LBPP) for medical use. The LBPP apparatus consists of a treadmill within a waist-high chamber, an air compressor, and a monitoring screen. When the air compressor raises the pressure in the chamber above atmospheric pressure, it creates an axial buoyant force that is proportional to the patient’s cross-sectional area. This pressure reduces patient weight loading and allows for gait training [23, 24]. The safety and feasibility of the LBPP procedure has been investigated in healthy individuals [24, 25], orthopedic patients [18, 19], and neurological patients [18,19,20, 26,27,28].
LBPP is a locomotor training approach that can be used to facilitate postoperative rehabilitation after knee surgery and lower-limb athletic injuries. It can also be used to minimize ground reaction forces during walking or running [18, 29, 30]. LBPP technology can efficiently and safely reduce body weight and relieve knee pain during weight-bearing exercise in overweight knee osteoarthritis (OA) patients [29]. Furthermore, LBPP has recently been used as a rehabilitation tool for neurological patients [8, 20, 31,32,33,34,35,36]. However, the present evidence regarding its clinical use and efficacy in the neurological population with locomotor deficits is insufficient. Furthermore, no synthesis has been produced, which could play an essential role in guiding future research. Therefore, this review aims to explore the clinical use and efficacy of LBPP gait training in neurological patients.
Methods
Data source and literature search
This review followed the PRISMA guidelines [37] and used an internet-based search to identify relevant studies. The search was conducted on multiple databases, including PubMed, Scopus, PEDro, the Cochrane Database, and Google Scholar. The search strategy was built on the following keywords: lower body positive pressure, antigravity treadmill, stroke, cerebrovascular accident, spinal cord injury, Parkinson’s disease, and multiple sclerosis. These keywords were used either separately or in combination with other search terms.
Eligibility criteria
The studies included in the review were experimental studies that used the LBPP treadmill on neurological patients. The studies were published in English from the inception of the database until March 2023 to avoid misinterpretation due to translation. The following types of studies were included in the review: randomized control trials (RCTs), pre- and post-studies, and case studies.
Study screening
The studies were screened for eligibility in two stages. In the first stage, the titles and abstracts of the studies were screened to identify those that met the inclusion criteria. In the second stage, the full-text articles of the studies that were identified in the first stage were screened to determine if they met the eligibility criteria. The reference lists of the included studies were also screened to identify any additional relevant studies. The search strategy employed in this study was comprehensive and systematic, ensuring that all relevant literature was included. The identified studies were critically appraised to assess their quality and relevance to the research question.
Quality assessment
The overall quality of each article included in the study was rated using the PEDro scale. The PEDro scale is a validated tool for assessing the methodological quality of randomized controlled trials. It has 10 items, and each item is scored as either “yes,” “no,” or “not applicable.” The total score for each study ranges from 0 to 10, with higher scores indicating higher methodological quality.
Results
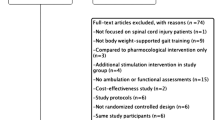
We conducted a systematic literature review to identify all relevant studies on the efficacy of LBPP gait training in neurological patients. We searched six databases: PubMed, Cochrane, PEDro, Google Scholar, and reference lists. The initial search yielded 793 articles. We excluded 420 articles due to duplication, leaving 373 articles. We screened the titles and abstracts of these articles and excluded 339 articles that did not meet our inclusion criteria. We then assessed the full texts of the remaining 34 articles and excluded 18 articles that did not meet our inclusion criteria. A total of 16 articles met our inclusion criteria and were included in the final analysis [8, 12, 20, 28, 32,33,34,35,36, 38,39,40,41,42,43,44]. The results of the search and selection process are summarized in a PRISMA flowchart diagram (Fig. 2).
Lower body positive pressure treadmill gait training after stroke
Table 1 provides a summary of the nine studies for stroke patients with a PEDro rating score for RCT studies. Nine studies were identified using a LBPP treadmill with stroke. Five of these studies were RCTs that were performed on 177 stroke patients [8, 20, 33, 34, 36]. The methodological quality of the RCTs ranged from 6 to 8 out of 10 on the PEDro scale, with a high quality (PEDro score ≥ 6). The other studies were an exploratory study [28], a prospective cohort study [31], and two case studies [32, 35] performed on 20 stroke patients. All the included studies did not report adverse events and reported improvements in balance and gait following LBPP training.
Lower body positive pressure treadmill training after Parkinson’s disease
Table 2 summarizes six studies on Parkinson's disease patients using a LBPP treadmill. The studies were exploratory and pre- and post-studies, and performed on 63 participants. None of the studies were RCTs [38,39,40,41,42,43]. All the included studies did not report adverse events and reported improvements in balance and gait following LBPP training, except one study [41], which did not report improvements in balance and gait.
Lower body positive pressure treadmill training after other neurological diseases
Only a pre- and post-study has investigated the effects of LBPP gait training on 6 MS patients (Table 3) [44]. In this study, LBPP increased muscle oxidative capacity and endurance, but did not improve walking ability. To the best of our knowledge, the use of LBPP treadmills for traumatic brain and spinal cord injuries has not yet been studied.
Discussion
In this review, articles on the use of a LBPP treadmill on neurological patients were classified into the follows categories:
Stroke
Stroke is a common neurological disease that can cause permanent disability [45]. The majority of stroke patients experience mobility limitations, such as difficulty walking or maintaining their balance [46]. This can increase the risk of falls and other accidents [47]. The primary goal of rehabilitation after a stroke is to help the patient regain as much function as possible, including the ability to walk independently [3]. A growing body of research has suggested that LBPP gait training may be effective in hel** post-stroke patients improve their walking speed and balance [8, 20, 31,32,33,34,35,36].
In RCT studies, LBPP treadmill gait training was compared to aquatic treadmill gait training, overground gait training, or regular treadmill gait training. These studies assessed the efficacy of the LBPP treadmill on gait parameters, walking ability and endurance, and quality of life. The main findings of the RCTs were that patients with subacute to chronic stroke tolerated LBPP treadmill training well, with no adverse events. Combining LBPP gait training with overground gait training was superior to overground gait training alone on walking ability and endurance in subacute to chronic stroke patients [20]. Particularly, the LBPP treadmill modified the temporal gait variables and muscular activation pattern. Specifically, LBPP increased a time stance, cadence, and stance/swing ratio in the affected limb and increased the gait quality index. Moreover, LBPP induced muscle specific activation (antigravity muscles) and gait cycle-specific compared to overground gait training, which improved overall muscle activation [20].
In subacute to chronic stroke patients, four weeks of LBPP gait training improved standing balance with eyes closed more than overground gait training. However, there were no differences in standing balance with eyes open, walking endurance, muscle activation, or walking ability between groups. According to the study, the average satisfaction score with the LBPP treadmill on a 5-point scale was 4.7 ± 0.61. [33] Oh et al. (2022) [34]. reported that LBPP gait training significantly improved gait score in the Tinetti Performance Oriented Mobility Assessment (POMA) and dynamic balance measured by the Timed Up and Go Test (TUG) compared to overground gait training in chronic stroke patients. However, balance scores in POMA and the Berg Balance Scale (BBS), as well as gait speed measured by the 10-Meter Walk Test (10MWT), did not differ substantially between groups. On the other hand, Park et al. (2018) [8] found that LBPP plus regular treadmill gait training was superior to regular treadmill gait training alone in terms of balance score measured by the BBS and TUG, as well as gait speed as measured by the 10MWT in chronic stroke patients after four weeks of treatment. However, no significant difference was observed between the LBPP and the aquatic gait training.
In a similar study, LBPP gait training plus overground gait training significantly improved maximal heart rate and walking endurance in chronic stroke patients compared to aquatic and overground gait training. As a result, the study suggested that LBPP gait training is beneficial for lowering cardiovascular morbidity and mortality due to a reduction in ventricular repolarization heterogeneity [36]. After 6 weeks of gait training on the LBPP treadmill, chronic stroke patients improved their walking ability measured by functional ambulation category (FAC), comfortable gait speed measured by 10MWT, and walking endurance measured by 6MWT. However, static and dynamic balance, fast gait speed, and quality of life did not change [31].
In summary, according to the available studies, LBPP treadmill gait training is a safe and effective intervention for the rehabilitation of stroke patients. It can improve gait speed, balance, and walking endurance in subacute and chronic stroke patients. The combination of LBPP treadmill gait training and conventional gait training appears to be more effective than conventional gait training alone on gait speed, balance, and walking endurance in subacute and chronic stroke patients. This is likely because LBPP treadmill gait training reduces the patient's body weight, which makes it easier for them to walk. LBPP treadmill gait training also appears to be more effective than aquatic gait training at increasing maximum heart rate and walking endurance. This is likely because aquatic gait training does not reduce the patient's body weight as much as LBPP treadmill gait training. However, there is a lack of comparisons between the LBPP treadmill and the BWST. These findings highlight the significance of incorporating LBPP treadmill gait training into the rehabilitation protocols for subacute to chronic stroke patients. Larger studies with sufficient sample sizes are needed to better understand the potential effects of the LBPP treadmill intervention on the functional performance of people with stroke.
Parkinson’s disease
The pathophysiology of Parkinson's disease may necessitate the use of efficient and safe aerobic exercise. Aerobic exercise is a type of exercise that involves continuous rhythmic motions of the body’s major muscles for extended periods of time, raising the heart rate and calorie requirements [48]. Aerobic exercise has been shown to have superior effects on improving motor and non-motor function in Parkinson’s disease patients [49]. People with Parkinson's disease are advised to only exercise at submaximal work rates with extra safety due to their increased susceptibility to fatigue and falling [50]. In clinical settings, aerobic exercise therapies, especially walking on specialized equipment (such as a treadmill with a safety harness), are commonly implemented [51]. Recently, an alternative of the BWST treadmill has been utilized in Parkinson's patients, such as the LBPP treadmill.
LBPP gait training resulted in a lower submaximal HR in Parkinson's disease patients than land exercises [40]. This indicated a lower cardiovascular strain during exercise, which is especially advantageous for patients with Parkinson’s disease [50]. Therefore, exercising on the LBPP may be a suitable alternative to exercising on land for patients with Parkinson's disease. In a study of 19 Parkinson’s disease patients, the use of the LBPP was found to significantly improve freezing of gait, mobility, balance, and fall risk after 4 weeks of therapy. Additionally, both step length and gait speed have increased [42]. Furthermore, eight weeks of gait training resulted in normalized abnormal flexor peak muscle activation in response to increased body weight support during LBPP gait training [43]. This suggests that LBPP gait training may be an effective way to improve muscle function in Parkinson’s disease patients.
Treadmill gait training with LBPP for eight weeks significantly improved balance in the sagittal plane, such as when rising from a sitting to a standing position. However, it did not improve balance in the transversal or mediolateral plane [38]. This suggests that LBPP gait training may be effective in improving balance in a specific direction, such as the sagittal plane. In another study, LBPP gait training was compared to GlideTrakTM treadmill gait training. LBPP gait training was found to be more effective in improving gait speed, walking endurance, lower extremity muscle strength, dynamic balance, self-reported pain, discomfort, tiredness, tremor, and a feasibility questionnaire [39]. Nevertheless, a third study found that LBPP treadmill exercise did not improve functional assessments of balance, gait, posture, and fine motor skills compared to land and aquatic exercise [41]. Table 2 provides a summary of the six studies that have been conducted on LBPP treadmill exercise for patients with Parkinson’s disease.
In summary, unfortunately, there was not a RCT conducted employing the LBPP for Parkinson's disease. The absence of an RCT limits us from gaining a comprehensive understanding of the possible benefits of utilizing the LBPP treadmill in Parkinson disease patients and leaves a lot of concerns unresolved.
Other neurological diseases
Only one study examined the effects of LBPP gait training on MS. The study evaluated muscle oxidative capacity and muscle endurance as well as their relationship to walking function in moderately to severely affected individuals with MS (Table 3). The study found that LBPP increased gastrocnemius muscle oxidative capacity and endurance, but did improve walking ability [44]. The study’s findings suggest that muscle plasticity may be induced in MS patients by LBPP gait training. However, the improvements in oxidative and endurance capacity of the muscle were not sufficient to improve walking function. More research is needed to determine whether LBPP gait training can be an effective treatment for MS.
Recently, a sco** review that has been published discussed the use of the LBPP for the pediatric population with specific lower limb motor function deficits [52]. The results of the study indicated that LBPP gait training may be viewed as a valuable training modality, particularly for children with cerebral palsy. However, additional research is needed to develop an effective protocol. To the best of our knowledge, the traumatic brain and spinal cord injuries have not been investigated in the LBPP treadmill yet. This gap in research is an area of significant concern, and understanding the effects of LBPP on these injuries could potentially provide new insights into their treatment.
Conclusions
It is imperative that rehabilitation programs for patients with neurological disorders include effective interventions for gait training. Rehabilitation programs for patients with severe neurological impairments require effective interventions for walking restoration. Recent studies indicate that the use of the LBPP in combination with traditional rehabilitation therapy has sequentially beneficial effects on motor function, particularly in subacute to chronic stroke and Parkinson's disease. Patients with stroke and Parkinson's disease appear to benefit more from LBPP treadmill gait training that has a longer duration and is more intense. During gait training, the LBPP treadmill provides more partial assistance and encourages the patient to actively engage their muscles. Recently, the use of LBPP treadmill gait training has been increasingly adopted by health care institutions because of its ability to improve balance performance, promote a task-oriented gait, and minimize the risk of falling.
Although LBPP treadmill gait training has been found to be an effective treatment for neurological patients, many limitations have been identified. The hustle to get on and off the LBPP treadmill can be difficult for patients with severe lower extremity muscle weakness. Furthermore, patients with severe lower extremity muscle weakness may have difficulty getting on and off the treadmill, and those with severe gait limitations may not be able to use it due to the bag barrier hindering the therapist’s ability to facilitate gait. Moreover, some patients may experience discomfort from putting on the required shorts and feel bladder fullness or urgency when unweighted to 50% of their body weight [39].
LBPP gait training has potential applications for enhancing the gait of patients with neurological disorders. However, there is currently no research directly compares different types of body weight-supported devices. In addition, there are insufficient data on the optimal LBPP protocol. Therefore, larger, well-controlled studies are needed to determine the optimal timing and protocol design for maximum efficacy and long-term outcomes of using the LBPP treadmill in neurological patients.
Availability of data and materials
N/A
References
Snijders AH, Van De Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. The Lancet Neurol. 2007;6(1):63–74.
Bohannon RW, Andrews AW, Smith MB. Rehabilitation goals of patients with hemiplegia. Int J Rehabil Res. 1988;11(2):181–4.
Mehrholz J, Thomas S, Kugler J, Pohl M, Elsner B. Electromechanical‐assisted training for walking after stroke. Cochrane Database Syst Rev. 2020(10).
Barbeau H. Locomotor training in neurorehabilitation: emerging rehabilitation concepts. Neurorehabil Neural Repair. 2003;17(1):3–11.
Macko RF, Smith GV, Dobrovolny CL, Sorkin JD, Goldberg AP, Silver KH. Treadmill training improves fitness reserve in chronic stroke patients. Arch Phys Med Rehabil. 2001;82(7):879–84.
Shackleton C, Evans R, Shamley D, West S, Albertus Y. Effectiveness of over-ground robotic locomotor training in improving walking performance, cardiovascular demands, secondary complications and user-satisfaction in individuals with spinal cord injuries: a systematic review. J Rehabil Med. 2019;51(10):723–33.
Kressler J, Thomas CK, Field-Fote EC, Sanchez J, Widerström-Noga E, Cilien DC, et al. Understanding therapeutic benefits of overground bionic ambulation: exploratory case series in persons with chronic, complete spinal cord injury. Arch Phys Med Rehabil. 2014;95(10):1878-1887. e4.
Park JH, Chung YJ. Comparison of aquatic treadmill and anti-gravity treadmill gait training to improve balance and gait abilities in stroke patients. J Korean Phys Ther. 2018;30(2):67–72.
Almutairi S, Swank C, Wang-Price S, Gao F, Medley A. Walking with and without a robotic exoskeleton in people with incomplete spinal cord injury compared to a typical gait pattern. NeuroRehabilit. 2021;49(4):585–96.
Swank C, Almutairi S, Wang-Price S, Gao F. Immediate kinematic and muscle activity changes after a single robotic exoskeleton walking session post-stroke. Top Stroke Rehabil. 2020:1-13.
Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D, et al. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurol. 2006;66(4):484–93.
Almutairi S. The effectiveness of lower-body positive pressure treadmill gait training on mobility function and quality of life in individuals with chronic stroke: prospective cohort study. Middle East J Rehabil Health Stud. 2023;10(2).
Harkema S, Behrman A, Barbeau H. Locomotor training: principles and practice. : Oxf Univ. Press; 2010.
Colombo G, Joerg M, Schreier R, Dietz V. Treadmill training of paraplegic patients using a robotic orthosis. J Rehabil Res Dev. 2000;37(6):693–700.
Ruckstuhl H, Kho J, Weed M, Wilkinson MW, Hargens AR. Comparing two devices of suspended treadmill walking by varying body unloading and Froude number. Gait Posture. 2009;30(4):446–51.
Mehrholz J, Thomas S, Kugler J, Pohl M, Elsner B. Electromechanical‐assisted training for walking after stroke. Cochrane Database Sys Rev. 2020(10).
Mehrholz J, Thomas S, Elsner B. Treadmill training and body weight support for walking after stroke. Cochrane Database Sys Rev. 2017(8).
Bugbee WD, Pulido PA, Goldberg T, D’Lima DD. Use of an anti-gravity treadmill for early postoperative rehabilitation after total knee replacement: a pilot study to determine safety and feasibility. Am J Orthop (Belle Mead NJ). 2016;45(4):167.
Webber SC, Horvey KJ, Yurach Pikaluk MT, Butcher SJ. Cardiovascular responses in older adults with total knee arthroplasty at rest and with exercise on a positive pressure treadmill. Eur J Appl Physiol. 2014;114(3):653–62.
Calabrò RS, Billeri L, Andronaco VA, Accorinti M, Milardi D, Cannavò A, et al. Walking on the moon: s randomized clinical trial on the role of lower body positive pressure treadmill training in post-stroke gait impairment. J Adv Res. 2020;21:15–24.
Liebenberg J, Scharf J, Forrest D, Dufek JS, Masumoto K, Mercer JA. Determination of muscle activity during running at reduced body weight. J Sports Sci. 2011;29(2):207–14.
Earth O. ‘Anti-Gravity’Treadmills Speed Rehabilitation.
Hargens AR, Whalen RT, Watenpaugh DE, Schwandt DF, Krock LP. Lower body negative pressure to provide load bearing in space. Aviat Space Environ Med. 1991;62(10):934–7.
Cutuk A, Groppo ER, Quigley EJ, White KW, Pedowitz RA, Hargens AR. Ambulation in simulated fractional gravity using lower body positive pressure: cardiovascular safety and gait analyses. J Appl Physiol. 2006;101(3):771–7.
Gojanovic B, Cutti P, Shultz R, Matheson GO. Maximal physiological parameters during partial body-weight support treadmill testing. Med Sci Sports Exerc. 2012;44(10):1935–41.
The effects of lower body positive pressure treadmill training on dynamic balance of children with cerebral palsy. 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC): IEEE; 2018.
Kurz MJ, Corr B, Stuberg W, Volkman KG, Smith N. Evaluation of lower body positive pressure supported treadmill training for children with cerebral palsy. Pediatr Phys Ther. 2011;23(3):232–9.
Almutairi SM, Alfouzan MM, Almutairi TS, Alkaabi HA, AlMulaifi MT, Almutairi MK, et al. The safety and feasibility of lower body positive pressure treadmill training in individuals with chronic stroke: an exploratory study. Brain Sci. 2023;13(2):166.
Takacs J, Anderson JE, Leiter JR, MacDonald PB, Peeler JD. Lower body positive pressure: an emerging technology in the battle against knee osteoarthritis? Clin Interv Aging. 2013;8:983–91.
Eastlack RK, Hargens AR, Groppo ER, Steinbach GC, White KK, Pedowitz RA. Lower body positive-pressure exercise after knee surgery. Clin Orthop Relat Res. 2005;431:213–9.
Almutairi SM. The effectiveness of lower-body positive pressure treadmill gait training on mobility function and quality of life in individuals with chronic stroke: prospective cohort study. Middle East J Rehabil Health Stud. 2023;10(2).
Lathan C, Myler A, Bagwell J, Powers CM, Fisher BE. Pressure-controlled treadmill training in chronic stroke: a case study with AlterG. J Neurol Phys Ther. 2015;39(2):127–33.
Sukonthamarn K, Rerkmoung S, Konjen N, Charoenlimprasert J, Sriaoum S. Effectiveness of anti-gravity treadmill training in improving walking capacity and balance in hemiparetic stroke patients: a randomized controlled trial. J Med Assoc Thai. 2019;102(9):982–90.
Oh K, Im N, Lee Y, Lim N, Cho T, Ryu S, et al. Effect of antigravity treadmill gait training on gait function and fall risk in stroke patients. Ann Rehabil Med. 2022;46(3):114–21.
Tang H, Yang B, Lin Q, Liang J, Mou Z. Dynamic biomechanical effect of lower body positive pressure treadmill training for hemiplegic gait rehabilitation after stroke: a case report. World J Clin Cases. 2021;9(3):632–8.
Duran ÜD, Duran M, Tekin E, Demir Y, Aydemir K, Aras B, et al. Comparison of the effectiveness of anti-gravity treadmill exercises and underwater walking exercises on cardiorespiratory fitness, functional capacity and balance in stroke patients. Acta Neurol Belg. 2022:1-10.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9.
Malling ASB, Jensen BR. Motor intensive anti-gravity training improves performance in dynamic balance related tasks in persons with Parkinson’s disease. Gait Posture. 2016;43:141–7.
Byl N, Kretschmer J, Chung A, Thomas A, Fedulow I. Short term technology-assisted-aerobic exercise (AlterGR, GlideTrakTM, Vasper) in a community fitness center for patients with mild to moderate Parkinson’s disease: subjective perceptions and motor effects. J Community Med Public Health Care. 2015;2(009).
Rigby BR, Davis RW, Avalos MA, Levine NA, Becker KA, Nichols DL. Acute cardiometabolic responses to three modes of treadmill exercise in older adults with Parkinson’s disease. Adapt Phys Activ Q. 2018;35(4):424–36.
Rigby BR, Davis RW, Avalos MA, Goudy LS, Becker KA, Nichols DL. An analysis of functional outcome measures after treadmill training in older adults with Parkinson’s disease. Palaestra. 2019;33(1).
Baizabal-Carvallo JF, Alonso-Juarez M, Fekete R. Anti-gravity treadmill training for freezing of gait in Parkinson’s disease. Brain Sci. 2020;10(10):739.
Rose MH, Løkkegaard A, Sonne-Holm S, Jensen BR. Effects of training and weight support on muscle activation in Parkinson’s disease. J Electromyogr Kinesiol. 2013;23(6):1499–504.
Willingham TB, Melbourn J, Moldavskiy M, McCully KK, Backus D. Effects of treadmill training on muscle oxidative capacity and endurance in people with multiple sclerosis with significant walking limitations. Int j MS care. 2019;21(4):166–72.
Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18–29.
Jonsdottir J, Cattaneo D. Reliability and validity of the dynamic gait index in persons with chronic stroke. Arch Phys Med Rehabil. 2007;88(11):1410–5.
Harris JE, Eng JJ, Marigold DS, Tokuno CD, Louis CL. Relationship of balance and mobility to fall incidence in people with chronic stroke. Phys Ther. 2005;85(2):150–8.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–8.
Shu H, Yang T, Yu S, Huang H, Jiang L, Gu J, et al. Aerobic exercise for Parkinson’s disease: a systematic review and meta-analysis of randomized controlled trials. PloS one. 2014;9(7): e100503.
Jacobs PL. NSCA's essentials of training special populations. Hum Kinet. 2017.
Atan T, Taşkiran ÖÖ, Tokçaer AB, Karataş GK, Çalişkan AK, Karaoğlan B. Effects of different percentages of body weight-supported treadmill training in Parkinson’s disease: a double-blind randomized controlled trial. Turk J Med Sci. 2019;49(4):999–1007.
Cherni Y, Gagné-Pelletier L, Bouyer L, Mercier C. Lower-body positive pressure treadmill training for pediatric gait disorders: a sco** review. Appl Sci. 2021;12(1):323.
Acknowledgments
N/A
Institutional review board statement
N/A
Funding
Not funded
Author information
Authors and Affiliations
Contributions
SA designed, search, extract, analyzed, interpreted the results, and writing and editing the manuscript. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
N/A
Consent for publication
N/A
Competing interest
The author declares no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Almutairi, S.M. Lower body positive pressure treadmill gait training for neurological patients: a systematic review. Bull Fac Phys Ther 28, 23 (2023). https://doi.org/10.1186/s43161-023-00134-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43161-023-00134-x