Abstract
Background/purpose
Surgical management of high-type anorectal malformations (ARM) has evolved over the years with the widespread of the laparoscopic approach over the last two decades. This study aims to compare the outcome of patients with high anorectal malformation (ARM) managed with laparoscopic-assisted anorectal pull-through (LAARP) vs. the open posterior sagittal anorectoplasty (PSARP) at a single Institution.
Methods
A retrospective chart review of pediatric patients, who were managed for high-type ARM at our institution, was performed for the period 2000–2015. Nine were excluded because of a lack of important data. Demographic data, surgical approach, associated anomalies, and complications were collected. Functional outcome was measured using the modified clinical scoring for the defecation function of the Japanese study group of anorectal anomalies. Comparison between groups was done using the T test for continuous variables and the Fisher-exact test for proportions. P < 0.05 is considered statistically significant.
Results
There were 82 patients with high type imperforate anus (59 males and 23 females) 73% had laparoscopy vs. 27% open. Type of fistulae were rectourethral (36), rectovesical (12), no fistula (19), and (15) cloaca anomalies. Patients underwent surgery at a mean age 8.4 (laparoscopy) vs. 10.1 (open) months (P value = 0.14). There was no difference between the two groups regarding weight at the surgery or associated anomalies, except for VACTRAL and genitourinary malformations which were more among the laparoscopic group (8 vs. 1).
There was no statistical significance for all elements of defecation function score: sensation, constipation, and soiling (P values 0.17, 0.6, 0.07, respectively). There was no difference between the two groups regarding rectal prolapse (P = 0.06), whereas rectal stenosis is more in PSARP compared to LAARP (P = 0.03). The hospital stay was significantly shorter in LAARP 7.1 vs. 9.4 (P = 0.006).
Conclusions
The defecation function and complication rate for both laparoscopic and open groups were almost similar. This may justify the preference of the laparoscopic approach over the open one, given its minimally invasive nature.
Similar content being viewed by others
Background
Anorectal malformations include a wide spectrum of varieties ranging from the simple imperforated membranous anus to a more complex anorectal fistula. High-grade anorectal malformations, which include common channel cloaca, vesical, or urethral fistulae, require complex surgical procedures.
Surgical management has evolved over the years. Pena et al. reported their experience (1982) with the posterior sagittal anorectal approach (PSARP) using a sacral incision for adequate visualization of the anatomy [1]. The literature review showed that the chance of being totally continent ranging between 0 and 32% after PSARP, while significant fecal soiling was reported in 30–56% of patients [2]. As the minimally invasive technique developed over the last two decades, Georgeson et al. described his experience with laparoscopic-assisted anorectal pull-through (LAARP) for high imperforate anus in 2000. His technique includes minimal perineal dissection, preservation of the distal rectum, and accurate placement of the rectum within the levator ani and external anal sphincter muscle complex [3]. Since then (LAARP) has gained popularity and was expected to achieve better fecal continence than the conventional procedure due to its minimal nature. However, few studies compared the two approaches, and the outcome is variable with no definite conclusions. The aim of the study is to adopt the Modified Clinical scoring for defecation function (Japanese study group of anorectal anomalies) classification to analyze and compare the outcomes of patients with high anorectal malformation (ARM) managed with laparoscopic-assisted anorectal pull through (LAARP) vs. posterior sagittal anorectoplasty (PSARP) at a single institution.
Methods
The study was designed as a retrospective chart review of pediatric patients managed for high type ARM at King Faisal Specialist Hospital and Research Centre (KFSH & RC) for the period 2000–2015. Demographic data, surgical approach, operative time, hospital stay, associated anomalies, and complications were collected.
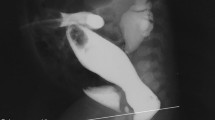
PSARP and LAARP were performed after a left-sided colostomy was created early on. All Patients (males and females) had renal US, Echocardiography, and contrast loopogram via the mucous fistula to check for associated anomalies and delineate the ARM. For all cloacal cases, common channel endoscopy was essential.
Since 2004, we started utilizing the laparoscopic approach instead of the PSARP and have no specific criteria for selecting the approach; moreover, the rectourethral fistulae cases, whether prostatic or bulbar, did not affect the approach and have been done laparoscopically since then in contrary to PSARA in old ones.
Postoperatively, a foley catheter was kept for 7 days while patients were in the hospital. The last three patients in the LAARP group were sent with a foley catheter in situ to be removed at a local hospital, which shortened the length of the hospital stay.
The functional outcomes were measured using the modified clinical score for the defecation function of the Japanese study group of anorectal anomalies [4].
The clinical scoring for defecation function criteria is based on a simple grading classification with strictly defined outcome variables: sensation, constipation, soiling, and staining.
For the purpose of this study, we modified this clinical scoring by removing the staining score due to difficulty in getting the information from patients/parents and minimizing the subdivided score for each parameter to become 0 or 1 (Table 1) for easier interpretation. The questionnaire data was collected by phone interviews by two individuals. The interrater reliability test was done for the 1st 10 patients, and a high correlation was obtained (86%).
The comparison between the two groups was done using a T test for continuous variables and Chi-square or Fisher’s exact test for proportions. A P value > 0.05 was considered statistically significant. The study was approved by our hospital’s IRB committee (RAC # 2151 041).
Results
There were 91 patients with high type ARM; 9 were excluded because of a lack of important data. The remaining 82 patients were divided into two groups 60 patients (45 male and 15 female) had LAARP versus 22 patients (14 male and 8 female) had PSARP. The LAARP female cases consisted of 9 cloacal and 6 no fistula cases, whereas the PSARP had 6 cloacal and 2 no fistula cases. All patients had left-sided colostomy performed shortly after birth, followed by anorectal repair, and completed by colostomy closure after 6 to 10 weeks after definitive repair. The characteristics of the two groups are illustrated in Table 2.
The hospital stay was significantly shorter in the laparoscopic technique 7.1 vs. 9.4 days (P value 0.006).
Fistula types for two groups are shown in Table 3.
In terms of associated anomalies, Table 4 demonstrated the distribution between the two groups.
Follow-up was significantly longer in PSARP 106.5 m V. S 69.2 m with P value 0.001; one patient treated laparoscopically passed away for cardiac comorbidity. One case converted from laparoscopy to open because of severe adhesions encountered during surgery.
Regarding postoperative complications, two cases of PSARP underwent redo surgery because of the malpositioning of the new anus. One patient had a bowel obstruction and exploration post-laparoscopic repair. Two patients in the LAARP had urethral stricture managed by dilatation and two urethral diverticula with no significant problems. Two patients had wound infections in each group. There was no difference between the two groups regarding rectal prolapse (p value 0.06), whereas the rectal stenosis is more in PSARP compared to LAARP (27.7% versus 7.8%) P value 0.03.
53 out of 82 (65%) scoring sheets were filled (39 LAARP versus 14 PSARP). Quality of life data showed no significant differences between the two groups with the P values 0.17, 0.6, 0.07 for sensation, constipation, and soiling, respectively (Table 5).
Discussion
PSARP was the standard of care since 1982 for the management of anorectal malformations, especially the high types. Georgeson reported the laparoscopic approach (LAARP) with promising results in the year 2000 [3]. The latter approach has spread globally with a relative lack of outcome data. Comparing the outcome results of the two approaches may add more evidence to support its utilization.
Although we could not demonstrate any significant differences between the use of LAARP or PSARP, regarding the three categories of the Modified Clinical scoring for defecation function, the overall trend would appear that more patients who underwent LAARP had a better functional outcome. Moreover, the fact that both were comparable may support the minimal approach (LAARP) associated with less stress on patients, better cosmesis, faster recovery, and shorter hospital stay.
In the literature, different scoring systems (subjective and objective) were used to assess continent, rectal tone, soiling, and bowel motion [5,6,7,8,9,10]. We have modified the clinical score for the defecation function of the Japanese study group of anorectal anomalies to show clear outcome data and simplify reporting by patients and families.
A systemic review by Al-Hozaim et al. in 2009 showed that only four studies compared the outcome between LAARP and PSARP [11]. The total numbers of patients were 47; they compared the following: stool frequency, continence, the anatomic position of pull through, and sphincter function. All of them concluded that LAARP seems to be superior for patients with high type anorectal malformation, with a long-term follow-up is needed to assess fecal continence [5,6,7,8]. Also, a similar conclusion was found in a systematic review by Shawyer AC [12] and a meta-analysis by Han Y [13].
Wong and colleagues used magnetic resonance (MRI) to assess the anatomical features after LAARP and compared functional outcomes with historical controls who had PSARP. MRI of the pelvis was performed postoperatively, and a semi-quantitative score was used to assess the degree of sphincter symmetry, peri-rectal fibrosis, and the position of the pull-through rectum. The defecation status of these patients was also recorded. The study concluded that LAARP allows for more optimal anatomical reconstruction in patients with high/intermediate types of the imperforated anus [7].
An-**ao Ming et al. reviewed 32 patients who underwent LAARP and compared them with 34 patients who underwent PSARP using Krickenbeck classification and reported that the long-term functional outcomes after LAARP were equivalent if not better than those of PSARP [14].
Ichijo et al. compared both types of surgery objectively using anal endosonography and pelvic magnetic resonance imaging to assess the pelvic muscle thickening, and he concluded that there is no statistically significant difference. Subjectively, he used “Continence evaluation questionnaire score” which includes frequency of defecation, soiling, perianal erosion, anal shape and medication, and he concluded that the score was generally higher after laparoscopic surgery throughout the study, but it was only statistically significant at 3 and 4 years of age [5].
Using the Kelly scoring system, one study showed equivalent results [8], while others have shown the superiority of LAARP over PSARP [15, 16].
In terms of long-term complications, the incidence of anal stenosis was higher in the posterior sagittal approach, as shown by our data and others [14]. This may be explained by the effect of open dissection. On the other hand, rectal prolapse was more in laparoscopy technique, although it did not reach significance. This has been reported previously [14, 17]. Other studies did not find such this effect [18]. We believe that the extensive reconstruction in the PSARP approach induces more fibrosis, hence fixing the anorectum to the pelvis structures and preventing rectal prolapse.
In ARM with rectourethral fistulae, there is no accurate guidance (landmark) to where to stop dissection of the fistula, fearing injury to the urethra. Getting close to the urethra could result in urethral stricture, and dividing away from it may result in a urethral diverticulum. We have encountered early in the series two stenoses (managed with dilatation successfully) and two urethral diverticula with no significant problems. All were in the LAARP.
Koga and his colleagues invented the intraoperative measurement of the rectourethral fistula using a cystoscope with a calibrated catheter to overcome the dilemma [19].
The differences in operative time between the two approaches vary among the studies in the literature; some of them reported shorter operative time in the laparoscopic pull through [7, 9], whereas Koga H reported the opposite [20].
The postoperative hospital stay in the LAARP group was significantly shorter, which is supported by many studies as well [7, 9, 15].
In conclusion, the defecation function and complication rate for both laparoscopic and open groups were almost similar from the statistical point of view. There was some trending in favor of the laparoscopic approach regarding shorter operative time, shorter hospital stay and less stenoses; the latter and the minimal nature of the laparoscopic approach may justify its utilization over the open one. Long-term follow-up with larger sample size studies may be needed to elicit the differences between the two approaches.
Availability of data and materials
The data and material are available for review.
Abbreviations
- ARM:
-
Anorectal malformation
- LAARP:
-
Laparoscopic-assisted anorectal pull-through
- PSARP:
-
Posterior sagittal anorectoplasty
- MRI:
-
Magnetic resonance imaging
References
Peña A, Devries PA. Posterior sagittal anorectoplasty: important technical considerations and new applications. J Pediatr Surg. 1982;17(6):796–811. https://doi.org/10.1016/s0022-3468(82)80448-x.
Levitt MA, Peña A. Outcomes from the correction of anorectal malformations. Curr Opin Pediatr. 2005;17:394–401.
Georgeson KE, Inge TH, Albanese CT. Laparoscopically assisted anorectal pull-through for high imperforate anus--a new technique. J Pediatr Surg. 2000;35(6):927–31. https://doi.org/10.1053/jpsu.2000.6925.
Endo M, Hayashi A, Ishihara M, et al. Analysis of 1,992 patients with anorectal malformations in Japan over the past two decades. Steering Committee of Japanese Study Group of anorectal anomalies. J Pediatr Surg. 1999;34(3):435–41. https://doi.org/10.1016/s0022-3468(99)90494-3 PMID: 10211649.
Ichijo C, Kaneyama K, Hayashi Y, et al. Midterm postoperative clinicoradiologic analysis of surgery for high/intermediate-type imperforate anus: a prospective comparative study between laparoscopy-assisted and posterior sagittal anorectoplasty. J Pediatr Surg. 2008;43(1):158–63. https://doi.org/10.1016/j.jpedsurg.2007.09.037.
Lin CL, Wong KKY, Lan CCL, et al. Earlier appearance and higher incidence of the rectoanal relaxation reflex in patients with imperforate anus repaired with laparoscopically assisted anorectoplasty. Surgery Endosec. 2003;17:1646–9.
Wong KKY, Khong PL, Lin SCL, et al. Postoperative magnetic resonance evaluation of children after laparoscopic anorectoplasty for imperforate anus. Int J Color Dis. 2004;20:33–7.
Kudou S, Iwanaka T, Kawashima H, et al. Midterm follow-up study of high-type imperforate anus after laparoscopically assisted anorectoplasty. J Pediatric surgery. 2005;40:1923–6.
Bailez MM, Cuenca ES, Mauri V, Solana J, Di Benedetto V. Outcome of males with high anorectal malformations treated with laparoscopic-assisted anorectal pull-through: preliminary results of a comparative study with the open approach in a single institution. J Pediatr Surg. 2011;46(3):473–7. https://doi.org/10.1016/j.jpedsurg.2010.08.007.
Kelly JH. The clinical and radiological assessment of anal continence in childhood. Aust N Z J Surg. 1972;42(1):62–3. https://doi.org/10.1111/j.1445-2197.1972.tb06743.x.
Al-Hozaim O, Al-Maary J, AlQahtani A, Zamakhshary M. Laparoscopic-assisted anorectal pull-through for anorectal malformations: a systematic review and the need for standardization of outcome reporting. J Pediatr Surg. 2010;45(7):1500–4. https://doi.org/10.1016/j.jpedsurg.2009.12.001.
Shawyer AC, Livingston MH, Cook DJ, et al. Laparoscopic versus open repair of the recto-bladder neck and recto-prostatic anorectal malformations: a systematic review and meta-analysis. Pediatr Surg Int. 2015;31(1):17–30. https://doi.org/10.1007/s00383-014-3626-3.
Han Y, **a Z, Guo S, et al. Laparoscopically assisted anorectal pull-through versus posterior sagittal anorectoplasty for high and intermediate anorectal malformations: a systematic review and meta-analysis. Plos One. 2017;12(1):e0170421. Published 2017 Jan 18. https://doi.org/10.1371/journal.pone.0170421.
An-**ao Ming A, Long Li A, Mei Diao A, et al. Long-term outcomes of laparoscopic-assisted anorectoplasty: a comparison study with posterior sagittal anorectoplasty. J Pediatr Surg. 2014;49:560–3.
Tong QS, Tang ST, Pu JR, et al. Laparoscopically assisted anorectal pull-through for high imperforate anus in infants: intermediate results. J Pediatr Surg. 2011;46(8):1578–86. https://doi.org/10.1016/j.jpedsurg.2011.04.059.
Yang J, Zhang W, Feng J, et al. Comparison of clinical outcomes and anorectal manometry in patients with congenital anorectal malformations treated with posterior sagittal anorectoplasty and laparoscopically assisted anorectal pull through. J Pediatr Surg. 2009;44(12):2380–3. https://doi.org/10.1016/j.jpedsurg.2009.07.064.
Jung S-M, Lee S-K, Seo J-M. Experience with laparoscopic-assisted anorectal pull-through in 25 males with anorectal malformation and rectourethral or rectovesical fistulae: postoperative complications and functional results. J Pediatr Surg. 2013;48:591–6.
Kimura O, Iwai N, Sasaki Y, et al. Laparoscopic versus open abdominoperineal rectoplasty for infants with high-type anorectal malformation. J Pediatr Surg. 2010;45:2390–3.
Koga H, Kato Y, Shimotakahara A, et al. Intraoperative measurement of rectourethral fistula: prevention of incomplete excision in male patients with high−/intermediate-type imperforate anus. J Pediatr Surg. 2010;45(2):397–400. https://doi.org/10.1016/j.jpedsurg.2009.10.085.
Koga H, Ochi T, Okawada M, et al. Comparison of outcomes between laparoscopy-assisted and posterior sagittal anorectoplasties for male imperforate anus with recto-bulbar fistula. J Pediatr Surg. 2014;49(12):1815–7. https://doi.org/10.1016/j.jpedsurg.2014.09.028.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MAS designed the study and participated in collecting, analyzing, and interpreting the data and manuscript writing. AW designed the study and aided in the collection of the data. SS designed the study and participated in the analysis and interpretation of the data and editing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by our hospital’s IRB committee (RAC # 2151 041).
A verbal consent was obtained from all parents or guardians who participated in the phone questionnaire.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
AlShawa, M.A., Al Wusaibie, A. & Al Shanafey, S. Laparoscopic-assisted anorectal pull-through vs. posterior sagittal anorectoplasty for treating high anorectal malformations: a single-center experience. Ann Pediatr Surg 18, 27 (2022). https://doi.org/10.1186/s43159-022-00162-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-022-00162-7