Abstract
Background
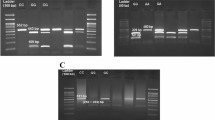
The genetic make-up of local granulosa cells and their function in the pathophysiology of polycystic ovary syndrome (PCOS) is crucial to a full comprehension of the disorder. The major purpose of this study was to compare the Single Nucleotide Polymorphism (SNP) of cumulus granulosa cells (CGCs) and mural granulosa cells (MGCs) between healthy individuals and women with PCOS using genome-wide association analysis (GWA). A case–control study was conducted in a total of 24 women diagnosed with PCOS and 24 healthy non-PCOS women of reproductive age aggregated into 4 samples of 6 patients each. GWA studies entail several processes, such as cell separation, cellular DNA extraction, library preparation followed by interpretation using bioinformatics databases. SNP locations were identified by reference gene also involves the use of Matrix-assisted laser desorption/ionisation-time of flight (MALDI-TOF) mass spectrometry (MS) (MALDI-TOF-MS) for the first sorting. Hybridization with the gene chip was followed by reading the SNP genotypes according to the publications in the literature. TASSEL (Trait Analysis by aSSociation, Evolution and Linkage) program and methods were used for GWA studies.
Results
An aggregate of 21,039 SNP calls were obtained from our samples. Genes of autoimmune illnesses, obesity, inflammatory illnesses, nervous system diseases such as retinitis pigmentosa, autism, neural tube defects, and Alzheimer's disease; and various malignancies such as lung cancer, colorectal cancer, breast cancer were also identified in these cells. Gene ranking score reveals that granulosa cells carry key genes of neurological system and reproductive systems especially in brain and testis, respectively.
Conclusions
Mural and Cumulus Granulosa cells were shown to have the PCOS directly and indirectly related genes MMP9, PRKAA2, COMT and HP. We found that the expression of ARID4B, MUC5AC, NID2, CREBBP, GNB1, KIF2C, COL18A1, and HNRNPC by these cells may contribute to PCOS.
Graphical abstract

Highlights
-
Investigated genetic make-up of mural and cumulus granulosa cells
-
Role of these cells in pathogenesis of PCOS studied
-
Local and systematic effect of these genes were correlated
Similar content being viewed by others
Background
Biomedical science has changed a lot since new technologies have come out. Now, it is where many different areas of science and engineering meet to find solutions to problems that people are facing. Innovative uses of technology in healthcare can improve patient safety, clinical effectiveness, and patient monitoring, as well as help accelerate and lower the cost of develo** and testing medical therapies. Some of the new and innovative technologies that are changing the healthcare system are the carbodiimide and N-hydroxy succinimide cross-linking system [1,2,3] thin film hydration techniques [4], visible light photocatalysts [5], sonochemical approach [6], hydrothermal methods [7] photocatalytic compounds with band gap [8], high-performance photocatalytic process [9] and facile combustion routes [10].
Single-nucleotide polymorphisms (SNPs) are the alteration in the single base-pair sequence of the deoxyribonucleic acid (DNA) when it takes place at a high frequency of the human genome also termed as modern units of genetic variation [11]. These genetic variations are identified by cutting-edge research technique Genome-Wide Association Studies (GWASs) through comprehensive sequencing and analysis of the complete genome of thousands of SNPs at once, allowing for the identification of common SNPs that are linked to certain diseases [12]. Focusing on SNPs throughout the entire genome is an exciting new direction in the study of complex, common illnesses in which several genes contribute in identifying the genes to a person's risk, pharmacological reactions, susceptibility to contaminants and environmental factors; in prognosis and diagnosis of illness or trait [13].
Women of reproductive age (12–45 years) are disproportionately affected by polycystic ovary syndrome (PCOS), which has a varying prevalence rate across different ethnic groups (ranging from 2.2% to 26% worldwide) responsible for almost 40% of female infertility in India [14]. The clinical presentation of PCOS is more genetically variable and can have an impact on a wide range of organs including the ovary, pituitary, hypothalamus, pancreas, liver, adrenal glands, etc. Negative body image, compromised physical and mental health, and a lower quality of life are all serious concerns for women who suffer from PCOS [15]. At least 70 candidate genes have been identified as potentially contributing to the diseases of the syndrome, although the exact aetiology is still unclear [16]. PCOS symptoms include absent or irregular periods, anovulation, male-pattern hair growth, acne, acanthosis nigricans, obesity with central or distinct abdominal obesity, etc. Impaired glucose tolerance (IGT), atherogenic dyslipidaemia (AD), type 2 diabetes mellitus, hepatic steatosis, cardiovascular problems such as hypertension, and metabolic complications, as well as endometrial cancer, are all more common in these individuals [17].
During ovulation, the oocyte is accompanied by the cumulus granulosa cells (CGCs), immediately surrounding the oocyte, supporting the oocyte by sharing nutrients and a safe, caring environment. These cells emit hyaluronic acid, stabilises the produced proteins; and collectively hel** the oocyte to resume meiotic division, initiating the maturation process and facilitating the formation of adult cumulus-oocyte-complexes [17]. The mural granulosa cells (MGCs) line the antrum of develo** follicles surrounding the fluid-filled section of the follicle and in close proximity to the basal lamina [18]. The MGCs differentiate into luteal cells and remain in the ovary after ovulation called corpus luteum, whereas CGCs transport the egg to the oviduct. Many reports and studies have shown that the quality of oocyte production and follicular maturation are both affected by the state of these cells [19]. There are several genes present within the follicles that are differently expressed between these two divisions of granulosa cells: MGCs and CGCs [20].
Since then, CGCs and MGCs have been important in a wide range of cellular processes, such as signal transduction, making extracellular matrix, folliculogenesis, ovulation, and fertilisation. For the improvement of knowledge, many methods are used. One of these is the modern GWAS [18]. Therefore, the primary goal of this study was to look into the genome-wide association of the SNP in order to find out more about SNPs that are linked to PCOS. If these SNPs are found and proven, they could help us know and understand more about the molecular mechanism and genetic diversity of PCOS. The secondary goal of this research was to find out how different cumulus cells and mural cells are genetically and what role they play in the development of PCOS. This was carried out by looking at SNPs and gene expressions in granulosa cells with SNP arrays.
Methods
Study Participants and centre
Twenty-four women with PCOS and twenty-four control women of the same ethnicity, age range (25–37 years), and body mass index (BMI) were enrolled in the trial, which took place between January 2020 and September 2021 at Morpheus Prasad International IVF Centre and Indira IVF Fertility Centre in Dehradun. Subjects were categorised based on clinical manifestations and diagnostics, without regard to genotype. The cells' DNA was taken and combined into a pool (n = 6), and then millions of SNPs were found. This GWA study was conducted at the TERI School of Advanced Studies, New Delhi, India.
Criterion of inclusion
The age range of the women in the research was from 25 to 37 years old. According to the Rotterdam Criteria agreement, PCOS is diagnosed when two out of three of the following conditions are present: hyperandrogenism; oligoanovulation; and polycystic ovaries on ultrasound examination (less than 12 follicles measuring 2–9 mm in diameter and/or an ovarian volume & increased ovarian volume, i.e., > 10 cm3 in a single ovary). Women without any gynaecological problems serving as a control group are those who choose to undergo the in vitro fertilisation/Intracytoplasmic sperm injection (IVF/ICSI) process for infertility caused by male factors (husband or male partner). Women in the control group had normal ovarian morphology as determined by ultrasonography and had androgen levels within the reference range (0.4–3.5 nmol/L) throughout the follicular phase of their menstrual cycles.
Criterion of exclusion
A diagnosis of androgen-producing tumours, a lack of the enzyme 21-hydroxylase, non-classical adrenal hyperplasia, hyperprolactinemia, active thyroid disease, or Cushing syndrome would rule out participation. Medications likely to affect carbohydrate metabolism or endocrine parameters (oral contraceptives, anti-hypertensives, lipid-lowering, and anti-inflammatory drugs) for at least three months prior to entering the study were also exclusion criteria for both women with PCOS and control women. BMIs below 18 kg/m2 or above 45 kg/m2 were also excluded. Participants who did not sign an informed consent form were also excluded from the research.
Bioethics
All participants provided written informed consent, and the study was approved by the University Research and Ethics Committee (UREC) (DITU/UREC/2019/07/2) on July, 9th 2019. All data collected were anonymous and identity of individuals will remain confidential.
Separation of CGCs from follicular fluid
As part of IVF/ICSI, routine short or long-term gonadotropin-releasing hormone agonist injection protocols were used to stimulate the ovaries in a controlled way. After about 36 h, the follicular fluid was taken and the oocytes were taken while the patient was under a light anaesthetic. Each person's follicular fluid was taken from 3–5 follicles and put into a 15 ml polypropylene centrifuge tube with a conical bottom. The fluid was then put into Petri dishes so it could be looked at under a microscope to find cumulus oocyte complexes. After the multiple washes, both the CGCs and the pipette tips dropped off the dish. The CGCs were then mixed together and washed with 1X Phosphate Buffer Saline. Six patients' CGCs were pooled together for further study [21].
Isolation of MGCs
The rest of the follicular fluid from the previous step was put back into the tubes of the centrifuge, which contained the granulosa cells. The tubes were then spun at 800 × g for 10 min at room temperature. The supernatant was discarded, and the remaining cells at the bottom of the centrifuged tube were re-suspended with a small amount of phosphate buffer saline. This suspension was then carefully layered (to avoid mixing at this stage) over the same amount of 50% (v/v) PercollTM and centrifuged at 500 × g for 20 min at room temperature [76]. To identify the similarities and differences between variants we used both hg19 and hg38 because hg19 is a unified representation of several genomes and hg38 is a representation of alternative sequences in line with previous study [77]. The genes expressed in the nervous system (2.13 and 4.09 in hg-19 and hg-38, respectively) and the reproductive system have the highest matching scores (2.44 and 3.98 in hg-19 and hg-38, respectively). This shows that granulosa cells have the genes needed for these systems substantiate the fact that they contribute in pathogenesis of PCOS through hyperandrogenism, obesity and insulin resistance [78].
Insulin resistance is known to be linked to PCOS through Protein Kinase AMP-Activated Catalytic Subunit Alpha 2 (PRKAA2), which is also found in granulosa cells. Our study also found Matrix Metallopeptidase 9 (MMP9) is linked to a higher risk of cardiovascular disease, which is also a serious problem that can happen with PCOS in line with earlier study [79]. Since haptoglobin (HP) is responsible for anti-oxidant and anti-inflammatory properties, its levels may be lower in people with PCOS supporting the fact that it has significant pro-inflammatory role in diabetes and metabolic syndrome [80]. Through GWA studies of SNPs, the results of this study showed the presence of PRKAA2, MMP9, and HP. This shows that granulosa cells are expressing these genes, which may lead to PCOS and complications.
The results of this study show that the granulosa cells have genes that make HP, which binds to haemoglobin (Hb) and causes haemolysis when macrophages recognise this. It shows that the HP gene in granulosa cells is linked to PCOS problems due to insulin resistance mentioned in previous study [81]. The most found genes Ceramide Kinase (CERK), MMP9, Protein Phosphatase 1 Regulatory Subunit 16B (PPP1R16B), Phospholipase C Beta 1 (PLCB1), Pantothenate Kinase 2 (PANK2), Piezo Type Mechanosensitive Ion Channel Component 2(PIEZO2), THO Complex Subunit 1 (THOC1), Component of Oligomeric Golgi Complex 4 (COG4), RNA Polymerase II Subunit C (POLR2C), Nuclear Pore Complex Interacting Protein Family Member B3 (NPIPB3), PPFIA Binding Protein 2 (PPFIBP2), Neuron Navigator 2 (NAV2), Nuclear Protein, Coactivator of Histone Transcription (NPAT), Glutamate Ionotropic Receptor Kainate Type Subunit 4 (GRIK4), Heterogeneous Nuclear Ribonucleoprotein C (HNRNPC), Rab Geranylgeranyltransferase Subunit Alpha (RABGGTA), F-Box And Leucine Rich Repeat Protein 16 (FBXL16), Meteorin, Glial Cell Differentiation Regulator (METRN), Coiled-Coil Domain Containing 78 (CCDC78), Tryptase Alpha/Beta 1 (TPSAB1), Deoxyribonuclease 1 (DNASE1), etc.) are mostly expressed in the brain, ovary, and testis. These supports the fact that there is a variation in expression of individual genes in organs [82]. Genes shared by epithelial cells, hearts, ovaries, and kidneys ArfGAP With Coiled-Coil, Ankyrin Repeat and PH Domains 3 (ACAP3), G Protein Subunit Beta 1 (GNB1), Retention In Endoplasmic Reticulum Sorting Receptor 1 (RER1), Multiple EGF Like Domains 6 (MEGF6), Rho Guanine Nucleotide Exchange Factor 10 Like (ARHGEF10L), Platelet Activating Factor Acetylhydrolase 2 (PAFAH2), Small Nuclear Ribonucleoprotein U5 Subunit 40 (SNRNP40), Zinc Finger CCCH-Type Containing 12A (ZC3H12A), Spermatogenesis Associated (6SPATA6), Solute Carrier Family 1 Member 7 (SLC1A7), Ras Association Domain Family Member 7 (RASSF7), Troponin I2, Fast Skeletal Type (TNNI2), PPFIBP2, NAV2, GRIK4, HNRNPC, CERK, Suppressor Of Glucose, Autophagy Associated 1 (SOGA1), and RABGGTA) are involved in neuromuscular development, neurotransmitter reuptake, positive regulation of miRNA catabolic process, immune response-activating signal transduction, vagus nerve development, etc., as mentioned in previous study [83]. It is possible that these genes, which are found in granulosa cells, are involved in the altered physiological activities that occur with PCOS.
We found six genes that are common between hg19 and hg38 by comparing the SNP data from the two genomes. These genes include AT-Rich Interaction Domain 4B(ARID4B), COMT, HP, MMP9, NID2 and Mucin 5AC, Oligomeric Mucus/Gel-Forming(MUC5AC). ARID4B of granulosa cells, which is expressed in the testis, bone marrow, bladder, and adrenal glands, among other places, and is responsible for the overexpression of testosterone from sertoli cells, may be the cause of hyperandrogenism [84].This links to the development of hyperandrogenism commonly seen in PCOS. Placental, adrenal, and ovarian Catechol-O-methyltransferase (COMT) expression is first implicated in symptoms of PCOS such as fibromyalgia, chronic fatigue, and mild inflammation. As per the literature and results of present study these genes were also found in granulosa cells, which indicates that a significant role may be played by the genes of granulosa cells [85]. The PCOS-related behaviours of diabetic nephropathy, coronary artery disease, and inflammatory illness were all discovered in granulosa cells, indicating that HP may have a role in the aetiology of PCOS similar to the fact produced in earlier study they were found strongly associated with obesity and glucose tolerance [42]. The MMP9 gene has a role in the remodelling of tissue, reproduction, embryonic development, and the local proteolysis of the extracellular matrix, as well as in the differentiation of macrophages and the migration of leukocytes. These study outcomes validate the role of this gene in reduction in scar formation and promote neovascularization [86]. PCOS is a syndrome in which there is a disruption in the normal functions of the immune system, the development of embryos, reproduction, and the remodelling of several different tissues, organs, and systems. This provides some insight into the potential function of these genes in granulosa cells. The expression of Mucin 5AC, Oligomeric Mucus/Gel-Forming (MUC5AC) in the stomach has been connected to biliary tract sickness, itchy-dry eye disease, Sjogren's syndrome, cystic fibrosis, and other disorders implicated with PCOS [87]. In our study MUC5AC expression found in CGCs and MGCs. The fact that NID2, which is linked to cell-adhesion, cardiovascular disease, polycystic ovarian syndrome, gastric cancer, and other diseases and conditions, is expressed in these granulosa cells is an indication that MGCs and CGCs are involved in PCOS pathogenesis through expression of this gene. Earlier study correlated other diseases and conditions, such as nasopharyngeal, esophageal, and oral carcinoma linking to NID2 methylation [88].
The Cyclic adenosine monophosphate (cAMP) response element-binding protein (CREBBP) gene plays a vital role in the interactive signalling process, as shown by the findings of studies on the interactions between proteins. It might be because of its essential function in the cellular phosphorylation signalling system, which influences processes such as cell differentiation, proliferation, growth, and cyclic regulation as mentioned in previous study [89]. If these steps are changed in PCOS, it could be because the expression of genes in granulosa cells has changed. GNB1, which we found, acts as a modulator or transducer in several transmembrane signalling pathways that control cell growth and differentiation, transport activities, protein synthesis, and other processes affected by PCOS. This is in line with the outcome of previous study explaining its importance in clinical etiopathogenesis of mutation [90]. Another gene of Kinesin family member 2C (KIF2C) is involved in chromosomal segregation during mitosis reflected in previous study [91] was also present in granulosa cells which is one of the most common complications in PCOS. In this GWA study, we found that Collagen alpha-1(XVIII) chain (COL18A1), which is involved in extracellular matrix architecture, Phospholipase-C pathway, collagen chain trimerization, ERK signalling, etc., similar to hepatotoxicity induced by drugs presented by previous study [92] affects the signalling process in PCOS, showing the role of this gene in the signal transduction pathway in skeletal muscle, which causes a change in glucose uptake as mentioned in earlier study [93].
Heterogeneous nuclear ribonucleoproteins C1/C2 (HNRNPC) is an oncogenic gene that is found in a wide range of tissues and organs, such as bone marrow, brain, ovary, bladder, testis, thyroid, endometrium, etc. These results are supported by one of the study carried out on hnRNP family [94, 95]. It is involved in protein metabolism, signalling through RhoGTPases, and the Rho Related BTB Domain-GTPase (RHOBTB-GTPase) Cycle. It was also found in MGCs and CGCs. Because of this gene, the cyst might continue to recur even after surgery as reported in earlier study [96, 97].
Conclusion
We have compiled a list of the characteristics of a large number of genes that are present in MGCs and CGCs, as well as their direct and indirect connections to PCOS. Based on the results, we can propose that the MGCs and CGCs express genes PRKAA2, MMP9, HP, ARID4B, COMT, MUC5AC, NID2, CREBBP, GNB1, KIF2C, COL18A1, and HNRNPC mostly connected to the clinical symptoms of PCOS, such as insulin resistance, cardiovascular disease, low-grade inflammation, hyperandrogenism, fibromyalgia, chronic fatigue, and itchy- dry eyes. We do suggest, though, that more detailed studies be done with a larger number of patients from different hospitals, regions, and ethnic groups. This would give us more information from which to reach a conclusion on the role of CGCs and MGCs in pathogenesis of PCOS.
Availability of data and materials
Data and materials are confidential and available with first author.
Abbreviations
- BMI:
-
Body mass index
- CGCs:
-
Cumulus granulosa cells
- COCs:
-
Cumulus oocyte complexes
- COMT:
-
Catechol-O-methyltransferase
- DNA:
-
Deoxyribonucleic acid
- FSH:
-
Follicle-stimulating hormone
- GLM:
-
Generalised linear models
- GO:
-
Gene Ontology
- GWAS:
-
Genome-Wide Association Study
- hCG:
-
Human chorionic gonadotropin
- ICSI:
-
Intracytoplasmic sperm injection
- IVF:
-
In vitro fertilisation
- LH:
-
Luteinizing hormone
- MGCs:
-
Mural granulosa cells
- MLM:
-
Mixed linear models
- OMIM:
-
Online Mendelian Inheritance in Man (OMIM®)
- PCOS:
-
Polycystic ovary syndrome
- SNP:
-
Single nucleotide polymorphism
- VCF:
-
Variant Call Format
References
Qazvini NT, Zinatloo S (2011) Synthesis and characterization of gelatin nanoparticles using CDI/NHS as a non-toxic cross-linking system. J Mater Sci: Mater Med 22(1):63–69. https://doi.org/10.1007/s10856-010-4178-2
Zinatloo-Ajabshir S, Qazvinia NT (2014) Inverse miniemulsion method for synthesis of gelatin nanoparticles in presence of CDI/NHS as a non-toxic cross-linking system. J Nanostruct 4:267–275. https://doi.org/10.7508/jns.2014.03.003
Zinatloo-Ajabshir S, Taheri Qazvini N (2015) Effect of some synthetic parameters on size and polydispersity index of gelatin nanoparticles cross-linked by CDI/NHS system. J Nanostruct 5(2):137–144. https://doi.org/10.7508/jns.2015.02.008
Zinatloo-Ajabshir Z, Zinatloo-Ajabshir S (2019) Preparation and characterization of curcumin niosomal nanoparticles via a simple and eco-friendly route. J Nanostruct 9(4):784–790. https://doi.org/10.22052/JNS.2019.04.020
Zinatloo-Ajabshir S, Heidari-Asil SA, Salavati-Niasari M (2022) Rapid and green combustion synthesis of nanocomposites based on Zn–Co–O nanostructures as photocatalysts for enhanced degradation of acid brown 14 contaminant under sunlight. Sep Purif Technol 280:119841. https://doi.org/10.1016/j.seppur.2021.119841
Mahdavi K, Zinatloo-Ajabshir S, Yousif QA, Salavati-Niasari M (2022) Enhanced photocatalytic degradation of toxic contaminants using Dy2O3-SiO2 ceramic nanostructured materials fabricated by a new, simple and rapid sonochemical approach. Ultrason Sonochem 82:105892. https://doi.org/10.1016/j.ultsonch.2021.105892
Hosseinzadeh G, Ghasemian N, Zinatloo-Ajabshir S (2022) TiO2/graphene nanocomposite supported on clinoptilolite nanoplate and its enhanced visible light photocatalytic activity. Inorg Chem Commun 136:109144. https://doi.org/10.1016/j.inoche.2021.109144
Tabatabaeinejada SM, Zinatloo-Ajabshir S, Amiric O, Salavati-Niasari M (2021) Magnetic Lu2Cu2O5-based ceramic nanostructured materials fabricated by a simple and green approach for an effective photocatalytic degradation of organic contamination. RSC Adv 11:40100–40111. https://doi.org/10.1039/d1ra06101a
Zinatloo-Ajabshir S, Heidari-Asil SA, Salavati-Niasari M (2021) Simple and eco-friendly synthesis of recoverable zinc cobalt oxide-based ceramic nanostructure as high-performance photocatalyst for enhanced photocatalytic removal of organic contamination under solar light. Sep Purif Technol 267:118667. https://doi.org/10.1016/j.seppur.2021.118667
Salehi Z, Zinatloo-Ajabshir S, Salavati-Niasari M (2016) Novel synthesis of Dy2Ce2O7 nanostructures via a facile combustion route. RSC Adv 6:26895–26901. https://doi.org/10.1039/C5RA27919D
Chang M, He L, Cai L (2018) An Overview of Genome-Wide Association Studies. Methods Mol Biol 1754:97–108. https://doi.org/10.1007/978-1-4939-7717-8_6
Wellcome Trust Case Control Consortium (2007) Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 447(7145):661–678. https://doi.org/10.1038/nature05911
Khatri B, Tessneer KL, Rasmussen A, Aghakhanian F, Reksten TR, Adler A, Alevizos I, Anaya JM, Aqrawi LA, Baecklund E, Brun JG, Bucher SM, Eloranta ML, Engelke F, Forsblad-d’Elia H, Glenn SB, Hammenfors D, Imgenberg-Kreuz J, Jensen JL, Johnsen SJA, Lessard CJ (2022) Genome-wide association study identifies Sjögren’s risk loci with functional implications in immune and glandular cells. Nat Commun 13(1):4287. https://doi.org/10.1038/s41467-022-30773-y
Vijayan SM, Kalaivani H, Mitra S, John J, Anila A, Damini Boban L, Chowdhury P, Gayen S (2022) Barriers to treatment regimen adherence in Indian women with polycystic ovarian syndrome. J Fam Med Prim Care 11:3687–3692. https://doi.org/10.4103/jfmpc.jfmpc_2360_21
Zhu YN, Zhang YT, Liu Q, Shen SM, Zou X, Cao YX (2020) Association analysis between the tag single nucleotide polymorphisms of DENND1A and the risk of polycystic ovary syndrome in Chinese Han women. BMC Med Genet 21(1):14. https://doi.org/10.1186/s12881-019-0945-1
Shukla P, Mukherjee S, Patil A, Joshi B (2022) Molecular characterization of variants in mitochondrial DNA encoded genes using next generation sequencing analysis and mitochondrial dysfunction in women with PCOS. Gene 855:147126. https://doi.org/10.1016/j.gene.2022.147126
Karen Nenonene E, Trottier-Lavoie M, Marchais M, Bastien A, Gilbert I, Macaulay AD, Khandjian EW, Maria Luciano A, Lodde V, Viger RS, Robert C (2023) Roles of the cumulus-oocyte transzonal network and the Fragile X protein family in oocyte competence. Reproduction (Cambridge, England) 165(2):209–219. https://doi.org/10.1530/REP-22-0165
Chen L, Hu M, Wang F, Yang Y, Huang Y, Zhou W, Sun X (2017) Genome-wide association study for SNPs associated with PCOS in human patients. Exp Ther Med 14(5):4896–4900. https://doi.org/10.3892/etm.2017.5113
Dai W, Zou X, Jia H, Peng Y, La B, Yan Z, Gao L, Qin L, Diao F, Ma X, Meng Y, Cui Y, Liu J (2022) Peroxiredoxin 4 secreted by cumulus cells ameliorates the maturation of oocytes in vitro. Biochem Biophys Res Commun 636(Pt 1):155–161. https://doi.org/10.1016/j.bbrc.2022.10.073
Nagy RA, van Montfoort A, Tietge U, Terpstra M, Kok K, van den Berg A, Hoek A, Kluiver J, Donker R (2019) Differential miRNA expression profiles in cumulus and mural granulosa cells from human pre-ovulatory follicles. Microrna 8(1):61–67. https://doi.org/10.2174/2211536607666180912152618
Karakaya C, Guzeloglu-Kayisli O, Hobbs RJ, Gerasimova T, Uyar A, Erdem M, Oktem M, Erdem A, Gumuslu S, Ercan D, Sakkas D, Comizzoli P, Seli E, Lalioti MD (2014) Follicle-stimulating hormone receptor (FSHR) alternative skip** of exon 2 or 3 affects ovarian response to FSH. Mol Hum Reprod 20(7):630–643. https://doi.org/10.1093/molehr/gau024
Han Y, Gao G, Li S, **ao N, Zhang Y, Luo H (2021) Development of an optimal protocol for isolation and purification of human granulosa cells in patients with different ovarian reserves. Exp Ther Med 22(3):938. https://doi.org/10.3892/etm.2021.10370
Diefenbach RJ, Lee JH, Kefford RF, Rizos H (2018) Evaluation of commercial kits for purification of circulating free DNA. Cancer Genet 228–229:21–27. https://doi.org/10.1016/j.cancergen.2018.08.005
Andrei D, Nagy RA, van Montfoort A, Tietge U, Terpstra M, Kok K, van den Berg A, Hoek A, Kluiver J, Donker R (2018) An improved primer set and amplification protocol with increased specificity and sensitivity targeting the Symbiodinium ITS2 region. PeerJ 6:e4816. https://doi.org/10.7717/peerj.4816
Santos K, Preussner M, Heroven AC, Weber G (2015) Crystallization and biochemical characterization of the human spliceosomal Aar2–Prp8RNaseH complex. Acta Crystallogr F Struct Biol Commun 71(Pt 11):1421–1428. https://doi.org/10.1107/S2053230X15019202
Peralta S, González-Quintana A, Ybarra M, Delmiro A, Pérez-Pérez R, Docampo J, Arenas J, Blázquez A, Ugalde C, Martín MA (2019) Novel ATAD3A recessive mutation associated to fatal cerebellar hypoplasia with multiorgan involvement and mitochondrial structural abnormalities. Mol Genet Metab 128(4):452–462. https://doi.org/10.1016/j.ymgme.2019.10.012
Nomoto H, Oohashi T, Hirakawa S, Ueki Y, Ohtsuki H, Ninomiya Y (2002) Human BRAL1 and BCAN genes that belong to the link-module superfamily are tandemly arranged on chromosome 1q21-23. Acta Med Okayama 56(1):25–29. https://doi.org/10.18926/AMO/31728
Hiatt SM, Thompson ML, Prokop JW, Lawlor JMJ, Gray DE, Bebin EM, Rinne T, Kempers M, Pfundt R, van Bon BW, Mignot C, Nava C, Depienne C, Kalsner L, Rauch A, Joset P, Bachmann-Gagescu R, Wentzensen IM, McWalter K, Cooper GM (2019) Deleterious variation in BRSK2 associates with a neurodevelopmental disorder. Am J Hum Genet 104(4):701–708. https://doi.org/10.18926/AMO/31728
Helbig KL, Lauerer RJ, Bahr JC, Souza IA, Myers CT, Uysal B, Schwarz N, Gandini MA, Huang S, Keren B, Mignot C, Afenjar A, Billette de Villemeur T, Héron D, Nava C, Valence S, Buratti J, Fagerberg CR, Soerensen KP, Kibaek M, Kamsteeg EJ, Koolen DA, Gunning B, Schelhaas HJ, Kruer MC, Fox J, Bakhtiari S, Jarrar R, Padilla-Lopez S, Lindstrom K, ** SC, Zeng X, Bilguvar K, Papavasileiou A, **ng Q, Zhu C, Boysen K, Vairo F, Lanpher BC, Klee EW, Tillema JM, Payne ET, Cousin MA, Kruisselbrink TM, Wick MJ, Baker J, Haan E, Smith N, Sadeghpour A, Davis EE, Katsanis N; Task Force for Neonatal Genomics; Corbett MA, MacLennan AH, Gecz J, Biskup S, Goldmann E, Rodan LH, Kichula E, Segal E, Jackson KE, Asamoah A, Dimmock D, McCarrier J, Botto LD, Filloux F, Tvrdik T, Cascino GD, Klingerman S, Neumann C, Wang R, Jacobsen JC, Nolan MA, Snell RG, Lehnert K, Sadleir LG, Anderlid BM, Kvarnung M, Guerrini R, Friez MJ, Lyons MJ, Leonhard J, Kringlen G, Casas K, El Achkar CM, Smith LA, Rotenberg A, Poduri A, Sanchis-Juan A, Carss KJ, Rankin J, Zeman A, Raymond FL, Blyth M, Kerr B, Ruiz K, Urquhart J, Hughes I, Banka S; Deciphering Developmental Disorders Study; Hedrich UBS, Scheffer IE, Helbig I, Zamponi GW, Lerche H, Mefford HC (2018) De novo pathogenic variants in CACNA1E cause developmental and epileptic encephalopathy with contractures, macrocephaly, and dyskinesias. Am J Hum Genet 103(5):666–678. https://doi.org/10.1016/j.ajhg.2018.09.006
Don AS, Rosen H (2009) A lipid binding domain in sphingosine kinase 2. Biochem Biophys Res Commun 380(1):87–92. https://doi.org/10.1016/j.bbrc.2009.01.075
Huttlin EL, Bruckner RJ, Navarrete-Perea J, Cannon JR, Baltier K, Gebreab F, Gygi MP, Thornock A, Zarraga G, Tam S, Szpyt J, Gassaway BM, Panov A, Parzen H, Fu S, Golbazi A, Maenpaa E, Stricker K, Guha Thakurta S, Zhang T, Rad R, Pan J, Nusinow DP, Paulo JA, Schweppe DK, Vaites LP, Harper JW, Gygi SP (2021) Dual proteome-scale networks reveal cell-specific remodeling of the human interactome. Cell 184(11):3022-3040.e28. https://doi.org/10.1016/j.cell.2021.04.011
Parenti I, Lehalle D, Nava C, Torti E, Leitão E, Person R, Mizuguchi T, Matsumoto N, Kato M, Nakamura K, de Man SA, Cope H, Shashi V; Undiagnosed Diseases Network; Friedman J, Joset P, Steindl K, Rauch A, Muffels I, van Hasselt PM, Petit F, Smol T, Le Guyader G, Bilan F, Sorlin A, Vitobello A, Philippe C, van de Laar IMBH, van Slegtenhorst MA, Campeau PM, Au PYB, Nakashima M, Saitsu H, Yamamoto T, Nomura Y, Louie RJ, Lyons MJ, Dobson A, Plomp AS, Motazacker MM, Kaiser FJ, Timberlake AT, Fuchs SA, Depienne C, Mignot C (2021) Missense and truncating variants in CHD5 in a dominant neurodevelopmental disorder with intellectual disability, behavioral disturbances, and epilepsy. Hum Genet 140(7):1109–1120. https://doi.org/10.1007/s00439-021-02283-2
Ferreira CR, **a ZJ, Clément A, Parry DA, Davids M, Taylan F, Sharma P, Turgeon CT, Blanco-Sánchez B, Ng BG, Logan CV, Wolfe LA, Solomon BD, Cho MT, Douglas G, Carvalho DR, Bratke H, Haug MG, Phillips JB, Wegner J, Tiemeyer M, Aoki K (2018) A recurrent de novo heterozygous COG4 substitution leads to Saul-Wilson syndrome, disrupted vesicular trafficking, and altered proteoglycan glycosylation. Am J Hum Genet 103(4):553–567. https://doi.org/10.1016/j.ajhg.2018.09.003
Suri F, Yazdani S, Chapi M, Safari I, Rasooli P, Daftarian N, Jafarinasab MR, Ghasemi Firouzabadi S, Alehabib E, Darvish H, Klotzle B, Fan JB, Turk C, Elahi E (2018) COL18A1 is a candidate eye iridocorneal angle-closure gene in humans. Hum Mol Genet 27(21):3772–3786. https://doi.org/10.1093/hmg/ddy256
Strohmaier J, Frank J, Wendland JR, Schumacher J, Jamra RA, Treutlein J, Nieratschker V, Breuer R, Mattheisen M, Herms S, Mühleisen TW, Maier W, Nöthen MM, Cichon S, Rietschel M, Schulze TG (2010) A reappraisal of the association between Dysbindin (DTNBP1) and schizophrenia in a large combined case-control and family-based sample of German ancestry. Schizophr Res 118(1–3):98. https://doi.org/10.1016/j.schres.2009.12.025
Teruhiko K, Yasuyuki K, Kenichiro A, Norihiro M, Jun K, Hiroshi T, Koichi T, Ryozo T, Isamu YK, Koichiro K, Toshihiro Y (2016) Association of Gln222Arg polymorphism in the deoxyribonuclease I (DNase I) gene with myocardial infarction in Japanese patients. Eur Heart J 27(17):2081–2087. https://doi.org/10.1093/eurheartj/ehl177
Harel T, Yesil G, Bayram Y, Coban-Akdemir Z, Charng WL, Karaca E, Al Asmari A, Eldomery MK, Hunter JV, Jhangiani SN, Rosenfeld JA, Pehlivan D, El-Hattab AW, Saleh MA, LeDuc CA, Muzny D, Boerwinkle E, Center B-H, for Mendelian Genomics; Gibbs RA, Chung WK, Yang Y, Belmont JW, Lupski JR (2016) Monoallelic and biallelic variants in EMC1 identified in individuals with global developmental delay, hypotonia, scoliosis, and cerebellar atrophy. Am J Hum Genet 98(3):562–570. https://doi.org/10.1016/j.ajhg.2016.01.011
Ahmed ZM, Jaworek TJ, Sarangdhar GN, Zheng L, Gul K, Khan SN, Friedman TB, Sisk RA, Bartles JR, Riazuddin S, Riazuddin S (2018) Inframe deletion of human ESPN is associated with deafness, vestibulopathy and vision impairment. J Med Genet 55(7):479–488. https://doi.org/10.1136/jmedgenet-2017-105221
Nomura T, Sandilands A, Akiyama M, Liao H, Evans AT, Sakai K, Ota M, Sugiura H, Yamamoto K, Sato H, Palmer CN, Smith FJ, McLean WH, Shimizu H (2007) Unique mutations in the filaggrin gene in Japanese patients with ichthyosis vulgaris and atopic dermatitis. J Allergy Clin Immunol 119(2):434–440. https://doi.org/10.1016/j.jaci.2006.12.646
Merner ND, Girard SL, Catoire H, Bourassa CV, Belzil VV, Rivière JB, Hince P, Levert A, Dionne-Laporte A, Spiegelman D, Noreau A, Diab S, Szuto A, Fournier H, Raelson J, Belouchi M, Panisset M, Cossette P, Dupré N, Bernard G, Chouinard S, Dion PA, Rouleau GA (2012) Exome sequencing identifies FUS mutations as a cause of essential tremor. Am J Hum Genet 91(2):313–319. https://doi.org/10.1016/j.ajhg.2012.07.002
Alvarez-Blasco F, Martínez-García MA, Luque-Ramírez M, Parraza N, San Millán JL, Escobar-Morreale HF (2009) Role of haptoglobin in polycystic ovary syndrome (PCOS), obesity and disorders of glucose tolerance in premenopausal women. PLoS ONE 4(5):e5606. https://doi.org/10.1371/journal.pone.0005606
Wu S, Hsu LA, Teng MS, Lin JF, Chang HH, Chang PY, Hu CF, Ko YL (2010) Association of matrix metalloproteinase 9 genotypes and cardiovascular disease risk factors with serum matrix metalloproteinase 9 concentrations in Taiwanese individuals. Clin Chem Lab Med 48(4):543–549. https://doi.org/10.1515/CCLM.2010.099
Jia Y, Persson C, Hou L, Zheng Z, Yeager M, Lissowska J, Chanock SJ, Chow H, Ye W (2010) A comprehensive analysis of common genetic variation in MUC1, MUC5AC, MUC6 genes and risk of stomach cancer. Cancer Causes Control 21(2):313–321. https://doi.org/10.1007/s10552-009-9463-3
Chu AY, Coresh J, Arking DE, Pankow JS, Tomaselli GF, Chakravarti A, Post WS, Spooner PH, Boerwinkle E, Kao WH (2010) NOS1AP variant associated with incidence of type 2 diabetes in calcium channel blocker users in the Atherosclerosis Risk in Communities (ARIC) study. Diabetologia 53(3):510–516. https://doi.org/10.1007/s00125-009-1608-0
Fujita A, Tsukaguchi H, Koshimizu E, Nakazato H, Itoh K, Kuraoka S, Komohara Y, Shiina M, Nakamura S, Kitajima M, Tsurusaki Y, Miyatake S, Ogata K, Iijima K, Matsumoto N, Miyake N (2018) Homozygous splicing mutation in NUP133 causes Galloway-Mowat syndrome. Ann Neurol 84(6):814–828. https://doi.org/10.1002/ana.25370
Monnot S, Serre V, Chadefaux-Vekemans B, Aupetit J, Romano S, De Lonlay P, Rival JM, Munnich A, Steffann J, Bonnefont JP (2009) Structural insights on pathogenic effects of novel mutations causing pyruvate carboxylase deficiency. Hum Mutat 30(5):734–740. https://doi.org/10.1002/humu.20908
McMillin MJ, Beck AE, Chong JX, Shively KM, Buckingham KJ, Gildersleeve HI, Aracena MI, Aylsworth AS, Bitoun P, Carey JC, Clericuzio CL, Crow YJ, Curry CJ, Devriendt K, Everman DB, Fryer A, Gibson K, Giovannucci Uzielli ML, Graham JM Jr, Hall JG, Hecht JT, Heidenreich RA, Hurst JA, Irani S, Krapels IP, Leroy JG, Mowat D, Plant GT, Robertson SP, Schorry EK, Scott RH, Seaver LH, Sherr E, Splitt M, Stewart H, Stumpel C, Temel SG, Weaver DD, Whiteford M, Williams MS, Tabor HK, Smith JD, Shendure J, Nickerson DA; University of Washington Center for Mendelian Genomics; Bamshad MJ (2014) Mutations in PIEZO2 cause Gordon syndrome, Marden-Walker syndrome, and distal arthrogryposis type 5. Am J Hum Gene 94(5):734–744. https://doi.org/10.1016/j.ajhg.2014.03.015
Schizophrenia Psychiatric Genome-Wide Association Study (GWAS) Consortium (2011) Genome-wide association study identifies five new schizophrenia loci. Nat Gene 43(10):969–976. https://doi.org/10.1038/ng.940
Ledford HA, Ren L, Thai PN, Park S, Timofeyev V, Sirish P, Xu W, Emigh AM, Priest JR, Perez MV, Ashley EA, Yarov-Yarovoy V, Yamoah EN, Zhang XD, Chiamvimonvat N (2022) Disruption of protein quality control of the human ether-à-go-go related gene K+ channel results in profound long QT syndrome. Heart Rhythm 19(2):281–292. https://doi.org/10.1016/j.hrthm.2021.10.005
Pinto D, Pagnamenta AT, Klei L, Anney R, Merico D, Regan R, Conroy J, Magalhaes TR, Correia C, Abrahams BS, Almeida J, Bacchelli E, Bader GD, Bailey AJ, Baird G, Battaglia A, Berney T, Bolshakova N, Bölte S, Bolton PF, Bourgeron T, Brennan S, Brian J, Bryson SE, Carson AR, Casallo G, Casey J, Chung BH, Cochrane L, Corsello C, Crawford EL, Crossett A, Cytrynbaum C, Dawson G, de Jonge M, Delorme R, Drmic I, Duketis E, Duque F, Estes A, Farrar P, Fernandez BA, Folstein SE, Fombonne E, Freitag CM, Gilbert J, Gillberg C, Glessner JT, Goldberg J, Green A, Green J, Guter SJ, Hakonarson H, Heron EA, Hill M, Holt R, Howe JL, Hughes G, Hus V, Igliozzi R, Kim C, Klauck SM, Kolevzon A, Korvatska O, Kustanovich V, Lajonchere CM, Lamb JA, Laskawiec M, Leboyer M, Le Couteur A, Leventhal BL, Lionel AC, Liu XQ, Lord C, Lotspeich L, Lund SC, Maestrini E, Mahoney W, Mantoulan C, Marshall CR, McConachie H, McDougle CJ, McGrath J, McMahon WM, Merikangas A, Migita O, Minshew NJ, Mirza GK, Munson J, Nelson SF, Noakes C, Noor A, Nygren G, Oliveira G, Papanikolaou K, Parr JR, Parrini B, Paton T, Pickles A, Pilorge M, Piven J, Ponting CP, Posey DJ, Poustka A, Poustka F, Prasad A, Ragoussis J, Renshaw K, Rickaby J, Roberts W, Roeder K, Roge B, Rutter ML, Bierut LJ, Rice JP, Salt J, Sansom K, Sato D, Segurado R, Sequeira AF, Senman L, Shah N, Sheffield VC, Soorya L, Sousa I, Stein O, Sykes N, Stoppioni V, Strawbridge C, Tancredi R, Tansey K, Thiruvahindrapduram B, Thompson AP, Thomson S, Tryfon A, Tsiantis J, Van Engeland H, Vincent JB, Volkmar F, Wallace S, Wang K, Wang Z, Wassink TH, Webber C, Weksberg R, Wing K, Wittemeyer K, Wood S, Wu J, Yaspan BL, Zurawiecki D, Zwaigenbaum L, Buxbaum JD, Cantor RM, Cook EH, Coon H, Cuccaro ML, Devlin B, Ennis S, Gallagher L, Geschwind DH, Gill M, Haines JL, Hallmayer J, Miller J, Monaco AP, Nurnberger JI Jr, Paterson AD, Pericak-Vance MA, Schellenberg GD, Szatmari P, Vicente AM, Vieland VJ, Wijsman EM, Scherer SW, Sutcliffe JS, Betancur C (2010) Functional impact of global rare copy number variation in autism spectrum disorders. Nature 466(7304):368–372. https://doi.org/10.1038/nature09146
Yokoyama K, Urashima M, Ohkido I, Kono T, Yoshida T, Muramatsu M, Niu T, Hosoya T (2010) L-type voltage-dependent calcium channel alpha subunit 1C is a novel candidate gene associated with secondary hyperparathyroidism: an application of haplotype-based analysis for multiple linked single nucleotide polymorphisms. Nephron Clin Prac 115(4):c237–c243. https://doi.org/10.1159/000313481
Robinson P, Lipscomb S, Preston LC, Altin E, Watkins H, Ashley CC, Redwood C (2007) Mutations in fast skeletal troponin I, troponin T, and beta-tropomyosin that cause distal arthrogryposis all increase contractile function. FASEB 21(3):896–905. https://doi.org/10.1096/fj.06-6899com
Luck K, Kim DK, Lambourne L, Spirohn K, Begg BE, Bian W, Brignall R, Cafarelli T, Campos-Laborie FJ, Charloteaux B, Choi D, Coté AG, Daley M, Deimling S, Desbuleux A, Dricot A, Gebbia M, Hardy MF, Kishore N, Knapp JJ, Kovács IA, Lemmens I, Mee MW, Mellor JC, Pollis C, Pons C, Richardson AD, Schlabach S, Teeking B, Yadav A, Babor M, Balcha D, Basha O, Bowman-Colin C, Chin SF, Choi SG, Colabella C, Coppin G, D’Amata C, De Ridder D, De Rouck S, Duran-Frigola M, Ennajdaoui H, Goebels F, Goehring L, Gopal A, Haddad G, Hatchi E, Helmy M, Jacob Y, Kassa Y, Landini S, Li R, van Lieshout N, MacWilliams A, Markey D, Paulson JN, Rangarajan S, Rasla J, Rayhan A, Rolland T, San-Miguel A, Shen Y, Sheykhkarimli D, Sheynkman GM, Simonovsky E, Taşan M, Tejeda A, Tropepe V, Twizere JC, Wang Y, Weatheritt RJ, Weile J, **a Y, Yang X, Yeger-Lotem E, Zhong Q, Aloy P, Bader GD, De Las RJ, Gaudet S, Hao T, Rak J, Tavernier J, Hill DE, Vidal M, Roth FP, Calderwood MA (2020) A reference map of the human binary protein interactome. Nature 580(7803):402–408. https://doi.org/10.1038/s41586-020-2188-x
Chaki M, Airik R, Ghosh AK, Giles RH, Chen R, Slaats GG, Wang H, Hurd TW, Zhou W, Cluckey A, Gee HY, Ramaswami G, Hong CJ, Hamilton BA, Cervenka I, Ganji RS, Bryja V, Arts HH, van Reeuwijk J, Oud MM, Letteboer SJ, Roepman R, Husson H, Ibraghimov-Beskrovnaya O, Yasunaga T, Walz G, Eley L, Sayer JA, Schermer B, Liebau MC, Benzing T, Le Corre S, Drummond I, Janssen S, Allen SJ, Natarajan S, O’Toole JF, Attanasio M, Saunier S, Antignac C, Koenekoop RK, Ren H, Lopez I, Nayir A, Stoetzel C, Dollfus H, Massoudi R, Gleeson JG, Andreoli SP, Doherty DG, Lindstrad A, Golzio C, Katsanis N, Pape L, Abboud EB, Al-Rajhi AA, Lewis RA, Omran H, Lee EY, Wang S, Sekiguchi JM, Saunders R, Johnson CA, Garner E, Vanselow K, Andersen JS, Shlomai J, Nurnberg G, Nurnberg P, Levy S, Smogorzewska A, Otto EA, Hildebrandt F (2012) Exome capture reveals ZNF423 and CEP164 mutations, linking renal ciliopathies to DNA damage response signaling. Cell 150(3):533–548. https://doi.org/10.1016/j.cell.2012.06.028
Howng SL, Hsu HC, Cheng TS, Lee YL, Chang LK, Lu PJ, Hong YR (2004) A novel ninein-interaction protein, CGI-99, blocks ninein phosphorylation by GSK3beta and is highly expressed in brain tumors. FEBS Lett 566(1–3):162–168. https://doi.org/10.1016/j.febslet.2004.04.024
Yin X, Tang B, Mao X, Peng J, Zeng S, Wang Y, Jiang H, Li N (2018) The genotypic and phenotypic spectrum of PARS2-related infantile-onset encephalopathy. J Hum Genet 63(9):971–980. https://doi.org/10.1038/s10038-018-0478-z
Coric V, Feldman HH, Oren DA, Shekhar A, Pultz J, Dockens RC, Wu X, Gentile KA, Huang SP, Emison E, Delmonte T, D’Souza BB, Zimbroff DL, Grebb JA, Goddard AW, Stock EG (2010) Multicenter, randomized, double-blind, active comparator and placebo-controlled trial of a corticotropin-releasing factor receptor-1 antagonist in generalized anxiety disorder. Depress Anxiety 27(5):417–425. https://doi.org/10.1002/da.20695
Kuo CL, Goldberg AL (2017) Ubiquitinated proteins promote the association of proteasomes with the deubiquitinating enzyme Usp14 and the ubiquitin ligase Ube3c. Proc Natl Acad Sci U S A 114(17):E3404–E3413. https://doi.org/10.1073/pnas.1701734114
Wang W, Huang X, **n HB, Fu M, Xue A, Wu ZH (2015) TRAF Family Member-associated NF-κB Activator (TANK) inhibits genotoxic nuclear factor κB activation by facilitating deubiquitinase USP10-dependent deubiquitination of TRAF6 ligase. J Biol Chem 290(21):13372–13385. https://doi.org/10.1074/jbc.M115.643767
Lyons JJ, Yu X, Hughes JD, Le QT, Jamil A, Bai Y, Ho N, Zhao M, Liu Y, O’Connell MP, Trivedi NN, Nelson C, DiMaggio T, Jones N, Matthews H, Lewis KL, Oler AJ, Carlson RJ, Arkwright PD, Hong C, Agama S, Wilson TM, Tucker S, Zhang Y, McElwee JJ, Pao M, Glover SC, Rothenberg ME, Hohman RJ, Stone KD, Caughey GH, Heller T, Metcalfe DD, Biesecker LG, Schwartz LB, Milner JD (2016) Elevated basal serum tryptase identifies a multisystem disorder associated with increased TPSAB1 copy number. Nat Genet 48(12):1564–1569. https://doi.org/10.1038/ng.3696
Mäkitie LT, Kanerva K, Polvikoski T, Paetau A, Andersson LC (2010) Brain neurons express ornithine decarboxylase-activating antizyme inhibitor 2 with accumulation in Alzheimer’s disease. Brain Pathol 20(3):571–580. https://doi.org/10.1111/j.1750-3639.2009.00334.x
Tang Z, Shu H, Oncel D, Chen S, Yu H (2004) Phosphorylation of Cdc20 by Bub1 provides a catalytic mechanism for APC/C inhibition by the spindle checkpoint. Mol Cell 16(3):387–397. https://doi.org/10.1016/j.molcel.2004.09.031
Tsao TY, Tsai CS, Tung JN, Chen SL, Yue CH, Liao CF, Wang CC, Jiang MC (2009) Function of CSE1L/CAS in the secretion of HT-29 human colorectal cells and its expression in human colon. Mol Cell Biochem 327(1–2):163–170. https://doi.org/10.1007/s11010-009-0054-0
Xu H, Foltz L, Sha Y, Madlansacay MR, Cain C, Lindemann G, Vargas J, Nagy D, Harriman B, Mahoney W, Schueler PA (2001) Cloning and characterization of human erythroid membrane-associated protein, human ERMAP. Genomics 76(1–3):2–4. https://doi.org/10.1006/geno.2001.6600
Ward-Caviness CK, Neas LM, Blach C, Haynes CS, LaRocque-Abramson K, Grass E, Dowdy ZE, Devlin RB, Diaz-Sanchez D, Cascio WE, Miranda ML, Gregory SG, Shah SH, Kraus WE, Hauser ER (2017) A genome-wide trans-ethnic interaction study links the PIGR-FCAMR locus to coronary atherosclerosis via interactions between genetic variants and residential exposure to traffic. PLoS ONE 12(3):e0173880. https://doi.org/10.1371/journal.pone.0173880
Cristina C, Mia H, Lorenzo S, Mari N, Andres M, Pagona L, Dimitrios T, Wolfgang A, Iris P, Franco M, Lorenzo R, Renato T, Luigi B, Gary JM, Tatiana VM, Ivana H, Vladimir B, Simone B, Christine B, Kristina K, Ray L, Antonio A, Xavier C, David IC, Patricia AM, Ariana Z, Bernard EM, Claire MH, Manuela M, Paul B (2009) Genetic associations of 115 polymorphisms with cancers of the upper aerodigestive tract across 10 European countries: the ARCAGE project. Cancer Res 69(7):2956–2965. https://doi.org/10.1158/0008-5472.CAN-08-2604
Shrestha RL, Draviam VM (2013) Lateral to end-on conversion of chromosome-microtubule attachment requires kinesins CENP-E and MCAK. Curr Bio 23(16):1514–1526. https://doi.org/10.1016/j.cub.2013.06.040
Pasmooij AM, Pas HH, Bolling MC, Jonkman MF (2007) Revertant mosaicism in junctional epidermolysis bullosa due to multiple correcting second-site mutations in LAMB3. J Clin Invest 117(5):1240–1248. https://doi.org/10.1172/JCI30465
Platzer K, Sticht H, Edwards SL, Allen W, Angione KM, Bonati MT, Brasington C, Cho MT, Demmer LA, Falik-Zaccai T, Gamble CN, Hellenbroich Y, Iascone M, Kok F, Mahida S, Mandel H, Marquardt T, McWalter K, Panis B, Pepler A, Pinz H, Ramos L, Shinde DN, Smith-Hicks C, Stegmann APA, Stöbe P, Stumpel CTRM, Wilson C, Lemke JR, Di Donato N, Miller KG, Jamra R (2019) De Novo Variants in MAPK8IP3 Cause Intellectual Disability with Variable Brain Anomalies. Am J Hum Genet 104(2):203–212. https://doi.org/10.1016/j.ajhg.2018.12.008
Onda M, Nagata S, Ho M, Bera TK, Hassan R, Alexander RH, Pastan I (2006) Megakaryocyte potentiation factor cleaved from mesothelin precursor is a useful tumor marker in the serum of patients with mesothelioma. Clin Cancer Res 12(14 Pt 1):4225–4231. https://doi.org/10.1158/1078-0432.CCR-06-0472
Stolk L, van Meurs JB, Arp PP, Hofman A, Pols HA, Uitterlinden AG (2008) The RIZ Pro704 insertion-deletion polymorphism, bone mineral density and fracture risk: the Rotterdam study. Bone 42(2):286–293. https://doi.org/10.1016/j.bone.2007.10.008
Rose JE, Behm FM, Drgon T, Johnson C, Uhl GR (2010) Personalized smoking cessation: interactions between nicotine dose, dependence and quit-success genotype score. Mol Med 16(7–8):247–253. https://doi.org/10.2119/molmed.2009.00159
Hoefele J, Sudbrak R, Reinhardt R, Lehrack S, Hennig S, Imm A, Muerb U, Utsch B, Attanasio M, O’Toole JF, Otto E, Hildebrandt F (2005) Mutational analysis of the NPHP4 gene in 250 patients with nephronophthisis. Hum Mutat 25(4):411. https://doi.org/10.1002/humu.9326
Hasin Y, Seldin M, Lusis A (2017) Multi-omics approaches to disease. Genome Biol 18(1):83. https://doi.org/10.1186/s13059-017-1215-1
Applegate CD, Schiettecatte F, Hamosh A, Amberger JS (2022) Exploring genes and phenotypes within chromosomal regions using OMIM’s GeneScout. Curr Protoc 2(9):e530. https://doi.org/10.1002/cpz1.530
Mandell JD, Cannataro VL, Townsend JP (2023) Estimation of neutral mutation rates and quantification of somatic variant selection using canceffectsizeR. Cancer Res 83(4):500–505. https://doi.org/10.1158/0008-5472.CAN-22-1508
Pan B, Kusko R, **ao W, Zheng Y, Liu Z, **ao C, Sakkiah S, Guo W, Gong P, Zhang C, Ge W, Shi L, Tong W, Hong H (2019) Similarities and differences between variants called with human reference genome HG19 or HG38. BMC Bioinform 20(Suppl 2):101. https://doi.org/10.1186/s12859-019-2620-0
Thathapudi S, Kodati V, Erukkambattu J, Katragadda A, Addepally U, Hasan Q (2014) Tumor necrosis factor-alpha and polycystic ovarian syndrome: a clinical, biochemical, and molecular genetic study. Genet Test Mol Biomark 18(9):605–609. https://doi.org/10.1089/gtmb.2014.0151
Yabluchanskiy A, Ma Y, Iyer RP, Hall ME, Lindsey ML (2013) Matrix metalloproteinase-9: Many shades of function in cardiovascular disease. Physiology (Bethesda) 28(6):391–403. https://doi.org/10.1152/physiol.00029.2013
MacKellar M, Vigerust DJ (2016) Role of haptoglobin in health and disease: a focus on diabetes. Clin Diabete 34(3):148–157. https://doi.org/10.2337/diaclin.34.3.148
Carvalho LML, Ferreira CN, de Oliveira DKD, Rodrigues KF, Duarte RCF, Teixeira MFA, Xavier LB, Candido AL, Reis FM, Silva IFO, Campos FMF, Gomes KB (2017) Haptoglobin levels, but not Hp1-Hp2 polymorphism, are associated with polycystic ovary syndrome. J Assist Reprod Genet 34(12):1691–1698. https://doi.org/10.1007/s10815-017-1030-3
Cardoso-Moreira M, Halbert J, Valloton D, Velten B, Chen C, Shao Y, Liechti A, Ascenção K, Rummel C, Ovchinnikova S, Mazin PV, Xenarios I, Harshman K, Mort M, Cooper DN, Sandi C, Soares MJ, Ferreira PG, Afonso S, Carneiro M, Turner JMA, VandeBerg JL, Fallahshahroudi A, Jensen P, Behr R, Lisgo S, Lindsay S, Khaitovich P, Huber W, Baker J, Anders S, Zhang YE, Kaessmann H (2019) Gene expression across mammalian organ development. Nature 571(7766):505–509. https://doi.org/10.1038/s41586-019-1338-5
Hsu SY (1999) Cloning of two novel mammalian paralogs of relaxin/insulin family proteins and their expression in testis and kidney. Mol Endocrinol 13(12):2163–2174. https://doi.org/10.1210/mend.13.12.0388
Wu RC, Zeng Y, Pan IW, Wu MY (2015) Androgen receptor coactivator ARID4B is required for the function of sertoli cells in spermatogenesis. Mol Endocrinol 29(9):1334–1346. https://doi.org/10.1210/me.2015-1089
Polli A, Hendrix J, Ickmans K, Bakusic J, Ghosh M, Monteyne D, Velkeniers B, Bekaert B, Nijs J, Godderis L (2022) Genetic and epigenetic regulation of Catechol-O-methyltransferase in relation to inflammation in chronic fatigue syndrome and Fibromyalgia. J Transl Med 20(1):487. https://doi.org/10.1186/s12967-022-03662-7
Pu W, Han X, He L, Li Y, Huang X, Zhang M, Lv Z, Yu W, Wang QD, Cai D, Wang J, Sun R, Fei J, Ji Y, Nie Y, Zhou B (2020) A genetic system for tissue-specific inhibition of cell proliferation. Development (Cambridge, England) 147(4):dev183830. https://doi.org/10.1242/dev.183830
Bonini S, Mantelli F, Moretti C, Lambiase A, Bonini S, Micera A (2007) Itchy-dry eye associated with polycystic ovary syndrome. Am J Ophthalmol 143(5):763–771. https://doi.org/10.1016/j.ajo.2007.01.030
Chettiankandy TJ, Sachdev SS, Khandekar SP, Dive A, Nagpal D, Tupkari JV (2022) Role of Nidogen-2 in diagnosis and prognosis of head and neck squamous cell carcinoma: a systematic review. J Oral Maxillofac Pathol 26(3):382–388. https://doi.org/10.4103/jomfp.jomfp_293_22
Wang H, Xu J, Lazarovici P, Quirion R, Zheng W (2018) cAMP response element-binding Protein (CREB): a possible signaling molecule link in the pathophysiology of schizophrenia. Front Mol Neurosci. https://doi.org/10.3389/fnmol.2018.00255
Szczałuba K, Biernacka A, Szymańska K, Gasperowicz P, Kosińska J, Rydzanicz M, Płoski R (2018) Novel GNB1 de novo mutation in a patient with neurodevelopmental disorder and cutaneous mastocytosis: clinical report and literature review. Eur J Med Genet 61(3):157–160. https://doi.org/10.1016/j.ejmg.2017.11.010
Zhang P, Gao H, Ye C, Yan R, Yu L, **a C, Yang D (2022) Large-scale transcriptome data analysis identifies KIF2C as a potential therapeutic target associated with immune infiltration in prostate cancer. Front Immunol 13:905259. https://doi.org/10.3389/fimmu.2022.905259
Cheng Y, Jiao L, Li W, Wang J, Lin Z, Lai H, Ying B (2021) Collagen type XVIII alpha 1 chain (COL18A1) variants affect the risk of anti-tuberculosis drug-induced hepatotoxicity: A prospective study. J Clin Lab Anal 35(2):3630. https://doi.org/10.1002/jcla.23630
Nilsson E, Benrick A, Kokosar M, Krook A, Lindgren E, Källman T, Martis MM, Højlund K, Ling C, Stener-Victorin E (2018) Transcriptional and epigenetic changes influencing skeletal muscle metabolism in women with polycystic ovary syndrome. J Clin Endocrinol Metal 103(12):4465–4477. https://doi.org/10.1210/jc.2018-00935
Geuens T, Bouhy D, Timmerman V (2016) The hnRNP family: insights into their role in health and disease. Hum Genet 135:851–867. https://doi.org/10.1007/s00439-016-1683-5
Liu Z, Xu X, Chen D, Zhang L, Pan Y, Liu D, Shen M, Chen M (2022) Circ_0022340 promotes colorectal cancer progression via HNRNPC/EBF1/SYT7 or miR-382–5p/ELK1 axis. Cell Mol Biol 68(7):107–116. https://doi.org/10.14715/cmb/2022.68.7.18
Pant P, Chitme HR (2020) Inflammation and ovulation, Edited by Hassan Abduljabbar, Fibroids. IntechOpen. https://doi.org/10.5772/intechopen.94107
Gairola N, Deorari M, Jakhmola V, Sircar R, Chitme HR (2022) Human follicular fluid, clinical use of proteomics analysis in identification of infertility. Indian J Pharm Edu Res 56(4):917–923. https://doi.org/10.5530/ijper.56.4.173
Acknowledgements
We take this opportunity to thank all volunteers involved in the study. We also acknowledge thanks to Mr. Ajeet Sharma, Mr. Nitin Kataria, Mr. Achal Tiwari, Ms. Laxmi Arya and all other technical and non-technical staff of Morpheus Prasad International IVF Centre and Indira IVF Fertility Centre, Dehradun for their help and support throughout the study. We also thank Dr. Shashi Bhushan Tripathi, TERI School of Advanced Studies, Delhi and Dr. Anoop Anand Malik, TERI, Guwahati. This research was financially supported by the Bayer Pharmaceuticals, Germany and Seed Grant of DIT University, Dehradun—India.
Funding
This research was supported by the Bayer Pharmaceuticals (Grant No. 2019-09-2438), Germany and Seed Grant of DIT University, Dehradun—India.
Author information
Authors and Affiliations
Contributions
All authors have equally contributed in conducting the study and prepare the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Present study is approved by University Research Ethics Committee of DIT University, Dehradun. Informed consent form was taken from all volunteers for participation and publication of study outcome.
Consent to participate
The informed consent to participate in the study was obtained from the participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pant, P., Chitme, H., Sircar, R. et al. Genome-wide association study for single nucleotide polymorphism associated with mural and cumulus granulosa cells of PCOS (polycystic ovary syndrome) and non-PCOS patients. Futur J Pharm Sci 9, 27 (2023). https://doi.org/10.1186/s43094-023-00475-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-023-00475-3