Abstract
Background
False negative myocardial perfusion images on single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is a substantial problem in the interpretation of MPI. To explore possible parameters from gated SPECT that could detected coronary artery disease (CAD) in patients with normal perfusion images, we retrospectively selected patients who underwent a 2-day Tc-99 m MIBI adenosine stress/rest MPI and a subsequent invasive coronary angiography. Gated SPECT parameters, including end systolic volume (ESV), end diastolic volume (EDV), left ventricular ejection fraction (LVEF), and transient ischemic dilation (TID) ratio of patients with and without CAD were compared and assessed for their respective diagnostic performance using receiver operating characteristics (ROC) area under the curve (AUC).
Results
Among 22 patients with normal perfusion images, 7 patients had CAD. Despite the small number of patients, we found significant differences between the ESV, the EDV, and the LVEF between patients with and without CAD. The analysis of ROC curve showed the stress ESV could excellently detect CAD (AUC = 0.900). The rest ESV, the stress EDV, the rest EDV, the stress LVEF and the rest LVEF could likewise perform well in the detection of CAD (AUC = 0.833, 0.819, 0.790, 0.862, and 0.838, respectively). In contrast, the change in LVEF and the TID ratio (AUC = 0.667 and 0.524, respectively) did not seem as reliable as other parameters. Optimal cutoffs for detection of CAD in patients with normal perfusion images from our study were ≥ 20.0 mL for the stress ESV, ≥ 71.0 mL for the stress EDV, ≤ 66.3 EF units for the stress LVEF, ≥ 18.0 mL for the rest ESV, ≥ 67.0 mL for the rest EDV and ≤ 70.0 EF unit for the rest LVEF.
Conclusions
Gated SPECT parameters could facilitate detection of CAD in patient with normal perfusion images on Tc-99m MIBI MPI. These parameters should be carefully interpreted to improve diagnostic accuracy and reduce false negative MPI.
Similar content being viewed by others
Background
Presence of coronary artery disease (CAD) in patients with normal perfusion images is a major limitation of radionuclide myocardial perfusion imaging (MPI) [1]. The causes of those false negative perfusion images can be attributed to multiple causes. Some causes, such as inadequate stress, image acquisition errors, and imaging artifacts, can be prevented through careful patient preparation and proper imaging technique. Others, unfortunately, are inherent limitations of perfusion image interpretation and are more challenging to overcome [2].
Several newer techniques has been developed to improve the accuracy of MPI, many of those techniques were not feasible for widespread adoption. The incremental value of absolute myocardial blood flow quantitation from either positron emission tomography (PET) or single-photon emission computed tomography (SPECT) MPI was very promising but required the installment of costly scanner system and well-trained experienced personnel [3,4,5]. Integration of calcium score to the interpretation of MPI could also improve diagnostic accuracy but might involve an additional separate imaging and increase the radiation exposure to the patients [6].
Gated SPECT parameters can be obtained by most imaging system used for MPI and are potentially useful to circumvent the false negative perfusion images. These parameters include end systolic volume (ESV), end diastolic volume (EDV), left ventricular ejection fraction (LVEF), LVEF response to stress, and transient ischemic dilation (TID) ratio. Unfortunately, the results of past studies were highly inconsistent and no consensus was reached on the optimum cutoffs for those parameters [7]. Moreover, not many studies, explored the diagnostic values of those parameters specifically in patients with normal perfusion images.
In the current study, we intended to examine the utility of gated SPECT parameters in the detection of CAD in patients with normal perfusion images by calculating the diagnostic values of those parameters from Tc-99 m MIBI MPI.
Methods
Study population
We retrospectively included patients who underwent Tc-99m MIBI SPECT MPI from January 2013 to December 2016 and underwent invasive coronary angiography (ICA) within 9 months after the MPI. The Institutional Review Board approved the protocols and waived the informed consent requirement.
SPECT MPI protocols and acquisition
The SPECT MPI was performed with a 2-day adenosine stress/rest protocol. On the stress day, the patient was infused with 140 mcg/kg/min of adenosine for 6 min. Twenty to thirty mCi of Tc-99m MIBI was injected at the forth minute of the adenosine infusion. Approximately 1 h later the SPECT was acquired. The rest SPECT was acquired on another day with the same dose of Tc-99m MIBI and the same interval of uptake time.
Attenuation correction with low dose computed tomography (CT) and electrocardiography (ECG)-gated SPECT were done in all patients. Both the post stress and the rest SPECT were acquired using the same a dual-head gamma camera SPECT/CT system (Symbia T6, Siemens, Erlangen, Germany).
SPECT MPI processing and interpretation
Perfusion images from non-gated SPECT were displayed in short, horizontal long, vertical long, and 17-segment polar map views. Two experienced nuclear medicine physicians blinded to the clinical history interpreted the perfusion images. A 5-point ordinal score of 0–4 was applied to each of the 17 segments based on the relative uptake. The score 0 represented normal uptake and the score 4 represented absent of uptake in the segment. Summed stress score (SSS) and summed rest score (SRS) were the summed of the scores in all segments from the polar map of the stress and the rest SPECT, respectively. Summed difference score (SDS) was calculated by subtracting the SRS from the SDS. The SSS of ≤ 3 was interpreted as normal perfusion images [8].
The gated SPECT was processed using a commercially-available Quantitative-Gated SPECT (QGS) software. The software calculated the ESV, the EDV, the LVEF using edge-detection algorithm. The LVEF response to stress was expressed in delta LVEF value (ΔEF), which was calculated by subtracting the rest LVEF from the stress LVEF. Transient ischemic dilation (TID) ratio was calculated by dividing the left ventricular volume after stress by the left ventricular volume at rest.
Invasive coronary angiography
Board-certified intervention cardiologists performed and interpreted the ICA of all patients. In the current study, any 50% or more stenosis of the left main coronary artery or any 70% or more stenosis of other major coronary arteries was considered positive for CAD.
Statistical analysis
All statistical analyses were performed using R statistical packages. Continuous variables were displayed as mean ± standard deviation. The Wilcoxon rank-sum test was used for comparison of data with non-normal distribution. Receiver operating characteristics (ROC) area under the curve (AUC) with 95% confidence interval (95% CI) was used for assessment of diagnostic performance and determination of optimal cutoffs. P value < 0.05 was considered statistical significant.
Results
Baseline characteristics
Total of 22 patients with normal perfusion images from 117 patients who underwent ICA and 801 patients who underwent MPI were included. Mean age of the patients was 72.2 ± 9.85 years. Seven patients (31.8%) had CAD, 9 patients (40.9%) were female. Four patients (18.2%) had history of PCI (Table 1). The median interval between MPI and ICA was 2 months (range < 1–9 months). There were no significant differences in SSS (p = 0.323), SRS (p = 0.680), or SDS (p = 0.054) between patients with CAD and without CAD.
Gated SPECT findings
Mean stress ESV was 34.5 ± 18.7 mL in patients with CAD and 17.3 ± 7.34 mL in patients without CAD. The stress ESV was significantly greater in patients with CAD (p = 0.002). Mean rest ESV was 31.4 ± 23.1 mL in patients with CAD and 15.3 ± 6.84 in patient without CAD. The rest ESV was significantly greater in patients with CAD (p = 0.007). Mean stress EDV was 81.7 ± 17.9 mL in patients with CAD and 61.2 ± 14.5 in patients without CAD. The stress EDV was significantly greater in patients with CAD (p = 0.002). Mean rest EDV was 80.7 ± 24.0 mL in patients with CAD and 60.1 ± 16.0 in patients without CAD. The rest EDV was significantly greater in patients with CAD (p = 0.017).
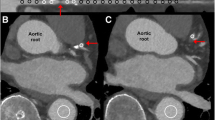
Mean stress LVEF was 59.0 ± 13.3 EF units in patients with CAD and 72.5 ± 6.41 in patients without CAD. Mean rest LVEF was 63.5 ± 14.6 EF units in patients with CAD and 75.2 ± 5.73 in patients without CAD. Both the stress and the rest LVEF in patient with CAD were significantly lower. (p = 0.004) (Fig. 1).
The mean ΔEF was − 4.56 ± 2.13 EF units in patients with CAD and − 2.73 ± 3.24 EF units in patients without CAD. Mean TID ratio was 1.04 ± 0.14 in patients with CAD and 1.04 ± 0.16 in patients without CAD. Between patients with and without CAD, there were no significant differences in either the ΔLVEF (p = 0.273) or the TID ratio (p = 0.891) (Fig. 2).
Diagnostic performance
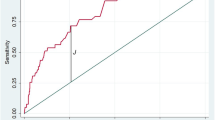
The AUC was 0.900 (95% CI 0.767–1) from the stress ESV, 0.819 (95% CI 0.625–1) from the rest ESV, 0.862 (95% CI 0.699–1) from the stress LVEF, 0.833 (95% CI 0.663–1) from the rest ESV, 0.790 (95% CI 0.559–1) from the rest EDV, 0.838 (95% CI 0.664–1) from the rest LVEF, 0.667 (95% CI 0.429–0.904) from the ΔEF, and 0.524 (95% CI 0.235–0.813) from the TID ratio (Fig. 3).
Between the parameters derived from the stress and the rest-gated SPECT, there were no significant differences in the AUC of the ESV (p = 0.209), the EDV (p = 0.501), and the LVEF (p = 0.640). The AUC of TID ratio was significantly less than the AUC of stress ESV (p = 0.004), stress EDV (p = 0.022), stress LVEF (p = 0.007), rest ESV (p = 0.004), rest EDV (p = 0.020), and rest LVEF (p = 0.009). There were no significance differences in the AUC of the ΔEF and the TID ratio (p = 0.532).
Optimum cutoffs were ≥ 20.0 mL for the stress ESV (sensitivity = 100%, specificity = 73.3%), ≥ 71.0 mL for the stress EDV (sensitivity = 85.7%, specificity = 80.0%), ≤ 66.3 EF units for the stress LVEF (sensitivity = 71.4%, specificity = 80.0%), ≥ 18.0 mL for the rest ESV (sensitivity = 85.7%, specificity = 73.3%), ≥ 67.0 mL for the rest EDV (sensitivity = 85.7%, specificity = 73.3%), and ≤ 70.0 EF unit for the rest LVEF (sensitivity = 71.4%, specificity = 73.3%).
Discussion
Our study examined the values of various gated SPECT parameters in the detection of CAD in patients with normal perfusion images using ROC AUC analysis. The AUC categorized the stress ESV as an excellent classifier and categorized all the stress EDV, the stress EF, the rest ESV, and the rest EF as good classifiers. Together with a closer inspection of the confident intervals of each parameters, the stress ESV was likely the most reliable parameter. In contrast, both the ΔEF and the TID ratio were not useful in detection of CAD in patients with normal perfusion images in our cohort.
Our result emphasized that the calculated left ventricular volumes, particularly the stress ESV, and the LVEF are valuable for detection of CAD in patients with normal perfusion images (Fig. 4). This was concordant with the finding of Peix, who found that the EDV of patients with ischemic were approximately 50% higher than those of patients without ischemic and the ESV of patients with ischemic were almost twice as high as those without ischemic [9]. We further strengthened those findings by the inclusion of ICA as a reference standard and proposed the possible cutoffs for those values. We postulated that the larger volumes of the left ventricle in patients with CAD might represent the impaired contractile function of the ischemic myocardium and the contractility dysfunction might be exacerbated by the stunning of myocardium after stress [9]. It was also possible that the subendocardial ischemic contributed to the apparently larger stress ESV in patients with CAD [10].
TID ratio and ΔEF were long believed to be crucial ancillary findings that could indicate the presence of CAD but our result indicated otherwise. TID is a phenomenon in which the left ventricular cavity after stress appears larger than the cavity at rest. It was thought to be a result of subendocardial ischemic or myocardial stunning. Increased TID ratio in patients with perfusion defects was proven to be a good indicator of severe CAD. However, there has been conflicting evidence on the utility of TID ratio in patients with normal perfusion images. Some studies suggest that increased TID ratio was a strong predictor for CAD in patients without apparent perfusion defect [11, 12]. Others found that high TID ratio in the otherwise normal perfusion images did not correlate with CAD [13, 14]. Many researchers speculated that the inconsistency resulted from the differences in stress protocols, radiotracers, and imaging techniques. Because a meta-analysis found that diagnostic values of TID ratio was remarkably poorer in vasodilator stress compared to those in exercise stress (AUC = 0.78. vs AUC = 0.92) [10], we suspected that the exclusive use of vasodilator stress in our cohort could be one culprit for the poor diagnostic performance of TID ratio in our study. The interpretation of ΔEF was similarly controversial and several cutoffs have been proposed to indicate abnormal EF response to stress. A publication form the International Atomic Energy Agency (IAEA) stated that the post stress LVEF that was at least 10 EF units lower than rest LVEF indicated abnormal EF response [8] but a more recent study proposed a smaller threshold at 5 EF units [9]. Because the EF response gradually faded after stress and it was found that the normalization of post stress LVEF could occur as early as 13 min [15]. The explanation for the poor diagnostic performance of ΔEF in our study was most likely the 1-h-long interval before the image acquisition.
Several limitations of this study were noticeable. First, it should be reminded that perfusion defect on perfusion images is still the most crucial findings for diagnosis of CAD from the MPI [16]. Although up to 7.2% of patients with normal perfusion images had CAD [12], correctable causes of false negative perfusion images must be excluded before the perfusion be considered normal. These causes include, but not limited to, unrecognized ingestion of caffeine-containing products, insufficient coronary vasodilatation, motion artifacts, and attenuation artifacts [2].
Secondly, our sample size was rather small, which could hamper the precision of our result and reduce our ability to detect the differences in diagnostic values among the examined parameters. The limitations resulted from the stringent need for the ICA, which was not frequently done in patient with normal perfusion images. Inclusion of alternative reference standard, such as clinical information after sufficient follow up may increase the number of eligible subjects and improve the precision of future study.
Thirdly, due to the small sample size, we could not provide gender specific cutoffs for the gated SPECT parameters. There has been plenty of evidences showing that the reference ranges for gated SPECT parameters could differ significantly between sexes and ethnicities. A study from Germany established normal ranges of 41–47 mL, 102–111 mL, and 51–55 EF units for ESV, EDV and LVEF in women and 68–89 mL, 150–170 mL, and 45–50 EF units for the respective values in men [17]. In contrast, the Japanese Nuclear Society working group published normal ranges of 1–30 mL, 32–86 mL, and 60–90 EF units for ESV, EDV and LVEF in women and 8–47 mL, 42–120 mL and 54–80 EF units in men [18]. Both the German and the Japanese studies demonstrated significant different gated SPECT parameters between women and men, which was consistent with many other studies [19]. With larger sample size in future studies, we hope to establish sex specific reliable cutoffs of the gated SPECT parameters, which will further improve the accuracy of MPI in the detection of CAD.
Conclusions
Gated SPECT parameters, particularly stress ESV could help detection of CAD in patients with normal perfusion images and should be carefully examined to prevent false negative, enhance the diagnostic accuracy, and improve outcomes of the patients.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Area under the curve
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- ECG:
-
Electrocardiography
- EDV:
-
End diastolic volume
- ESV:
-
End systolic volume
- IAEA:
-
International Atomic Energy Agency
- ICA:
-
Invasive coronary angiography
- LVEF:
-
Left ventricular ejection fraction
- MPI:
-
Myocardial perfusion imaging
- PET:
-
Positron emission tomography
- QGS:
-
Quantitative-Gated SPECT
- ROC:
-
Receiver operating characteristics
- SD:
-
Standard deviation
- SDS:
-
Summed difference score
- SPECT:
-
Single-photon emission computed tomography
- SRS:
-
Summed rest score
- SSS:
-
Summed stress score
- TID:
-
Transient ischemic dilation
- ΔEF:
-
Delta LVEF value
References
Yokota S, Ottervanger JP, Mouden M, Timmer JR, Knollema S, Jager PL (2014) Prevalence, location, and extent of significant coronary artery disease in patients with normal myocardial perfusion imaging. J Nucl Cardiol 21(2):284–290
Hage FG, AlJaroudi WA (2017) Review of cardiovascular imaging in the journal of nuclear cardiology in 2016: Part 2 of 2-myocardial perfusion imaging. J Nucl Cardiol 24(4):1190–1199
Klein R, Hung GU, Wu TC, Huang WS, Li D, deKemp RA et al (2014) Feasibility and operator variability of myocardial blood flow and reserve measurements with 99mTc-sestamibi quantitative dynamic SPECT/CT imaging. J Nucl Cardiol 21(6):1075–1088
Liu FS, Wang SY, Shiau YC, Wu YW (2022) Integration of quantitative absolute myocardial blood flow estimates from dynamic CZT-SPECT improves the detection of coronary artery disease. J Nucl Cardiol 29(5):2311–2321
Nammas W, Maaniitty T, Knuuti J, Saraste A (2021) Cardiac perfusion by positron emission tomography. Clin Physiol Funct Imaging 41(5):385–400
Yuoness SA, Goha AM, Romsa JG, Akincioglu C, Warrington JC, Datta S et al (2015) Very high coronary artery calcium score with normal myocardial perfusion SPECT imaging is associated with a moderate incidence of severe coronary artery disease. Eur J Nucl Med Mol Imaging 42(10):1542–1550
Camilletti J, Erriest J, Espinola-Zavaleta N, Hernández-Sandoval S, Redolatti M, Cartasegna L et al (2020) Left ventricular dyssynchrony and abnormalities in wall motion, assessed by gated-SPECT as ischemic auxiliary markers. J Nucl Cardiol 27(6):2261–2268
Nuclear Cardiology: Guidance on the Implementation of SPECT Myocardial Perfusion Imaging. Vienna: INTERNATIONAL ATOMIC ENERGY AGENCY; 2016. https://www.iaea.org/publications/11076/nuclear-cardiology-guidance-on-the-implementation-of-spect-myocardial-perfusion-imaging.
Peix A, Cabrera LO, Padrón K, Rodríguez L, Fernández J, López G et al (2018) Association between non-perfusion parameters and presence of ischemia in gated-SPECT myocardial perfusion imaging studies. J Nucl Cardiol 25(2):609–615
Alama M, Labos C, Emery H, Iwanochko RM, Freeman M, Husain M et al (2018) Diagnostic and prognostic significance of transient ischemic dilation (TID) in myocardial perfusion imaging: a systematic review and meta-analysis. J Nucl Cardiol 25(3):724–737
Abidov A, Bax JJ, Hayes SW, Hachamovitch R, Cohen I, Gerlach J et al (2003) Transient ischemic dilation ratio of the left ventricle is a significant predictor of future cardiac events in patients with otherwise normal myocardial perfusion SPECT. J Am Coll Cardiol 42(10):1818–1825
Nakanishi R, Gransar H, Slomka P, Arsanjani R, Shalev A, Otaki Y et al (2016) Predictors of high-risk coronary artery disease in subjects with normal SPECT myocardial perfusion imaging. J Nucl Cardiol 23(3):530–541
Mandour Ali MA, Bourque JM, Allam AH, Beller GA, Watson DD (2011) The prevalence and predictive accuracy of quantitatively defined transient ischemic dilation of the left ventricle on otherwise normal SPECT myocardial perfusion imaging studies. J Nucl Cardiol 18(6):1036–1043
Halligan WT, Morris PB, Schoepf UJ, Mischen BT, Spearman JV, Spears JR et al (2014) Transient ischemic dilation of the left ventricle on SPECT: correlation with findings at coronary CT angiography. J Nucl Med 55(6):917–922
Brodov Y, Fish M, Rubeaux M, Otaki Y, Gransar H, Lemley M et al (2016) Quantitation of left ventricular ejection fraction reserve from early gated regadenoson stress Tc-99m high-efficiency SPECT. J Nucl Cardiol 23(6):1251–1261
Vachatimanont S, Sirisalipoch S, Chantadisai M (2022) Comparison of the diagnostic performance of myocardial perfusion scintigraphy with and without attenuation correction. Mol Imaging Radionucl Ther 31(2):130–138
Lomsky M, Johansson L, Gjertsson P, Björk J, Edenbrandt L (2008) Normal limits for left ventricular ejection fraction and volumes determined by gated single photon emission computed tomography–a comparison between two quantification methods. Clin Physiol Funct Imaging 28(3):169–173
Nakajima K, Matsumoto N, Kasai T, Matsuo S, Kiso K, Okuda K (2016) Normal values and standardization of parameters in nuclear cardiology: Japanese Society of Nuclear Medicine working group database. Ann Nucl Med 30(3):188–199
Moslehi M, Alidadi S, Assadollahi E, Assadi M (2015) Do ejection fraction and other gated stress rest myocardial perfusion parameters differ by age and gender? Nucl Med Rev Cent East Eur 18(1):7–12
Acknowledgments
The authors would like to acknowledge the staffs, including nuclear medicine physician, technologist, and nurses in the division of nuclear medicine, King Chulalongkorn Memorial Hospital for their support. The author also recognize Professor Stephen John Kerr for the statistical consultations.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SV. MC performed the initial analysis and discussion. SS supervised the project. The first draft of the manuscript was written by SV and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was by the Ethics Committee of Faculty of Medicine, Chulalongkorn University and the need for informed consent was waived by the Ethics Committee. (COA No. 611/2017, IRB No. 366/60).
Consent for publication
Not application. No data in the manuscript can be traced back, or used to identify individual person.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chantadisai, M., Sirisalipoch, S. & Vachatimanont, S. Utility of gated SPECT parameters in detection of coronary artery disease in patients with normal perfusion images. Egypt J Radiol Nucl Med 53, 257 (2022). https://doi.org/10.1186/s43055-022-00944-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00944-4