Abstract
Background
Objectives: To comparatively evaluate the role of ultrasound and MRI in rotator cuff and biceps tendon pathologies and to establish ultrasound as a consistently reproducible, quick and accurate primary investigation modality sufficient to triage patients requiring surgical correction of full thickness rotator cuff tears. Methods: Fifty patients, clinically suspected to have rotator cuff and/or biceps tendon pathologies, with no contraindications to MRI, were evaluated by US and MRI, in a prospective cross-sectional observational study. US was done with high-frequency linear probe, and MRI was done on a 1.5-T scanner using T1 oblique sagittal, proton density (PD)/T2 fat-suppressed (FS) oblique sagittal, T1 axial, PD/T2 FS axial, T1 oblique coronal, T2 oblique coronal and PD FS oblique coronal sequences. Statistical testing was conducted with the statistical package for the social science system version SPSS 17.0. The sensitivity, specificity, PPV, NPV and accuracy were also calculated to analyze the diagnostic accuracy of US findings correlating with MRI findings. A p value less than 0.05 was taken to indicate a significant difference.
Results
Mean age was 45 years; 74% patients were males; 77% females and 60% males had tears. Majority of patients with rotator cuff tears were in the sixth decade of life. The frequency of tears was higher among older patients. Fourteen percent of patients had full thickness tears while 64% had partial thickness tears. US was comparable to MRI for detection of full thickness tears with overall sensitivity, specificity, PPV and accuracy of 93.8%, 100%, 100% and 98.2%, respectively (p value < 0.001). For partial thickness tears, US had overall sensitivity, specificity, PPV and accuracy of 75.6%, 82.6%, 89.5% and 78%, respectively (p value < 0.001), as compared to MRI. Subacromial-subdeltoid bursal effusion and long head of biceps tendon sheath effusion were common associated, though, non-specific findings.
Conclusion
Ultrasound findings in our study were found to be in significant correlation with findings on MRI in detection of rotator cuff tears. US was equivalent to MRI in detection of full thickness tears and fairly accurate for partial thickness tears. Therefore, US should be considered as the first line of investigation for rotator cuff pathologies.
Similar content being viewed by others
Background
Rotator cuff and biceps tendon pathologies range from rotator cuff degeneration or tendinosis to partial thickness and full thickness tears [1, 2]. Both magnetic resonance imaging (MRI) and ultrasound (US) are indispensable tools of investigation for rotator cuff pathologies.
MRI provides good multiplanar delineation without the need of contrast and is free from radiation hazards. In addition to detailed information regarding rotator cuff defects, it also provides clinically significant information about adjacent structures, muscle atrophy, size of muscle cross-sectional area and fatty degeneration of muscles [3]. However, as compared with US, MRI is expensive and not as widely available. Ultrasound permits dynamic imaging. With recent advances, better probes and increasing experience, US has become the staple primary tool for evaluation that also serves well for follow up of rotator cuff pathologies [4, 5].
The variable utility of US in previous papers could be attributed to poor technique, lack of experience of ultrasonologist, inadequately defined ultrasound criteria and multiple observers. This inconsistency in accuracy in the published work has discouraged many from using shoulder ultrasound as a diagnostic tool for rotator cuff pathologies [6,7,8,9].
Shoulder ultrasound, if carried out by a single, trained, experienced radiologist using modern high-resolution equipment and standard diagnostic criteria is both sensitive and specific for the diagnosis of rotator cuff injuries, including partial thickness tears [10].
MR arthrography is not available at most centres and is an invasive process. We have compared the two most commonly ordered investigations. Moreover, our study aims at educating the smaller set-ups and clinicians that US can provide most answers at significantly lower costs.
Objective
This study aims to comparatively evaluate the role of ultrasound and MRI in various rotator cuff and biceps tendon pathologies with the objective to establish ultrasound as a consistently reproducible, quick and accurate primary investigation modality that is sufficient to triage patients requiring surgical correction of a full thickness tendon tear.
Methods
Fifty patients, who were clinically suspected to have rotator cuff and biceps tendon pathologies, were evaluated by US and MRI, in a prospective cross-sectional observational study by one observer studying only one modality in order to get independent interpretations for each modality. Patients with contraindications to MRI and those with surgical interventions on the shoulder joint were excluded. The patients were referred by an orthopaedist. Institutional review board approval was obtained, and each participant’s written informed consent was taken.
Ultrasound scanning was done using a linear high-frequency (5–12 Hz) probe by a single radiologist having more than 10 years of experience. The patients were made to sit on a revolving chair. The basic principles of musculoskeletal US were followed, i.e., each structure was examined in 2 planes and US scanning was done with beam perpendicular to tendon fibres. Evaluation was done as per the sequence: long head of biceps tendon (LHBT), subscapularis tendon, supraspinatus tendon (including test for im**ement), infraspinatus tendon, teres minor tendon, glenohumeral space and acromio-clavicular joint.
MRI was done on a 1.5-T MRI scanner using a dedicated shoulder coil. Planning of the study was done on axial view of the supraspinatus tendon. Imaging sequences included T1 oblique sagittal, proton density (PD)/T2 fat-suppressed (FS) oblique sagittal, T1 axial, PD/T2 FS axial, T1 oblique coronal, T2 oblique coronal and PD FS oblique coronal. Oblique coronal images were acquired with sections parallel to the supraspinatus tendon and oblique sagittal with sections perpendicular to the supraspinatus tendon. The images were read by a different radiologist having experience of more than 10 years.
The diagnostic criteria for US and MRI are summarized in Table 1.
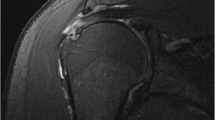
Tendinosis vs partial tear: US image (a) of a patient showing bulky and heterogeneous supraspinatus tendon with mixed hypo- and hyperechoic areas. Corresponding MRI PDFS image (c) shows increase in signal intensity while T2WI image (b) shows normal signal intensity, suggestive of tendinosis of supraspinatus tendon. US image (d) from another patient reveals an anechoic area on the articular side of supraspinatus tendon (arrowheads) with raised signal intensity on both PDFS (not shown) and T2WI (e) MRI images suggestive of articular sided partial thickness tear
Statistical testing was conducted with the statistical package for the social science system version SPSS 17.0. Categorical variables were expressed as frequencies and percentages. Nominal categorical data between the groups were compared using chi-squared test or Fisher’s exact test as appropriate. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were also calculated to analyze the diagnostic accuracy of US findings correlating with MRI findings. For all statistical tests, a p value less than 0.05 was taken to indicate a significant difference.
Results
Demographic data and imaging findings are detailed in Table 2. Majority of patients with combined rotator cuff tears were in the sixth decade of life. Sixty-four percent of patients had partial thickness tears, and 14% patients had full thickness tears. All full thickness tears involving LHBT, subscapularis tendon and supraspinatus tendon were correctly demonstrated on US. The sensitivity and accuracy of US for partial thickness tears for LHBT (6 cases) were 50% and 93.6%, respectively. The sensitivity, specificity, PPV, NPV and accuracy of US in detection of partial thickness tears of the subscapularis tendon (12 cases) were 75%, 94.7%, 82%, 92.3% and 90%, respectively.
US had sensitivity, specificity and accuracy of 91%, 93% and 92%, respectively, for partial thickness tears (22 cases) of supraspinatus tendon and 82.6%, 96.3% and 90% for tendinosis (23 cases) of supraspinatus tendon.
For full thickness tears of infraspinatus tendon (7 cases), US had a sensitivity, specificity and accuracy of 85.7%, 100% and 98%, respectively. For partial thickness tears (5 cases), US had a sensitivity, specificity and accuracy of 60%, 100% and 96%, respectively.
There were no cases of teres minor tendon pathologies in our study.
US was comparable to MRI for detection of full thickness tears with overall sensitivity, specificity, PPV and accuracy of 93.8%, 100%, 100% and 98.2%, respectively (p value < 0.001). For partial thickness tears, it had overall sensitivity, specificity, PPV and accuracy of 75.6%, 82.6%, 89.5% and 78%, respectively (p value < 0.001) as compared to MRI.
There were a total of 61 tears, including both partial and full thickness tears. The sensitivity, specificity, PPV, NPV and accuracy of US for detection of any tear were 80.3%, 93.8%, 92.4%, 83.5% and 87.3%, respectively (p value < 0.001).
The most common finding associated with tendon tears was subacromial-subdeltoid (SA-SD) bursal effusion which was present in 82% (41/50) of the patients. Of these, 58% patients had a rotator cuff tear. The sensitivity, specificity, positive predictive value (PPV) and accuracy of SA-SD bursal effusion for diagnosing rotator cuff tear were 90%, 33%, 71% and 70%, respectively. The association was not statistically significant (p value = 0.056). Biceps tendon sheath effusion was seen in 28 out of 50 patients (56%). Of these, 68% patients had a rotator cuff tear. The sensitivity, specificity, positive predictive value (PPV) and accuracy of biceps tendon sheath effusions for diagnosing rotator cuff tear were 60%, 50%, 68% and 56%, respectively. The association was not statistically significant (p value = 0.522).
Discussion
Mean age of patients was 45 years (range: 13–75 years). Seventy-four percent were males; 77% females and 60% males had tears. Majority of patients with combined rotator cuff tears were in the sixth decade of life. The frequency of tears was higher among older patients. Fourteen percent of the patients had full thickness tears, and 64% had partial thickness tears.
There was a single case of full thickness tear of the long head of biceps tendon (LHBT). It was correctly diagnosed by both US and MRI. The sensitivity and accuracy of US for partial thickness tears of LHBT were 50% and 93.6%, respectively. Medial dislocation of the tendon (two cases) was correctly diagnosed by US (Fig. 3c, d).
Biceps pulley, the intraarticular portion formed by coracohumeral and superior glenohumeral ligaments, is poorly visualized by US and even MRI. Only magnetic resonance arthrography (MRA) is able to directly identify pulley and its lesions [17].
All subscapularis full thickness tears were correctly identified on US. The sensitivity, specificity, PPV, NPV and accuracy of US in detection of partial thickness tears of the subscapularis tendon were 75%, 94.4%, 82%, 92.3% and 89.6%, respectively. Narsimhan et al. [18] also reported high specificity of 93.1% for detection of subscapularis tears with overall accuracy, PPV and NPV of 75.8%, 73.1% and 76.4%, respectively. Sensitivity of ultrasound was low (42.8%) for smaller tears and higher (79%) for larger tears [18].
All full thickness supraspinatus tendon tears were correctly demonstrated on US. Sensitivity, specificity and accuracy of US for partial thickness tears were 91%, 93% and 92%, respectively, and 82.6%, 96.3% and 90%, respectively for tendinosis. Abd-ElGawad et al. [19] reported US sensitivity, specificity and accuracy of 92.3%, 92.6% and 92.5%, respectively, for diagnosing partial thickness tears (PTT) and 92.6%, 94% and 95% for diagnosing full thickness tears (FTT).
There were seven cases of full thickness tears of the infraspinatus tendon on MRI. US was able to correctly diagnose six tears, with sensitivity, specificity and accuracy of 85.7%, 100% and 98%, respectively. Sensitivity, specificity and accuracy of US were 60%, 100% and 96%, respectively, for partial tears.
There were no cases of teres minor tendon pathologies seen in any of the patients examined.
There were two cases of calcific tendinitis in our study affecting supraspinatus and subscapularis tendons (Fig. 4a–c). On US, calcifications appear as hyperechoic foci with or without posterior acoustic shadowing. In case of shoulder, type I calcific tendinitis shows posterior acoustic shadowing while type II calcific tendinitis shows mild shadowing and type III shows no posterior acoustic shadowing. Conventional MRI has poor sensitivity in detection of calcific tendinitis because of lesser amounts of resonating protons contained within calcific deposits. Moreover, when the calcification is edematous, signal changes may occur mimicking a tear. In our study, the deposits were clearly demonstrated on US and were inconspicuous on conventional MRI.
Acromio-clavicular joint degeneration (Fig. 4d, e) was seen in 64% (32/50) patients, with mild degeneration in 47% (15/32), moderate in 28% (9/32) and severe in 25% (8/32) of these patients. US could not detect 3 out of 15 patients of mild degeneration. All cases of moderate and severe degeneration were correctly diagnosed on US. Overall for detection of acromio-clavicular joint degeneration, US had sensitivity, specificity and accuracy of 90%, 100% and 93%, respectively. Another important associated finding that came to light on data analysis was that 84% (27/32) of patients with a rotator cuff tear had acromio-clavicular degeneration. The association was found to be statistically significant (p value < 0.001) as shown in Table 3. According to Ban et al. [20], 92% cases with acromio-clavicular joint changes showed tear/tendinosis of supraspinatus tendon.
Farley et al. [13] concluded that interruption of tendon continuity was the most specific MR finding associated with full thickness rotator cuff tears and subacromial fluid was the most common finding associated with rotator cuff tears. According to our study, interruption of tendon continuity (major criterion) was found to be present in all cases of full thickness tears.
Arslan et al. [21] did not find a statistically significant association between rotator cuff tears and effusions in the biceps tendon sheath, SA-SD bursa or both and concluded that sonographic detection of isolated intraarticular fluid, SA-SD bursal fluid or both had a low sensitivity and PPV in the diagnosis of rotator cuff tears. Our study concurs with this study. SA-SD bursal fluid and biceps tendon sheath effusion were common associated findings, however did not show statistical significance with tears (p value > 0.05).
Rutten et al. [22] concluded that US had sensitivity and accuracy of 95% and 94%, respectively, for detection of full thickness tears and 89% and 81%, respectively for partial tears.
Roy et al. [23] noted that diagnostic accuracy of US, MRI and MR arthrogram in the characterization of full thickness RC tears was high with overall estimates of sensitivity and specificity over 90%. As for partial RC tears and tendinopathy, overall estimates of specificity were also high (> 90%), while sensitivity was lower (67–83%). When considering accuracy, cost, and safety, they concluded that US was the best option.
Naqvi et al. [24] found sensitivity, PPV, NPV and accuracy of 88%, 88%, 89% and 89%, respectively, for US as compared to MRI, for detection of full-thickness tears.
According to Mohtasib [25], overall PPV, NPV, sensitivity, specificity and accuracy of US for the detection of full thickness tears were 35%, 97%, 78%, 83% and 83%, respectively, as compared with MRI. For partial thickness tears, the overall PPV, NPV, sensitivity, specificity and accuracy of US compared with MRI were 51%, 60%, 51%, 60% and 56%, respectively.
We found US to be a fairly good modality to detect partial thickness tears with an overall sensitivity, specificity, PPV and accuracy of 75.6%, 82.6%, 89.5% and 78%, respectively (p value < 0.001), as compared to MRI. US is an excellent modality for detection of full thickness tears with an overall sensitivity, specificity, PPV and accuracy of 93.8%, 100%, 100% and 98.2%, respectively, (p value < 0.001).
There were a total number of 61 tears, including both partial and full thickness tears. US could correctly identify 49 of these. The sensitivity, specificity, PPV, NPV and accuracy of US for detection of any tear were found to be 80.3%, 93.8%, 92.4%, 83.5% and 87.3%, respectively (49 true positives, 61 true negatives, 4 false positives and 12 false negatives).
Few potential pitfalls of US are misinterpretation of the rotator interval as a tear, difficulty in visualization of longitudinal tears that may not be associated with typical signs, anisotropy, limited ability to assess labral pathologies, operator dependence and lack of uniformity because of the dynamic nature of musculoskeletal examinations. The mobile nature of joints, in combination with random probe placements, gives rise to unlimited permutations in image variations. Thus, for accurate interpretation of the findings, there is a learning curve [26].
US has several advantages. It is cheaper, portable and highly accessible modality. Further, it allows side-to-side comparisons with ease. The disadvantages and limitations of US are easily overcome. A disadvantage stated above which stems from mobile nature of joints has been utilized as one of the major advantages as this very mobile nature permits dynamic maneuvers in real time for subcoracoid and subacromial im**ement studies (as shown in Fig. 2d–f).
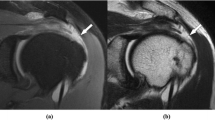
US images (a–c) showing spectra of partial thickness tears. a Interstitial partial tear of LHBT. b Interstitial tear of supraspinatus tendon. c Interstitial tear of subscapularis tendon with corresponding changes in MRI images (not shown). d–f Acromial spur with subacromial im**ement. d An acromial spur and supraspinatus fibres (asterisk) with shoulder in adducted position. In the abducted position (e), acromial spur is seen preventing smooth gliding of supraspinatus fibres underneath the acromion process resulting in buckling of supraspinatus fibres (acromial spur—outlined in white). T1W sagittal MRI images (f) showing an acromial spur (outlined in white) with type III acromion morphology and reduced acromio-humeral distance
Complete rotator cuff tear with medially displaced long head of biceps tendon: US images (a) and corresponding sagittal PDFS MRI image (b) of a patient showing non-visualization of rotator cuff tendons in the form of anechoic space (asterisk) in the expected locations of these tendons with associated herniation of the overlying deltoid muscle. This indicates a full thickness tear of rotator cuff. US images in the same patient show non-visualization of LHBT in the bicipital grove (thick white arrow in c) which is seen lying medially and inferiorly (arrowhead in c). Corresponding axial PDFS MRI image (d) shows empty bicipital grove with medially displaced LHBT with full thickness tear and retraction of subscapularis tendon
Radiograph of the shoulder (a) shows multiple foci of calcification in the region of supraspinatus tendon. US image (b) of the same patient shows multiple calcific foci in supraspinatus tendon casting posterior acoustic shadowing. MRI PDFS axial image (c) shows tiny hypointense foci at the bursal surface (multiple small arrows) suggestive of calcific tendinosis. Sagittal PDFS MRI image (d) and US image (e) showing acromio-clavicular degeneration with multiple bony irregularities (small arrows in e) and deformed acromio-clavicular joint with hyperintense signal intensity (d)
In experienced hands, with proper utilization of knowledge of normal anatomy and pitfalls, rotator cuff sonography is an adjunct diagnostic and a primary screening tool that provides valuable extension to patient’s physical examination, the non-invasive gold standard being the MR imaging. This is in accordance with the latest ESSR guidelines, according to which US is first choice technique for full thickness tears, bursitis, calcific tendinitis, LHBT rupture and dislocation and equivalent to MRI for partial tears and LHBT tendinosis [27].
We believe that our study differs from many others that precede this, in that we have directly compared US with MRI, the two modalities that are most frequently ordered investigations for rotator cuff pathologies. MR arthrography is not available at most centres. Further, we had a well-equipped team of trained and experienced musculoskeletal radiologists with proficient technological support in the form of trained technologists, a dedicated shoulder coil for MR imaging and modern equipment with a linear high-frequency probe for ultrasound examination.
Number of cases that underwent surgery and arthroscopy was less, thereby not allowing us comparison with surgical/arthroscopic findings. In our study, only 4 patients underwent surgery/arthroscopy, so we considered MRI as the non-invasive gold standard investigation of choice and compared our ultrasound findings with MRI.
MR arthrography (MRA) is considered the gold standard imaging modality; however, issues such as its invasive nature, use of ionizing radiation during fluoroscopy and contrast-related adverse reactions are associated with it. Also, it is not available at most centres. Hence, the benefits from MRA should be weighed against its risks, and it is not appropriate to perform such an investigation when patients have no serious symptoms. Moreover, in most cases, clinical examination combined with MRI are sufficient for the diagnosis. In patients with acute or severe tears, MRI provides intrinsic contrast in the form of effusions or soft tissue changes without the need of external contrast agents. MRA is more appropriate for chronic tears or subtle abnormalities. For full thickness tears, MRA may not be necessary at all in most cases. There may be certain situations like postoperative re-tear of the rotator cuff or distinguishing very small complete tears from partial thickness rotator cuff tears where MRA is required [28].
For overall analysis of partial thickness tears, MRA obviously has higher sensitivity and specificity compared with conventional MRI. Owing to lack of contrast agents and joint distension on conventional MRI, small partial tears may be misdiagnosed as tendinosis, and large ones as full thickness tears [29]. However, for bursal-sided partial thickness tears, MRI has a similar sensitivity as MRA [30]. Considering all these points, MRA is not required as the initial examination because of its invasiveness and inconvenience.
The sample size could be considered as a limiting factor for calculation of statistics of individual tendons and some of the perfect values may be attributed to this factor.
Conclusion
Ultrasound findings in our study showed significant correlation with MRI findings in detection of full thickness tears with high sensitivity and specificity. We suggest the use of US scan as a primary imaging modality that is sufficient to triage patients who require surgical correction of a full thickness rotator cuff tear.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- MRA:
-
Magnetic resonance arthrography
- US:
-
Ultrasound
- LHBT:
-
Long head of biceps tendon
- PD:
-
Proton density
- RC:
-
Rotator cuff
- FS:
-
Fat suppressed
- SA-SD bursa:
-
Subacromial-subdeltoid bursa
- PPV/NPV:
-
Positive predictive value/ Negative predictive value
- FTT/PTT:
-
Full thickness tear/partial thickness tear
References
Neer CS 2nd. (1972) Anterior acromioplasty for the chronic im**ement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 54(1):41–50. https://doi.org/10.2106/00004623-197254010-00003
Neer CS 2nd (1983) Im**ement lesions. Clin Orthop Relat Res 173:70–77
Morag Y, Jacobson JA, Miller B, Maeseneer M, Girish G, Jamadar D (2006) MR imaging of rotator cuff injury: what the clinician needs to know. RadioGraphics 26(4):1045–1065
Saraya S, Bakry RE (2016) Ultrasound: can it replace MRI in the evaluation of the rotator cuff tears? Egypt J Radiol Nuclear Med 47(1):193–201. https://doi.org/10.1016/j.ejrnm.2015.11.010
Rutten MJCM, Jager GJ, Blickman JG (2006) US of the rotator cuff: pitfalls, limitations, and artifacts. Radiographics 26(2):589–604. https://doi.org/10.1148/rg.262045719
Martin-Hervas C, Romero J, Navas-Acien A, Reboiras JJ, Munuera L (2001) Ultrasonographic and magnetic resonance images of rotator cuff lesions compared with arthroscopy or open surgery findings. J Shoulder Elbow Surg. 10(5):410–415. https://doi.org/10.1067/mse.2001.116515
Van Holsbeeck MT, Kolowich PA, Eyler WR et al (1995) US depiction of partial-thickness tear of the rotator cuff. Radiology. 197(2):443–446. https://doi.org/10.1148/radiology.197.2.7480690
Read JW, Perko M (1998) Shoulder ultrasound: diagnostic accuracy for im**ement syndrome, rotator cuff tear, and biceps tendon pathology. J Shoulder Elbow Surg. 7(3):264–271. https://doi.org/10.1016/S1058-2746(98)90055-6
Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K (2000) Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in 100 consecutive cases. J Bone Joint Surg Am. 82(4):498–504. https://doi.org/10.2106/00004623-200004000-00005
Cullen DM, Breidahl WH, Janes GC (2007) Diagnostic accuracy of shoulder ultrasound performed by a single operator. Australas Radiol. 51(3):226–229. https://doi.org/10.1111/j.1440-1673.2007.01685.x
Fischer CA, Weber MA, Neubecker C, Bruckner T, Tanner M, Zeifang F (2015) Ultrasound vs. MRI in the assessment of rotator cuff structure prior to shoulder arthroplasty. J Orthop. 12(1):23–30. https://doi.org/10.1016/j.jor.2015.01.003
Stoller DW (2007) Magnetic resonance imaging in orthopaedics and sports medicine, 3rd edn. Lippincott Williams & Wilkins, Philadelphia, pp 1131–1462
Farley TE, Neumann CH, Steinbach LS, Jahnke AJ, Petersen SS (1992) Full-thickness tears of the rotator cuff of the shoulder: diagnosis with MR imaging. Am J Roentgenol 158(2):347–351. https://doi.org/10.2214/ajr.158.2.1729796
Bianchi S, Martinoli C (2007) Ultrasound of the musculoskeletal system. Springer, Berlin, pp 189–331
Stein BES, Wiater JM, Pfaff HC, Bigliani LU, Levine WN (2001) Detection of acromioclavicular joint pathology in asymptomatic shoulders with magnetic resonance imaging. J Shoulder Elbow Surg. 10(3):204–208. https://doi.org/10.1067/mse.2001.113498
Chianca V, Albano D, Messina C et al (2018) Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta Biomed 89(1-S):186–196
Zappia M, Chianca V, Pietto DF, Reginelli A, Natella R, Maggialetti N et al (2019) Imaging of long head biceps tendon: a multimodality pictorial essay. Acta bio-medica: Atenei Parmensis 90(5-S):84–94
Narasimhan R, Shamse K, Nash C, Dhingra D, Kennedy S (2015) Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop. https://doi.org/10.1007/s00264-015-3043-9 (Epub ahead of print)
Abd-ElGawad EA, Ibraheem MA, Fouly EH (2013) Evaluation of supraspinatus muscle tears by ultrasonography and magnetic resonance imaging in comparison with surgical findings. Egypt J Radiol Nucl Med. 44(4):829–834. https://doi.org/10.1016/j.ejrnm.2013.08.001
Ban AA, Makada MT, Bahri NU (2019) Correlation of supraspinatus tears and tendinosis with acromion morphology and acromioclavicular arthritis based on conventional MRI and CT. J Med Sci Clin Res 07(06):106–115
Arslan G, Apaydin A, Kabaalioglu A, Sindel T, Lüleci E (1999) Sonographically detected subacromial/subdeltoid bursal effusion and biceps tendon sheath fluid: reliable signs of rotator cuff tear. J Clin Ultrasound. 27(6):335–339. https://doi.org/10.1002/(SICI)1097-0096(199907/08)27:6<335::AID-JCU4>3.0.CO;2-0
Rutten MJCM, Spaargaren GJ, van Loon T, de Waal Malefijt MC, Kiemeney LALM, Jager GJ (2010) Detection of rotator cuff tears: the value of MRI following ultrasound. Eur Radiol. 20(2):450–457. https://doi.org/10.1007/s00330-009-1561-9
Roy JS, Braën C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, Bureau NJ, Fremont P (2015) Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 49(20):1316–1328. https://doi.org/10.1136/bjsports-2014-094148
Naqvi GA, Jadaan M, Harrington P (2009) Accuracy of ultrasonography and magnetic resonance imaging for detection of full thickness rotator cuff tears. Int J Shoulder Surg. 3(4):94–97. https://doi.org/10.4103/0973-6042.63218
Mohtasib RS, Alzahrani AM, Asiri YN, Rayes ZF, Alshaalan MA (2019) Accuracy of shoulder ultrasound examination for diagnosis of rotator cuff pathologies: a single-center retrospective study. Ann Saudi Med. 39(3):162–171. https://doi.org/10.5144/0256-4947.2019.162
Lew HL, Chen CPC, Wang TG, Chew KTL (2007) Introduction to musculoskeletal diagnostic ultrasound: examination of the upper limb. Am J Phys Med Rehabil. 86(4):310–321. https://doi.org/10.1097/PHM.0b013e31803839ac
Sconfienza LM, Albano D, Allen G, Bazzocchi A, Bignotti B, Chianca V, Facal de Castro F, Drakonaki EE, Gallardo E, Gielen J, Klauser AS, Martinoli C, Mauri G, McNally E, Messina C, Mirón Mombiela R, Orlandi D, Plagou A, Posadzy M, de la Puente R, Reijnierse M, Rossi F, Rutkauskas S, Snoj Z, Vucetic J, Wilson D, Tagliafico AS (2018) Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur Radiol. 28(12):5338–5351. https://doi.org/10.1007/s00330-018-5474-3
Liu F, Cheng X, Dong J, Zhou D, Han S, Yang Y (2020) Comparison of MRI and MRA for the diagnosis of rotator cuff tears: a meta-analysis. Medicine. 99(12):e19579. https://doi.org/10.1097/MD.0000000000019579
Wright T, Yoon C, Schmit BP (2001) Shoulder MRI refinements: differentiation of rotator cuff tear from artifacts and tendonosis, and reassessment of normal findings. Semin Ultrasound CT MR 22(4):383–395. https://doi.org/10.1016/S0887-2171(01)90028-9
Suh K, Kim Y, Lee S et al (1996) Glenohumeral MR arthrography with intravenously administered Gd-DPTA: evaluation of clinical utility and effect of exercise time and amount of contrast medium. Radiology 201:160
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
AA did the conception, design and analysis; interpreted the data and drafted the work. VK drafted and supervised the work. BA did the conception, design and analysis. VK supervised the work. CS helped with interpretation. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Ethics Committee of Diwan Chand Satyapal Aggarwal Imaging Research Centre. Reference number is not available. The modalities used were ultrasound and MRI which do not entail any ionic radiations. MRI was done without contrast. Patients were screened for any contraindications for MRI. This was not a clinical trial. The patients selected were referred from clinicians for symptoms related to shoulder joint and underwent ultrasound and MRI. These cases were included in study. Written and informed consent was obtained from patients. No personal information has been used in the dataset. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies on animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agarwal, A., Vani, K., Batta, A. et al. Can ultrasound suffice for triaging patients requiring surgical correction of rotator cuff tears—a comparative evaluation of ultrasound and magnetic resonance imaging. Egypt J Radiol Nucl Med 52, 119 (2021). https://doi.org/10.1186/s43055-021-00477-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-021-00477-2