Abstract
Background
The infection caused by the SARS-CoV-2 virus has led to the emergence of a novel diagnostic entity known as “post-COVID syndrome” (PCS). It is characterized by a constellation of medical and psychiatric symptoms that occur and persist for variable duration following the COVID infection. Among these post-COVID psychiatric symptoms are depressive and anxiety disorders, which were found to be the highest prevalence in the post-COVID period. The frequency and severity of post-COVID symptoms are correlated with the severity of the infection. Many inflammatory and coagulation markers have been involved in the severity of post-COVID symptoms and hence the development of post-COVID psychiatric symptoms/disorders. Limited research has been conducted to examine the psychological challenges experienced by individuals in the early stages of post-COVID recovery in Egypt, specifically within a timeframe of 1 to 3 months. The current study aims to estimate the occurrence rate of early post-COVID psychiatric symptoms/disorders such as depression and anxiety and to detect its association with clinical and severity parameters of COVID-19 infection.
Methods
The current study was a comparative cross-sectional approach, from the chest department’s “post-COVID-19 follow-up” outpatient clinic at Kobri ElKoba Medical Complex in Cairo, Egypt. A convenient sample of adult Egyptian patients were recruited between October 2021 and June 2022. They were subjected to the following: a pre-designed questionnaire to collect the patients’ demographic characteristics, Arabic version of General Health Questionnaire (GHQ) to identify potential cases, Arabic version of Structured Clinical Interview for DSM-IV (SCID I) Clinician Version (SCID-CV) and retrieval of essential related clinical and laboratory data like C-reactive protein (CRP), systemic immune-inflammation index (SII): (neutrophils × platelets)/lymphocytes), neutrophil/lymphocyte ratio (NLR) and platelet/lymphocyte ratio (PLR), and D-dimer and COVID-19 treatment lines together with a liker scale questionnaire to assess the severity of COVID-19 infection.
Results
Depression was found to be the most prevalent psychiatric disorder (45.6%) among the study participants, followed by generalized anxiety disorder (42.1%). Subthreshold GAD and depression were found in 17.5% and 14% of patients respectively. COVID was a major predictor of GAD (p 0.000), while being on antibiotics (p = 0.033), having cardiac illnesses (p = 0.007), and an increased D dimer (p = 0.022) were the most predictive factors for depression.
Conclusion
COVID-19 infection has demonstrated an increased risk of mental health problems in multiple domains. It was evident that depression was the most presenting psychiatric illness among the studied sample (45.6%), while generalized anxiety disorder was the second most prevalent disorder (42.1%). And suicide was found in 9.6% of the study sample. It is worth noting that our results displayed a high prevalence of subthreshold psychiatric symptoms. These findings emphasize the utmost need for mental health assessments for all survivors.
Similar content being viewed by others
Introduction
In the context of a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, the post coronavirus disease of 2019 (COVID-19) illness is widely acknowledged as a major clinical consequence [1]. The notion of “infection plus” has lately been used to characterize the consequential outcomes of infectious pandemics such as COVID-19, as their psychological and cognitive impacts typically surpass their medical influences [2].
Extensive scholarly literature indicates that the prevalence of post-COVID-19 syndrome varies between 10 and 35%. Nevertheless, it is worth noting that rates as high as 85% have been observed among individuals who had been previously hospitalized [1]. Despite ongoing debate, recent suggestions have proposed diagnostic criteria and a classification system for post-COVID-19 syndrome. This new clinical entity can be categorized into three groups: (a) subacute syndrome or ongoing symptomatic COVID-19, characterized by symptoms and abnormalities persisting from 4 to 12 weeks after acute COVID-19; (b) chronic or long post-COVID-19 syndrome, which encompasses symptoms and issues that persist or emerge after 12 to 24 weeks following the onset of acute COVID-19; and (c) persistent post-COVID symptoms, referring to symptoms that continue for more than 24 weeks and cannot be attributed to any other diagnoses [3, 4].
The current recommendation by the World Health Organization (WHO) is to refer to the condition as “post-COVID-19 condition,” as this terminology avoids assigning causality or specifying the duration [5]. In recent times, the International Classification of Diseases, 10th edition (U09) and the International Classification of Diseases, 11th edition (RA02) have introduced distinct codes [6, 7] for the purpose of identification. The condition known as “Post COVID-19 condition” has been officially recognized by the International Classification of Diseases, 11th edition. It manifests in individuals who have an established record of probable or confirmed infection with the SARS CoV-2 virus. Typically, this condition arises approximately 3 months after the initial onset of COVID-19 symptoms and persists for a minimum of 2 months. Importantly, the symptoms experienced by these individuals cannot be attributed to any other diagnosable condition. Symptoms may manifest either as a fresh beginning subsequent to the initial recuperation from an acute episode of COVID-19 or as a continuation of the initial disease. Symptoms may exhibit variability, mutability, or recurrence over time.
Frequently observed are enduring medical manifestations subsequent to the first onset of COVID-19, which commonly encompass symptoms such as weariness, difficulty breathing, thoracic discomfort, and persistent coughing [4]. Multiple studies have indicated that there is a notable prevalence of sleep and psychiatric issues during the COVID-19 pandemic, with roughly 26 to 40% of individuals experiencing such problems persisting for up to 6 months after their initial infection. The symptoms associated with this condition encompass a range of manifestations, such as obsessions and compulsions, diminished engagement in social interactions, impaired capacity to pay attention, displays of aggression, heightened irritability, substance abuse, cognitive impairments, and the development of post-traumatic stress disorder [8,9,10,11]. The enduring nature of these symptoms has a substantial impact on the quality of life experienced by patients and contributes to an increased level of required care [12, 13].
An etiology of post-COVID-19 syndrome remains predominantly elusive. The pathophysiology of the condition has been hypothesized to involve multiple interacting pathways. The pathogenesis of post-COVID-19 syndrome involves several factors, including prolonged inflammatory and immune reactions characterized by elevated levels of interferon-γ and interleukin-2, and 6 [14, 15]. Additionally, virus-driven tissue damage [16, 17], alterations in the microbiome [18], and the occurrence of a multisystem inflammatory syndrome in adults (MIS-A) [19] have all been identified and associated with this condition.
Additional pathogenic pathways implicated in post-COVID-19 syndrome encompass immune-mediated vascular dysfunction and thromboembolism [20]. Elevated levels of D-dimer have been seen in severe cases of COVID-19, which are often accompanied by microangiopathy and a state of hypercoagulability. Multiple investigations have documented a correlation between elevated baseline D-dimer levels and the occurrence of depression and cognitive deterioration during the post-COVID-19 phase [21]. Multiple studies have revealed several sociodemographic and clinical risk factors associated with the development of PCS. For instance, gender disparities have been seen, with a higher prevalence of PCS in females compared to males. Furthermore, it has been found that women have a more pronounced specific T-cell response to the SARS-CoV-19 virus, which may contribute to their increased susceptibility to PCS [22]. Furthermore, it appears that middle-aged adults are more susceptible to its effects compared to elderly individuals [5].
Furthermore, additional literature has demonstrated that the psychological symptoms observed are not solely confined to the post-COVID-19 period. Instead, the intensity of these symptoms is influenced by the severity of the inflammatory response experienced during the initial illness, thereby exerting a substantial influence on the overall quality of life for affected individuals. The topic of discussion pertains to the COVID-19 pandemic. However, the existing evidence on fundamental inflammatory biomarkers in post-COVID-19 syndrome is very limited, lacking proper organization, and exhibits conflicting findings [18]. To date, numerous methodological shortcomings have been identified in the existing body of literature pertaining to post-COVID-19 psychiatric sequelae. These limitations include the absence of a standardized assessment of SARS-CoV-2 infection [23] and the failure to assess severity markers [24]. Moreover, a significant proportion of these investigations focused on a limited range of neuropsychiatric symptoms when examining the presence of psychiatric symptoms or disorders following COVID-19 [25]. The primary method employed for evaluating psychiatric symptoms was the utilization of self-report questionnaires [26]. Additionally, data collection often relied on electronic databases [27] or the subjective clinical judgement of attending physicians [28]. Consequently, the assessment of psychiatric symptoms in these studies was constrained to dimensional or non-validated symptom scales, rather than employing structured clinical objectives and validated interview psychometric scales [4, 29, 30].
Eventually, it is worth noting that a significant proportion of the studies included in this analysis were carried out on samples from Eastern and European nations. This particular characteristic of the research participants may potentially restrict the extent to which the findings can be applied to other populations or circumstances [4].
Given the concerning implications of COVID-19 infection on mental well-being, the growing recognition of inflammation’s significance in the field of psychiatry, and the current evidence linking the severity of inflammation to more severe manifestations of mental health disorders [31, 32], it is advisable to assess the psychopathology of individuals recovering from COVID-19 and expand investigations into inflammatory biomarkers. This approach aims to facilitate early identification and intervention.
To the best of our current understanding, with the exception of a solitary study conducted in Egypt that examined the cognitive consequences experienced by individuals who have recovered from COVID-19 [33], there is a dearth of Egyptian research exploring the occurrence of psychological and psychiatric impairments following COVID-19, as well as their potential connection to inflammatory and coagulation markers.
The research team was motivated to undertake this study in order to assess the prevalence of psychological symptoms and disorders during the early post-COVID-19 period (1–3 months). Additionally, they aimed to identify the underlying inflammatory, coagulation, and clinical factors associated with the psychological symptoms related to COVID-19, as well as predict potential variables linked to a higher risk of psychiatric morbidity. The research team placed significant emphasis on evaluating patients through the utilization of a thorough protocol consisting of psychometric tools that have been objectively validated and established [34].
Methods
Study design and setting
This study employed a comparative cross-sectional approach. From the chest department’s “post-COVID-19 follow-up” outpatient clinic at Kobri ElKoba Medical Complex in Cairo, Egypt, we were able to collect a convenient sample of adult Egyptian patients. Using Epi Info 6.0, we determined that a sample size of 140 people would provide 80% power at the 95% confidence level. A face-to-face interview was conducted utilizing the research assessment instruments between October 2021 and June 2022, taking into account maintaining at least 1 m of physical distance and wearing personal protective materials such as face masks.
Participants
The study included all COVID-19 patients presented to the “post-COVID-19 follow-up” outpatient clinic of the chest department at Kobri ElKoba Medical Complex in Cairo, Egypt, in the period from December 2021 to May 2022, which coincided with the 3rd wave of COVID-19 in Egypt.
The COVID-19 diagnosis was confirmed by a positive polymerase chain reaction test, and we included only cases who recovered for at least 1 to 3 months after either home isolation for those with mild symptoms or hospital treatment, with confirmation of stabilization of their general medical condition. Individuals with a history of a psychiatric disorder, a neurological condition, an intellectual disability, or dementia were excluded, as were patients taking psychotropic drugs. Moreover, patients who were younger than 18 years or older than 65 years, refused to participate, or refused to sign a written consent form were excluded from the study. According to the Egyptian Ministry of Health regulations, all patients with suspected COVID-19 infection were subjected to certain laboratory and radiological investigations, which included CBC, CRP, ferritin, nasopharyngeal swab D-dimer, and chest CT with clinical examination.
The study tools
All participants were subjected to the following:
-
A-
A pre-designed questionnaire to collect the patients’ sociodemographic characteristics (age, gender, education, and cigarette smoking) and clinical characteristics (self-reported comorbidities, symptom onset time).
-
B-
Psychometric tests
-
1.
General Health Questionnaire (GHQ) [15] (Arabic version) [16]: A self-administered, 28-item general health questionnaire. It was used to identify potential cases, which could then be verified, and the nature of which could be determined by using a second-stage instrument, as it should not be used as a sole criterion for diagnosis.
-
2.
Structured Clinical Interview for DSM-IV (SCID I) [18] Arabic Version [19]: Structured Clinical Interview for DSM-IV-Clinician Version (SCID-CV) [18] Arabic version [19]. It contains seven diagnostic modules and focused on different diagnostic groups: mood, psychotic, substance abuse, anxiety, somatoform, eating, and adjustment disorders. It was validated through its use in numerous studies conducted at research centers in Egypt. We used the clinical version for a relatively easier administration in a clinical setting.
-
1.
-
C-
Retrieval of the clinical data: A set of clinical data relative to the acute stage of the disease was retrieved from hospital charts and databases, providing baseline information on the duration of the hospital stay, COVID severity (requirement/duration of ICU care, requirement of orotracheal intubation, mechanical ventilation, or dialysis), and any available information about previous diagnoses, smoking, comorbidities, and relevant clinical symptoms.
-
D-
Clinical data on disease severity: It was measured using a Likert scale of 1 to 6 severity index as follows: 1, not admitted to hospital with resumption of normal activities; 2, not admitted to hospital but unable to resume normal activities; 3, admitted to hospital but not requiring supplemental oxygen; 4, admitted to hospital but requiring supplemental oxygen; 5, admitted to hospital requiring high-flow nasal cannula (HFNC), noninvasive mechanical ventilation (NIV), or both; and 6, admitted to hospital requiring extracorporeal membrane oxygenation, invasive mechanical ventilation (IMV), or both. On the other hand, laboratory data was retrospectively collected from the hospital registry system, and it included the following:
-
1.
C-reactive protein (CRP): A cut-off level of more than 6 mg/L indicated a pathological rise.
-
2.
Systemic immune-inflammation index (SII): (neutrophils × platelets)/lymphocytes): A reference range of more than 390 × 109 cells/L was considered significant.
-
3.
Neutrophil/lymphocyte ratio (NLR) and platelet/lymphocyte ratio (PLR): The NLR cutoff was 3.0, and the cutoff for PLR was 115.3.
-
4.
D-dimer: A positive D-dimer was considered 0.50 or higher.
-
5.
COVID-19 treatment: (corticosteroids, intravenous immunoglobulin, antibiotics, thymosin, and antivirals including lopinavir–ritonavir, arbidol, chloroquine phosphate, and hydroxychloroquine).
-
1.
Study procedure
Subjects were assessed 1–3 months after resolution of COVID-19 symptoms through structured interviews and assessment protocols pertaining to an interdisciplinary medical team. First, sociodemographic data and clinical characteristics were collected using a designed questionnaire. Then study participants were subjected to the GHQ test for assessment of minor psychiatric morbidities. Those GHQ-positive participants were further evaluated for psychiatric morbidities using the SCID-1, which is a semi-structured diagnostic interview based on an efficient and comprehensive clinical evaluation (Fig. 1).
Evaluation of mental status was done in face-to-face interviews by a trained psychiatrist who attended five training sessions on the assessment protocol in order to standardize procedures and maximize the reliability of psychometric measures.
The assessment protocol required, on average, 45–60 min to be completed, comprising a structured interview with psychometric tests, as described below in the flowchart. Assessment for patients with SCID-I was done in a separate room at the post-COVID-19 outpatient clinic.
Statistical analysis
Recorded data were analyzed and tabulated using the Statistical Package for Social Sciences, version 23.0 (SPSS Inc., Chicago, IL, USA). The quantitative data were presented as mean ± standard deviation and ranges. Also, qualitative variables were presented as number and percentages. Data were explored for normality using Kolmogorov–Smirnov and Shapiro–Wilk test. Kruskal–Wallis test was used for multiple-group comparisons in nonparametric data, and Mann–Whitney U-test was used for two-group comparisons in nonparametric data. The comparison between groups with qualitative data was done by using chi-square test. Multivariate logistic regression analysis and odds ratios (OR) with 95% confidence intervals were computed to assess the overall association between each possible risk factors and the occurrence of each item of SCID. The confidence interval was set to 95%, and the margin of error accepted was set to 5%. So, the p-value was considered significant if < 0.05 and highly significant if < 0.001.
Results
Two-hundred and ninety-two patients (292) were eligible for the study. Non response was defined as fulfilling less than 80% of items in the questionnaires. Of all patients, 280 (95.9%) managed to complete the whole study assessment protocol, while only 12 patients were dropped out from the study, bringing the total non-response rate of the current study to 4.1%. The 12 non-response cases were excluded due to their inability to complete the assessment. Seven of them could not attend due to their work commitments, four of them due to medical complications, and one of them due to worsening of his psychiatric symptoms that necessitated hospital admission. The rest of patients (N = 280) were assessed by using the pre-designed questionnaire for collecting their sociodemographic and clinical characteristics and were then subjected to GHQ where 114 patients proved to have a minor psychiatric morbidity (GHQ ≥ 7). Those study participants were subjected further to the assessment of their psychiatric morbidities by using SCID-1 (Figs. 1 and 2) (Table 1).
Sociodemographic data
Out of the total study sample (280 patients), the patients aged between 18 and 35 years comprise 55% (n = 154) of the total sample. The majority of the sample 84% (n = 236) had finished their university degree, and nearly half of the sample 50% (n = 140) were married, and 78.7% (n = 220) were employed, and 92% (n = 258) of the total sample were from urban areas.
While medical comorbidities distribution among the study sample showed that nearly half of them 43.6% (n = 122) were smokers, 11.4% (n = 32) had diabetes mellitus, and the same percent had hypertension, while only 5% (n = 14) suffered from cardiac diseases. With regard to the distribution of severity of COVID infection, our results revealed that 51% (n = 144) COVID patients had not been hospitalized and had normal daily activities, and 40% (n = 112) had not been admitted to the hospital, yet showed an impaired daily activity.
With regard to the laboratory data, the current study revealed that C-reactive protein (CRP) levels ranged between 2 and 88 mg/l with a mean of 24.38 ± 20.01. While systemic immune inflammatory index (SII) ranged from 126.35 to 6500 (cells/liter) and shows a mean of 1003.73 ± 789.49. The neutrophil–lymphocyte ratio (NLR) level ranged between 0.7 and 763 (cells/liter) and shows a mean of 9.60 ± 64.21. Furthermore, platelet-lymphocyte ratio (PLR) ranged from 1.77 to 1245 (cells/liter) and shows a mean of 174.28 ± 115.04. Finally, the D-dimer has ranged between 0.07 and 2.49 (μ/mL) and has a mean of 1.28 ± 1.21.
The current study revealed that 92.9% (n = 260) of the study participants were prescribed antipyretics, 75% of the participants were prescribed antibiotics, and 37.1% (n = 104) were on corticosteroids.
Clinical data of the study participants
The current study used the General Health Questionnaire to detect the potential cases, and it revealed that 40.7% (n = 114 out of 280) of the patients were positive on GHQ (score ≥ 7) with a mean score of 7.84 ± 5.07.
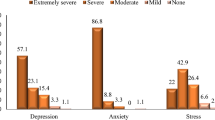
Then, those 114 patients were then subjected to SCID-1, in order to evaluate the occurrence of psychiatric disorders in post-COVID-19 patients who scored ≥ 7 on GHQ. Out of 114 patients who scored positive with GHQ, a total of 112 patients showed psychiatric morbidity. The “Results” revealed that the most prevalent disorder among the studied sample was depressive disorder as nearly half of the cases were having depressive disorder 45.6% (n = 52). Generalized anxiety disorder represents the second common disorder among the studied population (42.1% n = 48 patients). With regard to suicide distribution, the results demonstrated that eleven patients (9.6%) were having only suicidal ideation, but no suicidal plans or attempts. Detailed data on psychiatric morbidity in the study sample are illustrated in Table 1.
The results also showed high prevalance of subthreshold psychiatric symptoms among the studied sample (n = 114), where subthreshold generalized anxiety symptoms were among the highly prevalent types 17.5% (n = 20) followed by the subthreshold major depressive symptoms 14% (n = 16) and the least common subthreshold symptoms in the study sample were the OCD as it was seen in only 1.8% (n = 2) of patients.
Sociodemographic and clinical correlates associated with major depressive disorder
In this article, we are going to display the results of analysis of sociodemographic and clinical correlates with common psychiatric disorders mainly depression and anxiety.
The current results showed that being married (p = 0.019) is significantly associated with higher levels of major depressive disorder among study participants (Table 2). It also displayed a significant statistical association between having a cardiac disease (p = 0.007) and being on antibiotics (p = 0.033) with high prevalence of major depressive disorder among the study participants.
As shown in Table 3, studying the association between major depressive disorder and different laboratory parameters has revealed no significant association between prevalence of major depressive disorder and any of the laboratory parameters (p > 0.05) except for D-dimer (p = 0.022).
Sociodemographic and clinical correlates associated with generalized anxiety disorder
The current study revealed that higher prevalence rate of generalized anxiety disorder was significantly associated with unemployment (p = 0.001), female gender (p = 0.025), having Diabetes mellitus (0.002), cardiac diseases (p = 0.001), and high level of COVID severity with impaired daily activity (p = 0.029) (Table 4).
According to Table 5, no significant statistical association is detected between different laboratory parameter and high prevalence of GAD among study participants, however (Table 5).
Predictive factors for occurrence of early post-COVID major depressive disorder among the study participants
Multivariate analysis revealed that significant predictors of major depressive disorder were marital status, cardiac disease, antibiotics, and elevated D-dimer, with p-value (p < 0.05 significant), while the rest have insignificant with p-value (p > 0.05 NS) (Table 6).
Predictive factors for occurrence of early post-COVID-19 GAD among the study participants
Generalized anxiety disorder increased 2.455 times in female compared to male patients (OR: 2.455, CI: 2.215–5.321; p = 0.019). Also, working status increased the susceptibility for GAD 2 times compared to non-employed (p-value = 0.023). GAD was also increased with the presence of DM (OR: 3.162, CI: 1.960–4.712; p = 0.026) and cardiac diseases (OR: 2.363, CI: 1.465–3.520; p-value = 0.039). Furthermore, COVID psychiatric symptoms increased the odds for develo** GAD to 1.25 (p = 0.02). Multivariate analysis revealed that significant predictors of GAD full criteria were gender, working status, DM, cardiac disease, and COVID severity, with p-value (p < 0.05 significant), while the rest have insignificant with p-value (p > 0.05 NS) (Table7).
Discussion
The current study indicated that a majority of the study sample fell within the age range of 18 to 35 years. Consistent with our research, a study conducted in the UK revealed a significant rise in mental distress during the COVID-19 pandemic. Specifically, the study saw a nearly threefold increase in mental distress among individuals aged 18 to 24, while the 25 to 34 age group experienced an approximately twofold increase [23]. During the era following the COVID-19 pandemic, Alberto and his colleagues conducted a study which revealed that young adults exhibited a higher prevalence of mental health impairments compared to older patients [35]. The potential reasons for the variability in outcomes can be attributed to the type of socioeconomic circumstances in Egypt. The participant age range (18 to 35) group that is depicting those who were most frequently exposed to COVID as a result of their age of employment. Consequently, this demographic is more susceptible to exposure to the virus.
In this study, it was shown that a total of 114 participants, including approximately 41% of the sample, exhibited modest psychiatric morbidities as assessed using the GHQ scale. In line with our investigation, a prior study conducted in Spain reported that the average GHQ-28 score among their surveyed population was 13.676.6 [35].
The findings obtained from the utilization of the Structured Clinical Interview for DSM-5 (SCID-1) indicated that the predominant psychiatric disorder observed within the examined cohort was depressive disorder, with approximately half of the cases (45.6%, n = 52) exhibiting symptoms consistent with this condition. And the second most prevalent psychiatric disorder among the study population was generalized anxiety disorder, affecting 42.1% (n = 48) of the patients. Obsessive–compulsive disorder (OCD) was identified in 5.3% (n = 6) of the individuals included in the study, whereas panic disorder was observed in 1.8% (n = 2) of the study cohort. The findings of the study also indicated a prevalence rate of 1.8% (n = 2 patients) for comorbid post-traumatic stress disorder.
Based on a recent systematic study [36], the prevailing mental impairments frequently cited were depression and/or anxiety. The findings presented here correlate with a substantial body of prior research that has similarly reported congruent outcomes. A total of 47 papers were examined in relation to this subject matter. The findings varied from the absence of symptoms and signs of sadness or anxiety [37, 38] to a prevalence exceeding 30% during the follow-up period [39], which extended up to 199 days after discharge from the hospital. The observed disparities in outcomes between the studies mentioned above and the ones we conduct can be attributed to the utilization of distinct research apparatus and the considerable variation in the duration between subsequent examinations between investigations.
Two previous studies examined symptoms of obsessive–compulsive disorder (OCD) [29, 40]. In a study conducted by Mazza et al. (2020), an assessment of patients was performed to determine the presence of symptoms related to obsessive–compulsive disorder (OCD). The findings revealed that 20% of the patients displayed OCD symptoms during the follow-up period (Mazza et al., 2020). Gennaro et al. (2021) reported that within a period of 1 to 3 months, investigators saw improvements in symptoms associated with obsessive–compulsive disorder (OCD). The observed prevalence of obsessive–compulsive disorder (OCD) in the research we conducted was determined to be 5.3%.
This relatively low figure could potentially be explained by the heterogeneity in sample sizes and the utilization of different psychometric instruments for evaluating individuals with OCD. In our research, the SCID-1 interview was utilized for the purpose of diagnosing psychopathology. Additionally, the other studies’ investigations incorporated validated self-report questionnaires, such as the obsessive–compulsive inventory (OCI) [29, 40].
Post-COVID-19 PTSD incidence was reported in 20 papers, with findings ranging from 6.5 to 42.8% of the included patients. Low levels of our results in PTSD (1.8%) may be attributable to differences in sample size and psychometric instruments used to assess patients [41, 42].
It is worth noting that our results showed a high prevalence of subthreshold psychiatric symptoms among the studied sample (N = 114), where subthreshold generalized anxiety symptoms were among the highly prevalent types 17.5% (N = 20) followed by the subthreshold major depressive symptoms 14% (N = 16) and the least common subthreshold symptoms in the study sample was the OCD as it was seen in only 1.8% (N = 2) of patients.
In our study, the rate of subthreshold symptoms is lower than other previous studies. This could be attributed to the fact that we used SCID-I diagnostic interview for assessment of both threshold and subthreshold cases which is more specific and accurate, while other studies used self-rated questionnaires that might yield high false-positive results.
The impact of COVID-19 is widespread, as evidenced by the findings of a study conducted during the second wave of the pandemic [43]. This investigation revealed a significantly greater prevalence of likely depression (30.3%) compared to the general population. The criteria used to identify probable depression or anxiety were PHQ-9 or GAD-7 scores of 5 [39]. In the region of southern China, specifically in close proximity to Wuhan, it was observed that a significant proportion of healthcare professionals, similar to the overall population, exhibited symptoms indicative of sadness, anxiety, and sleeplessness. Specifically, around 50.4% of these professionals displayed probable symptoms of depression, while 44.6% exhibited probable symptoms of anxiety [44].
In this research, we examined the clinical investigation of suicidal ideations. It revealed that a total of eleven patients, accounting for 9.6% of the sample, reported experiencing suicidal thoughts exclusively, without any accompanying suicidal plans or attempts. Despite being recognized as a concealed crisis within the context of post-COVID syndrome, regrettably, there exists a dearth of research pertaining to the prevalence of suicidal risk in those experiencing post-COVID signs and symptoms. In a singular study, a total of 3.5% of participants indicated the presence of suicidal thoughts or behaviors 1 month after being infected [29].
The observed discrepancies in findings may be attributed to several factors, including variations in sample size. Notably, the study under consideration included a smaller sample of 402 patients, whereas our study encompassed a different sample size. Additionally, differences in the psychometric instruments employed for assessing suicidal tendencies may have contributed to the observed variability. Specifically, this study utilized the Beck Depression Inventory, a self-rated questionnaire, to evaluate suicidal ideations and plans. In contrast, our study employed clinical interviewing techniques to inquire about patients’ suicidal inclinations.
As regard risk and predictive factors for common post-COVID-19 psychiatric disorders. Studying the demographic and clinical correlates among our study sample revealed that being married (p = 0.019), having a cardiac disease (p = 0.007), and being on antibiotics (p = 0.033) are significantly associated with higher levels of major depressive disorder among study participants.
To further analyze the risk factors for depressive symptoms among the study sample, multivariable logistic regression was performed. Our study revealed that 45.6% having cardiac diseases increased the odds for develo** depression to 3.7 times (p = 0.045), while being married raised the odds to 1.1 times (p = 0.015). Furthermore, being on antibiotic increased the odds for develo** depression to 1.5 times (p = 0.030), while increased blood serum of D-dimer has raised the odds for depression to 3.7 times (p = 0.042).
One of the predominant risk factors for hospitalization and mortality in individuals with COVID-19 is the presence of preexisting cardiovascular disease (CVD) [45]. The proposition has been presented that hyperinflammation serves as an underlying mechanism that predisposes people with COVID-19 to develop severe cases of the disease, hence potentially increasing the likelihood of experiencing post-COVID depression [46]. Multiple studies have indicated that individuals suffering from cardiovascular disease may encounter symptoms of anxiety and sadness following a COVID-19 infection. These psychological consequences are attributed not only to the challenges arising from the disease itself but also to the impacts of the viral infection.
There is a paucity of research examining the correlation between elevated levels of D-dimer and the onset of post-COVID depression. Similar to our research, a recent study has demonstrated a longitudinal and autonomous correlation between symptoms of depression and levels of plasma D-dimer in healthy people who were monitored for up to 1 year following an acute myocardial infarction [47, 48].
The current study revealed that the risk factors associated with higher prevalence rate of generalized anxiety disorder are as follows: unemployment (p = 0.001), female gender (p = 0.025), having DM (0.002), and cardiac diseases (p = 0.001).
On conduction of multivariate logistic regression analysis, it was revealed that being employed would increase the susceptibility for generalized anxiety disorder by 2 times compared to non-employed patients (p = 0.023). GAD was also increased 3.1 times with the presence of DM (p = 0.026), and cardiac diseases increased the odds of GAD by 2.3 times (p = 0.039). None of the laboratory data was found to be associated with generalized anxiety disorders among the study sample. Similar to our findings, an increasing number of studies of COVID-19 survivors showed that anxiety symptoms after COVID 19 have been linked to female gender, disease severity, and symptom duration. Researchers followed up with over 4000 COVID-19 survivors and also found that the existence of comorbidities is a predictor for long COVID anxiety disorders [10].
Limitations
The main limitation of the present study is its cross-sectional nature that does not allow interpretation for causality. Due to the circumstances of the pandemic, we were not able to enroll a control group and thus are unable to confirm causality. Without such comparisons, it is not possible to completely differentiate between direct and indirect effects of COVID-19. Mental health problems may be consequences of chronic stress resulting from social and economic challenges of COVID-19, rather than a result of infection, in a proportion of PCS patients. It is also noteworthy that social consequences may be exacerbated for infected individuals. A limited time frame is considered one of the major restrictions, as study data collected from December 2021 to May 2022. Given the surge of research on COVID-19, timeframe restrictions on literature searches notably limit the inclusion of emerging data on the topic. In addition, sample size seems to be small and did not include all patients’ categories like those admitted to the ICU; statistical tests were not be able to identify significant relationships within data set such as depression/anxiety association with COVID severity and laboratory investigations especially D-dimer as well as medication used during COVID infection. Larger sample size could have generated more accurate results.
Recommendations
This research finding strongly recommends that clinicians should check all COVID-19 patients for mental health problems, regardless of the severity of the disease, treatment methods, and length of ICU stay. We do recommend involving a psychiatric outpatient service among any post-COVID follow-up clinics with a structured referral pathway.
Detailed and individualized assessment of mental status may enable the design of treatment plans including psychiatric outpatient programs. Larger studies, long-term symptom monitoring, and post-COVID syndrome and other survivor suicidality research are needed.
Conclusion
COVID-19 infection has demonstrated an increased risk of mental health problems in multiple domains. It was evident that depression was the most presenting psychiatric illness among the studied sample (45.6%), while generalized anxiety disorder was the second most prevalent disorder (42.1%). And suicide was found in 9.6% of the study sample. It is worth noting that our results displayed a high prevalence of subthreshold psychiatric symptoms. These findings emphasize the utmost need for mental health assessments for all survivors.
Availability of data and materials
The dataset created and analyzed during the current study will be uploaded with the manuscript in Excel file format and will be available from the corresponding author on reasonable request.
Abbreviations
- PCS:
-
Post-COVID syndrome
- GAD:
-
Generalized anxiety disorder
- CRP:
-
C-reactive protein
- GHQ:
-
General Health Questionnaire
References
Maltezou HC, Pavli A, Tsakris A. (2021) Post-COVID syndrome: an insight on its pathogenesis. Vaccines.;9(5). https://doi.org/10.3390/vaccines9050497
Taylor S (2022) The psychology of pandemics. Annu Rev Clin Psychol 9(18):581–609. https://doi.org/10.1146/annurev-clinpsy-072720-020131. Epub 2021 Nov 15 PMID: 34780260
Tenforde MW et al (2020) Symptom duration and risk factors for delayed returnto usual health among outpatients with COVID-19 in a multistate health care systems network—United States. Morb Mortal Wkly Rep 69:993–998
Huang C et al (2021) 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 397:220–232
WHO coronavirus disease (COVID-19) dashboard [Accessed 29 Mar 2021] Available from: https://covid19.who.int/.
Emergency use ICD codes for COVID-19 disease outbreak [Accessed 29 Mar 2021] Available from: https://www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak.
International Classification of Diseases, Eleventh Revision (ICD-11), World Health Organization (WHO) 2019/2021 https://icd.who.int/browse11.
Carfi A, Bernabei R, Landi F (2020) Against COVID-19 post-acute care study group. Persistent symptoms in patients after acute COVID-19. J Am Med Assoc 324:603–605
McElvaney OJ et al (2020) Characterization of the inflammatory response to severe COVID-19 illness. Am J Respir Crit Care Med 202:812–821
Alemanno F, Houdayer E, Parma et al (2021) COVID-19 cognitive deficits after respiratory assistance in the subacute phase: a COVID-rehabilitation unit experience. PLoS ONE 16:e0246590. https://doi.org/10.1371/journal.pone.024659
Chang MC, Park D (2020) Incidence of post-traumatic stress disorder after coronavirus, disease. Health Care 8:373
Evans RA, McAuley H, Harrison EM et al (2021) Physical, cognitive, and mental health impacts of COVID-19 after hospitalization (PHOSP-COVID): a UK multicenter, prospective cohort study. Lancet Respir Med 9(11):1275–1287
Mikkelsen ME, Abramoff B (2021) COVID-19: evaluation and management of adults following acute viral illness. In: Post TW (ed) UpToDate. UpToDate Inc, Waltham Accessed on Oct 30
Trougakos IP, Stamatelopoulos K, Terpos E, Tsitsilonis OE, Aivalioti E, Paraskevis D et al (2021) Insights to SARS-CoV-2 life cycle, pathophysiology, and rationalized treatments that target COVID-19 clinical complications. J Biomed Sci 28(1):1–18
Alpert O, Begun L, Garren P, Solhkhah R (2020) Cytokine storm induced new onset depression in patients with COVID-19. A new look into the association between depression and cytokines-two case reports. Brain, Behav Immunity-Health 9:100173
Altmann DM, Boyton RJ (2020) Confronting the pathophysiology of long COVID. BMJ Opinion, London
Castanares-Zapatero D, Chalon P, Van den Heede K (2022) Pathophysiology of long COVID: a preliminary report. COVID-19 KCE contributions. Belgian Health Care Knowledge Centre. Ann Med 54(1):1473–1487. https://doi.org/10.1080/07853890.2022.2076901
Yong SJ (2021) Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis 53(10):737–754
Morris SB, Schwartz NG, Patel P, Abbo L, Beauchamps L, Balan S et al (2020) Case series of multisystem inflammatory syndrome in adults associated with SARS-CoV-2 infection—United Kingdom and United States, March–August 2020. Morb Mortal Wkly Rep 69(40):1450
Kumar MA, Krishnaswamy M, Arul JN (2021) Post COVID-19 sequelae: venous thromboembolism complicated by lower GI bleed. BMJ Case Reports CP 14(1):e241059
Townsend L, Fogarty H, Dyer A, Martin-Loeches I, Bannan C, Nadarajan P et al (2021) Prolonged elevation of D-dimer levels in convalescent COVID-19 patients is independent of the acute phase response. J Thromb Haemost 19(4):1064–1070
British Society for Immunology (2020) Report: long-term immunological health consequences of COVID-19
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A et al (2020) Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 7:883–892
Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L et al (2020) Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 2020:6
Méndez R, Balanzá-Martínez V, Luperdi SC, Estrada I, Latorre A, González-Jiménez P et al (2021) Long-term neuropsychiatric outcomes in COVID-19 survivors: a 1-year longitudinal study. J Intern Med 291(2):247–251
Pan K-Y, Kok AAL, Eikelenboom M, Horsfall M, Jörg F, Luteijn RA et al (2021) The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 8:121–129
Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ (2021) 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8:416–427
Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL et al (2020) Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry 7:875–882
Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I et al (2020) Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun 89:594–600
Fancourt D, Steptoe A, Bu F (2021) Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8:141–149
Miller AH, Raison CL (2016) The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol 16:22–34
Najjar S, Pearlman DM, Alper K (2013) Neuroinflammation and psychiatric illness. J Neuroinflamm 10:43
Abdelghani M, Atwa SA, Said A et al (2022) Cognitive after-effects and associated correlates among post-illness COVID-19 survivors: a cross-sectional study. Egypt Egypt J Neurol Psychiatry Neurosurg 58:77. https://doi.org/10.1186/s41983-022-00505-6
El-Zoghby S, Soltan E, Salama H (2020) Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J Community Health 45(4):689–695. https://doi.org/10.1007/s10900-020-00853-5
Alberto L, Moncunill G, Tortajada M, Vidal M,Guinovart C. Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. 2020;11(1):3500. https://doi.org/10.1038/s41467-020-17318-x
Schou T, Joca S, Wegener G, Bay-Richter C (2021) Psychiatric and neuropsychiatric sequelae of COVID-19 – a systematic review. Brain Behav Immun 97:328–348. https://doi.org/10.1016/j.bbi.2021.07.018
Daher A, Balfanz P, Cornelissen C, Müller A, Bergs I, Marx N, Müller-Wieland D, Hartmann B, Dreher M, Müller T (2020) Follow up of patients with severe coronavirus disease 2019 (COVID-19): pulmonary and extrapulmonary disease sequelae. Respir Med 174:106197. https://doi.org/10.1016/j.rmed.2020.106197
Zhou H, Lu S, Chen J, Wei N, Wang D, Lyu H, Shi C, Hu S (2020) The landscape of cognitive function in recovered COVID-19 patients. J Psychiatr Res 129:98–102
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17:1705–1729
Mazza MG, Palladini M, De Lorenzo R, Magnaghi C, Poletti S, Furlan R, Ciceri F, Rovere-Querini P, Benedetti F (2021) Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun 94:138–147
Horn M, Wathelet M, Fovet T, Amad A, Vuotto F, et al. Is COVID-19 associated with posttraumatic stress disorder? J Clin Psychiatry. 2020;82(1) https://doi.org/10.4088/JCP.20m13641
Bellan M, Soddu D, Balbo PE, Baricich A, Zeppegno P et al (2021) Respiratory and psychophysical sequelae among patients with COVID-19 four months after hospital discharge. JAMA Netw Open 4:e2036142
Liao YH, Fan BF, Zhang HM, Guo L, Lee Y, Wang WX et al (2021) The impact of COVID-19 on subthreshold depressive symptoms: a longitudinal study. Epidemiol Psychiatr Sci 30:e20. https://doi.org/10.1017/S2045796021000044. Published online 2021 Feb 15
Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M (2020) Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med Sci Monit 26:e924609
Medzikovic L, Cunningham CM, Li M, Amjedi M, Hong J, Ruffenach G et al (2020) Sex differences underlying preexisting cardiovascular disease and cardiovascular injury in COVID-19. J Mol Cell Cardiol 148:25–33
Landmesser U, Lehmann I, Eils R (2021) Hyperinflammation as underlying mechanism predisposing patients with cardiovascular diseases for severe COVID-19. Eur Heart J 42(18):1720–1721
von Känel R, Pazhenkottil A, Meister-Langraf A, Znoj H et al (2021) Longitudinal association between cognitive depressive symptoms and D-dimer levels in patients following acute myocardial infarction. Clin Cardiol. 44(9):1316–1325. https://doi.org/10.1002/clc.23689. Published online 2021 Jul 7
Wu D, Yang XO (2020) TH17 responses in cytokine storm of COVID-19: an emerging target of JAK2 inhibitor fedratinib. J Microbiol Immunol Infect 53(3):368–370
Acknowledgements
Not applicable.
Funding
The research was totally funded by the researchers.
Author information
Authors and Affiliations
Contributions
All authors had made a substantial contribution to the design of work, data collection and interpretation, writing the manuscript, revising it, and approving the final version. AZ made the main effort in patient data collection. WS, MB, and ZM made the major contribution in analyzing the results, reviewing current literature, and writing the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Ethical Committee of the Armed Forces College of Medicine, Ministry of Defense, Institutional Review Board (V.G.IRB-1–010) (37 MEETING 25 September 2021). A written informed consent was obtained from the selected patients. The researchers described the study to the patients, ensured the confidentiality of their information, and obtained their written informed consent for participation. The researchers stated that participation in the study was voluntary, and that the patients had the freedom to withdraw from the assessment at any time, and that patients might withdraw from the evaluation at any moment without affection of their treatment plan.
Consent for publication
Not applicable. Manuscript does not contain data from any individual person, images or case reports, etc.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sabry, W., El Dien, M.B., Elsherbiny, A.I.Z. et al. Early post-COVID-19 common psychiatric complications: role of basic inflammatory, coagulation, and clinical risk factors. Middle East Curr Psychiatry 30, 112 (2023). https://doi.org/10.1186/s43045-023-00376-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00376-4