Abstract
Background
Previous studies showed that top-quality embryo transfer (ET), number of transferred embryos, endometrial preparation with natural cycles or mild stimulation, and female BMI independently affected the outcome in frozen-thawed ET. However, the effect of culturing thawed cleavage embryos to blastocyst stage on the outcome was not sufficiently elucidated. Our objective is to evaluate the role of this extended culturing as predictor of cycle outcome in vitrified-thawed ICSI cycles.
Materials and methods
One thousand forty-two consecutive cycles of vitrified-thawed ET done in a single IVF unit [Mansoura Integrated Fertility Centre (MIFC)] were reviewed during a period from 2014 to 2017. Endometrial preparation methods were natural, stimulation by antiestrogen and/or gonadotropins, or replacement using sequential estradiol (E2) and progesterone (P4). The primary outcome was the clinical pregnancy rate while the secondary outcome was the chemical and ongoing pregnancy rate.
Results
Overall clinical pregnancy rate (CPR) is 298/1042 is 28.5%, chemical pregnancy rate (326/1042) 31.3%, and ongoing pregnancy rate (167/615) 27.2%. Comparing clinically pregnant (n = 298) and non-pregnant (n = 744) showed, respectively, the following: age 28.76 ± 5.0, 28.85 ± 5.18 (p = 0.8); BMI 31.06 ± 5.9, 32.45 ± 5.9 (p = 0.002); infertility duration 4.17 ± 3.2, 4.6 ± 3.5 (p = 0.038); endometrial thickness 10.82 ± 1.6, 10.13 ± 2.06 (p = 0.0001); and no. of ET 3.35 ± 1.5, 3.12 ± 1.60 (p = 0.035). The clinical pregnancy rate when vitrification was done on cleavage embryos was 198/502 (39.4%), and when vitrification done on blastocyst stage 100/ 536 (18.7%) (P < 0.0001); endometrial preparation: natural 72/240(29.1%), stimulated 204/680 (30.0%) replacement 17/90 (18.8%) (p = 0.09); extended culture of cleavage embryos to blastocyst stage: clinical pregnancy rate 116/194 (59.7%) chemical pregnancy rate 125/194 (64.1%), ongoing pregnancy rate 87/165 (52.7%) and non extended culture clinical pregnancy rate 182/848 (21.4%), chemical pregnancy rate 201/848 (23.7%), and ongoing pregnancy rate 80/450 (17.7%) (P < 0.0001).
Conclusion
Top-quality ET, number of transferred embryos and extended culture of cleavage embryos to blastocyst stage, cleavage embryos but not infertility duration, BMI, endometrial thickness, or hCG trigger of ovulation independently predict successful outcome in frozen cycle ET and extended culture of cleavage embryos significantly improved clinical and chemical and ongoing pregnancy rates.
Similar content being viewed by others
Background
Societal changes together with increasing opportunity and welling to preserve fertility had extended the indications of assisted reproduction technologies (ART). This in association with great evolutions in embryo cryopreservation had re-framed the therapeutic field in infertility management [1]. The first reported human pregnancy as a result of a cryopreserved embryo was in 1983 while in 1984 the first live birth from cryopreservation was reported [2, 3].
The great advances in vitrification techniques increased the capability to perform elective freezing of the whole embryos which will be transferred in the next cycles [4]. This was firstly indicated in high responders for fear of the development of ovarian hyperstimulation syndrome (OHSS) [5]. Controlled ovarian stimulation (COS) was hypothesized to cause endometrial disturbance and embryo-endometrial asynchronization that led to a suggestion of practicing a liberal utilization of elective frozen embryo transfer (eFET) by a lot of fertility clinics to decrease the development of OHSS besides enhancing the outcome of IVF/ICSI cycles [6, 7]. As declared by the US Centre for Disease Control and Prevention, the percentage of frozen embryo transfer (FET) following freezing all cycles was 20% at 2005 and escalated to 50% in 2014 with a concomitant decrease in fresh ET [8]. It was postulated that elective frozen embryo transfer (eFET) will be considered as the gold standard maneuver in IVF/ICSI programs [9]. This suggestion was dependent mostly upon evidence from observational data and minimal randomized trials. In agreement with this, Roque et al. (2013) reported that elective frozen embryo transfer (eFET) was introduced pre-termly as a new line of treatment in IVF/ICSI programs without sufficient randomized controlled trials [1]. The conventional slow freezing technique was associated with a lower success rate in spite of the many trials to enhance the procedure encompassing improved cryoprotectants, adjusting time, rate, and cooling devices [10]. This was possibly attributed to change of a liquid embryo or oocyte to a solid state with the formation of ice intracellular leading to cellular morphological disturbance [10]. A shift to vitrification from slow freezing was noticed in the past years that entailed the suspension of embryos in a glass-like state after ultrarapid freezing with cryoprotective additives at higher concentrations [11]. The advantages of this turnover is that vitrification causes a reduction in ice nucleation and crystals formation [12], an increase of embryo cryo-survival together with a more better clinical pregnancy and live birth rates [13,14,15]. These advantages were behind the conclusion that vitrification is more effective than slow frozen methods irrespective of embryo stage whether cleavage or blastocyst stage [13].
Several factors were determined to affect the frozen ET outcome: female age which inversely affects the outcome [16], high and low BMI which were found to increase miscarriage rate [17], the quality of embryos before freezing as good quality associated with better survival and elevated pregnancy rates [18], and regaining of cleavage activity of the thawed embryos which is accompanied with better outcome [19]. Also, a natural cycle regimen was recommended for frozen ET in cases with ovulatory and regular cycles with added advantages of avoiding daily subcutaneous injection and being inexpensive [20]. Fragmentation of sperm DNA and the peri-implantation serum progesterone level were considered among important factors and it was recommended that future research must be focused on those points [1]. It was found that studying the role of the post thawed embryo culture was insufficiently elucidated; while the studies on this issue were focusing on the comparison of short culture for 3–5 h to overnight culture, the effect of extended culturing for 48 h of thawed cleavage embryos to blastocyst stage on the outcome was not evaluated.
We aimed to evaluate the role of an extended culture of post-thawed CSE to BSE among other independent variables as a predictor of cycle outcome in vitrified-thawed ICSI cycles using binomial logistic regression (BNLR).
Materials and methods
Study design
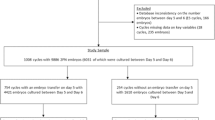
This is a retrospective cohort study of women who had undergone ICSI-ET cycles in Mansoura Integrated Fertility Centre (MIFC) in Mansoura, Egypt, during a period from 2014 to 2017. The inclusion criteria used in the study were vitrified-thawed ET cycles after ICSI treatment. The exclusion criteria used in the study were women with Natural cycles, those undergone fresh ET cycles, and cases with non-top-quality embryos. A total of 1042 consecutive cycles of vitrified-thawed ET fulfilling inclusion and exclusion criteria were reviewed. The following parameters were included: female age at vitrification, female BMI, duration of infertility, cause and type of infertility, endometrial thickness, number of transferred embryos, embryo stage at vitrification, embryo quality (top or non-top), endometrial preparation, embryo culture, and ovulation triggering. The criteria of male gametes were not included because all types of sperm sources (ejaculate, epididymal aspirate, or testicular biopsy) yield similar fertilization, cleavage, and cycle outcome) [21]. Nor does the state of male gamete whether fresh or frozen affect ICSI outcome [22]. The primary outcome was determining the independent predictors of clinical pregnancy with visible heart rate employing BNLR. Secondary outcome measure was the effect of extended culture on chemical and ongoing pregnancy rates.
Embryo grading and selection for vitrification
Following fertilization and the transfer of fresh embryos on either day 3 or day 5 after oocyte retrieval, the remaining top-quality embryos were selected for vitrification (all embryos in freeze-all cases). Embryos were assessed in accordance with Istanbul’s Consensus [23]. Day 3 embryos were assessed as Top-quality as follows: a number of blastomeres 7–8 cells of proper size, ≤ 20% fragmentation, the presence of an integrated zona pellucida, and no vacuoles and no multiple nuclei. Grading for day 5 blastocysts is based on the assessment of blastocoel expansion, inner cell mass (ICM), and trophectoderm (TE) appearance.
Vitrification procedure of the selected embryos
Day 3 and day 5 embryos were frozen using a Vitrification Freezing Kit (Kitazato, Japan). Selected embryos were removed from cleavage medium to equilibrium solution (ES: 7.5% ethylene glycol (EG) and 7.5% dimethyl sulfoxide (DMSO) at room temperature) for 6–12 min (time was defined by the re-expansion of the embryos) and then transferred into vitrification solution (VS: 15% EG, 15% DMSO and 0.5 M sucrose) for 60–90 s. The excess VS solution was removed to leave just a thin layer surrounding each embryo on the Cryo-top straw (Kitazato, Japan) and was immediately plunged into liquid nitrogen at − 196 °C.
Endometrial preparation
Natural cycles were used for ovulatory cases which were monitored by transvaginal ultrasound (TVS) starting on the 10th day of the cycle and then every other day until the leading follicle reached 18–20 mm, endometrial thickness at least 8 mm; when ovulation was triggered by 10,000 IU hCG IM (Choriomon®, IBSA, Switzerland) or is checked by measuring urinary LH. Thawing of frozen embryo was scheduled for transfer after 5 days for cleavage ET and 7 days for blastocyst ET and considering hCG injection day or LH detection as day zero. In stimulated cycles we employed oral ovulatory drugs; antiestrogens (50 mg clomiphene citrate oral tablet (Clomid®, Sanofi Aventis, France) twice daily for 5 days starting on 3rd day of cycle), or aromatase inhibitors ((Letrozole 2.5 mg oral tablet (Femara®, Novartis, Switzerland)) twice daily for 5 days starting on the 2nd day of cycle) with or without sequential hMG (Menopur, Ferring, Spain); (75 IU daily subcutaneous started on day 8 till the leading follicles reached 15 mm); to achieve endometrial estrogenic stimulation through endogenous production of estrogen by growing follicles. When leading follicle(s) reached 18–20 mm ovulation was triggered by exogenous urinary hCG 10,000 IU IM (Choriomon®, IBSA, Switzerland). Timing of ET was scheduled in the same way as mentioned above with natural cycles. The replacement regimen consisted of estradiol valerate 2 mg oral tablet (Progynova®, Bayer Schering, Germany) twice daily for 5 days starting on the day 3 of the cycle, then 2 mg three times daily for 5 days. Endometrial thickness was measured by TVS on the 10th day of the cycle. When at least 8 mm thickness was achieved, progesterone was added to estrogen. We used progesterone 100 mg IM (Prontogest®, IBSA, Switzerland) daily or vaginal progesterone 400 mg suppository (Cyclogest®, Actavis, UK) daily plus 2 mg estradiol valerate oral tablet (Progynova®, Bayer Schering, Germany) twice daily for 3 days for cleavage ET or 5 days for blastocyst ET.
Embryo transfer procedure
Timing of ET
Timing of ET was scheduled by HCG triggering of ovulation or monitoring spontaneous ovulation by the utilization of both transvaginal ultrasound and ovulation kits.
Thawing
The inner straw was removed from liquid nitrogen (LN2) and plunged directly in a large droplet (200 μl) of TS media (thawing solution: 1 M sucrose) preheated to 37 °C. The embryo(s) were left in this media for 1 min on a heated stage (37 °C), and then transferred into 100 μl of DS media (dilution solution: 0.5 M sucrose) for 4 min. Lastly, washing was performed twice each of 4 min in 100 μl WS media (Washing Solution: HEPES-buffered solution of Medium-199 containing gentamicin sulfate 35 μg/mL HEPES and 20% DSS).
Culture
Cleaved embryos were cultured to blastocyst stages in a cleavage medium (COOK Medical, Sydney, Australia). Thawed CSE were cultured for 24–48 h to reach BSE.
Grading of embryos
Grading of embryos was performed depending on the criteria of top and non-top-quality embryos. Categorizing a top-quality embryo when it had 7–8 cells and fragmentation of less than 20% [24]. Damaged embryo was diagnosed when not all but more than half of blastomeres survived thawing. Dead embryo was considered when less than half of blastomeres survived thawing and were neglected.
Embryo transfer
Thawed embryos were transferred 5–7 days after hCG trigger or LH result became positive in a natural or stimulated cycle or 3–5 days of progesterone in replacement cycles by using the blind tactile method described previously [25] or ultrasound-guided transfer.
Luteal support
Vaginal progesterone suppository 400 mg/day (Cyclogest®, Actavis, UK) or IM progesterone 100 mg/day (Prontogest®, IBSA, Switzerland) was used. Luteal support in natural and stimulated cycles was started on ET day whereas, in the replacement cycle, progesterone was started when endometrial thickness under estrogen priming reached at least 8 mm and after 3–5 days of P4 treatment thawed embryos were transferred. luteal support was continued for 2 weeks after ET. In pregnant cases, luteal support was continued until 10–12 weeks of pregnancy.
Successful endpoint
Successful endpoint was a clinical pregnancy which was defined by an existence of a gestational sac with visible cardiac pulsations by transvaginal ultrasound at 6 weeks of pregnancy (2 weeks after positive pregnancy test).
Statistical analysis
It was achieved by the IBM statistical Package for the Social Sciences software package, version 20. Significance was considered when P ˂ 0.05. For normally distributed quantitative data comparison between means was done using a two-tailed Student t-test and for comparing proportions, we used chi-square test (χ2). In order to assess the predictive value of the different independent variables shown in the results to be significantly different in pregnant and nonpregnant outcomes (Tables 1 and 2) which include BMI, infertility duration, endometrial thickness, use of hCG ovulation trigger, number of transferred embryos, vitrification day 3 or 5, extended culture, and the ratio of top-quality embryos transferred. Since cycle outcome is a qualitative variable (pregnant or nonpregnant) a binomial logistic regression model (BNLR) was chosen using enter method. We noticed collinearity between the vitrification stage and extended culture of thawed CSE and excluded the verification stage from independent predictors. The model was statistically significant, Chi-square (8 df) = 61.45, P = 0.000. The model explained 29.2% (Nagelkerke’s R2) of the variance and correctly predicted 77% % of the cases. The model performance was assessed by the Hosmer and Lemeshow test (Table 3) indicating goodness-of-fitness of the model with p = 0.358 (> 0.05) which means good performance with an absence of a high degree of correlation.
Results
This study included 1042 consecutive cycles of vitrified-thawed ET. The overall clinical pregnancy rate (CPR) was 298/1042 (28.5%), chemical PR (326/1042) 31.3%, ongoing PR (167/615) 27.2%. As shown in Table 1, Comparing pregnant group (n = 298) and non-pregnant (n = 744) showed respectively; mean age was not significantly different [ 28.76 ± 5.0, 28.85 ± 5.18 and P = 0.8]. BMI significantly lower in pregnant group [31.06 ± 5.9, 32.45 ± 5.9 and P = 0.002]. The duration of infertility significantly lower in pregnant group [4.17 ± 3.2, 4.6 ± 3.5 respectively and P = 0.038]. The pregnant group had significantly higher endometrial thickness [10.82 ± 1.6, 10.13 ± 2.06 and P = 0.0001]. Regarding number of transferred embryos, a significantly higher number was transferred in pregnant group [3.35 ± 1.5, 3.12 ± 1.60 and P = 0.035] (Fig. 1).
Table 2 show the effect of different vitrified-thawed cycle parameters on cycle outcome. As regard embryo stage at vitrification, pregnancy rate was significantly higher with CSE compared with BSE (CSE = 198/502 (39.4%) and BSE = 100/536 (18.7%), P = 0.001). Top-quality embryos showed a significantly higher pregnancy rate compared to non-top-quality embryos 216/684 (31.5%), 0/68 (0%), respectively (P = 0.001). Regarding endometrial preparation pregnancy rates were as follows: natural cycles 70/240 (29.1.%), stimulated cycles 204/680 (30.0%), and replacement cycles 17/90 (18.8%). The difference was statistically insignificant (P = 0.09). Regarding utilization of extended culture, with extended culture of CSE to BSE clinical pregnancy rate was 116/194 (59.7%), chemical PR 125/194 (64.1%), ongoing PR 87/165 (52.7%) while without culture the corresponding values were respectively 182/848 (21.4%), 201/848 (23.7%), and ongoing PR 80/450 (17.7%); these differences were highly significant P = ˂ 0.0001. When hCG triggering of ovulation was used pregnancy rate was 212/610 (34.7%) while non-hCG was 66/370 (17.8%) and thes difference was highly significant (P = ˂ 0.001). Table 4 compared frozen cleavage and blastocyst transfer. There were no significant differences in cycle features nor in cycle outcome apart from significantly shorter infertility duration in blastocyst reflecting tendency towards younger age. BNLR model output (Table 5) was statistically significant, chi-square (8 DF) = 61.46, P = 0.000. The model explained 29.29% (Nagelkerke R2) of the variance and correctly predicted outcome in 77% of the cases. The Wald criterion demonstrated that top-quality grade embryo, extended culture and number of embryos transferred independently predict positive clinical outcome (P ˂ 0.05) but endometrial thickness, hCG ovulation triggering, infertility duration, and BMI did not predict (P ˃ 0.05)).
Discussion
Improvements in vitrification protocols have enabled elective freezing of all embryos, followed by transfer in a subsequent cycle, also known as elective frozen embryo transfer (eFET), ‘freeze-all’, deferred ET or cycle segmentation [4]. Nowadays, assisted reproduction practice considers vitrified-thawed embryos to be an integral part in IVF/ICSI cycles. This is owing to overwhelming shift towards elective single ET and the expected better outcome when the embryo is transferred to the prepared endometrium to have a physiologic hormonal environment. However, a recent systematic review and meta-analysis [4] and a prospective cohort study [26] concluded that there are currently no clinical data supporting the indiscriminate use of elective frozen embryo transfer (eFET) for all patients submitted to IVF/ICSI. Based on the available randomized controlled trials (RCT), it seems appropriate to implement this strategy in patients at risk of OHSS, in hyper-responders, and in those undergoing preimplantation genetic testing for aneuploidy (PGT-A) at the blastocyst stage [4, 26]. In our own practice, we follow this conclusion and segmented or freeze all ICSI practice accounts for only 15% of cases (unpublished data). Most of our frozen embryo transfer (FET) cycles are cases with frozen transfer following previous fresh transfer. The study clarified that the predictors of successful outcome in vitrified-thawed ICSI cycles were top-quality embryos, number of embryos transferred, and extended culture of post-thawed cleavage embryos (CSE to BSE). Although we found that endometrial thickness, timing ET by hCG triggering of ovulation, wife’s BMI, and infertility duration are significantly different in pregnant and pregnant outcome (Tables 1 and 2), yet however these variables are not independently predictive of outcome of FET cycle as proved by the BNLR model. This comes in partial agreement with the study of Veleva et al. [27] who found that predictors of FET were top-quality embryo and the number of embryos transferred and unlike our study, they found that endometrial preparation protocol and BMI also independently predicted live birth in FET [27]. The variance between our study and that of Velva et al. [27] regarding BMI as an independent predictor of FET outcome is that our study primary outcome measure was clinical pregnancy with visible cardiac activity while that of Velva et al. [27] was live birth rate. It is known that higher BMI is associated with more early pregnancy loss [27, 28]. The number of embryos transferred an independent predictor of a successful outcome in frozen ET cycles which came in agreement with those reporting the transfer of 2 embryos in frozen cycles was associated with a better outcome [27, 29, 30]. In contrast, other recommended transfer of a single high-quality vitrified-thawed embryo is exactly similar to the strategy of elective single ET in fresh cycles [31]. Among the determinant factors of the frozen ET outcome was the female age which affect inversely the outcome [16, 29, 32]. In our FET study we did not find a significant difference between pregnant and pregnant cases agreeing with Ashrafi et al. who commented that if we have enough good-quality eggs and embryos, the age does not have an effect on pregnancy outcome.
In our results we found that endometrial preparation by natural cycle or mild stimulation tended to have a better outcome, chi-square, P = 0.09, and hCG ovulation trigger more significantly associated with improved outcome (P < 0.0001) compared with hormonal replacement and no hCG ovulation trigger However BNLR model showed that endometrial preparation protocol and hCG trigger of ovulation are not independent predictors of pregnancy. In agreement with us, a meta-analysis by Groenewoud et al. and Cochrane systematic review declared no significant difference between natural and stimulated cycles for endometrial preparation, [8, 33].
Veleva et al. [27] found that overnight culture of thawed embryos had no independent predictive effect on live birth in variance with our results. The difference between Veleva et al. and our study can be explained by the fact that the culture in our study was for an extended time (24–48 h) changing the embryo stage from cleavage stage to blastocyst stage. Also, the study by Veleva et al. [27] contained exclusively vitrified cleavage stage embryos many of which were non-top-quality. Joshi et al. [34] in a retrospective study of 518 FET found that overnight culture of cleavage embryos resulted in an improved outcome of the FET cycle if the embryo resumed cleavage after thawing compared with embryos transferred within 2 h of thawing and those overnight culture that did not resume cleavage. Eftekhar et al. [35] in a prospective study of 134 FET found that blastocyst formation after thawing of cleavage stage embryos was a good predictor for embryo viability and pregnancy outcome giving credence to our results. In this study, we found no significant difference in cycle outcome between unselected cleavage and blastocyst embryo transfer (Table 3). This goes in agreement with the known observation that in FET cycles unselected CSE or BSE offers similar reproductive outcomes [36, 37]. This is in contrast with fresh cycle transfers where there is near general agreement with good evidence that BSE transfer is associated with better cycle outcome [36, 37]. The essence of this difference is “embryo self-selection” to reach fresh BSE and in frozen ET to allow cleavage embryo stage to self-select and to reach BSE. This selection allows better synchrony between blastocyst and endometrium.
To the best of our knowledge, this study is among the few studies on the place of post thawing extended culture to 24–48 h among predictors of success in vitrified-thawed ICSI cycles. One of the important findings in the study is the positive role of culturing CSE to BSE on cycle outcome. In agreement with our finding, regarding the culture of post thawed embryos, Ziebe et al. [38] proved that regaining cleavage potential is accompanied by higher pregnancy and implantation rates and considered it as a sole criterion in selecting the best embryo for successful transfer and outcome. This finding was also confirmed by several studies which reported that the resumption of cleavage division after the overnight culture is a crucial parameter to enhance pregnancy and implantation rates [39, 40]. In favor of preference of blastocyst ET, Tannus et al. in a study found poor outcomes with fresh day 5 ET and reported significantly improved outcomes on delaying fresh transfer and extend culture until the achievement of a fully expanded blastocyst that will be used in vitrified-thawed ET later on [41]. Contradictory to our finding, a study of short (2–5 h) versus long (18–24 h) post thawed culture period indicated a higher implantation and live birth rate in short cultured embryos and attributed this to exposure of embryos to more culture stress in long period [42]. However, this study by Rato et al. [42] spanned a long period and used slow freezing rather than ultra-rapid freezing (vitrification) which is used in our study. Guo et al. [43] searched the effect of post-thawed culture for 2–4 h or 20–24 h on the frozen cycle outcome (using vitrification rather than slow freezing) and showed no significant difference between both groups. Although Veleva et al. and Agha-Rahimi et al. concluded that no benefit of overnight culture on the cycle outcome and attributed this to the non-improvement of the quality of embryo with culture, nevertheless, they reported that it facilitated the best embryo selection to be transferred. Also, Veleva reported an important confounder in his study which was significantly higher implantation rate with D3 top-quality ET in relation to D2 top-quality ET, this was not the same with non-top-quality embryos and recommended further research to clarify such issue [27, 44]. This actually was answered in this study that documented the role of extended culture of cleaved embryo to blastocyst stage in improving frozen cycle outcome. The available culture systems provide embryos with environment similar to physiological situations.
Among merits of this study, it was among few studies which investigated the role of extended post-thawed culture of cleavage embryo to blastocyst stage and demonstrated a definite role in a successful outcome in vitrified-thawed cycles. Despite it being a retrospective study, it was a single-center long experience with a considerable number of included studied cycles beside limited heterogeneity of the studied group that added to the strength of the results. Limitations were non-investigations of possible other predictors like, role of smoking, number of retrieved oocytes, and socioeconomic status of participants, also since our center is a referral center; details of live births and take-home baby rates were not available, besides it was a retrospective and single-center study. So, we recommended further prospective multicenter works to confirm the results and investigate other factors.
Conclusion
Top-quality ET, number of transferred embryos, and extended culture of cleavage stage embryo to blastocyst stage embryo independently predict a successful outcome in frozen-thawed ET cycles.
Availability of data and materials
The data that support the findings of this study are available on reasonable request from the corresponding author, [MA].
References
Bosch E, De Vos M, Humaidan P (2020) The future of cryopreservation in assisted reproductive technologies. Front Endocrinol (Lausanne) 11:67. https://doi.org/10.3389/fendo.2020.00067
Trounson A, Mohr L (1983) Human pregnancy following cryopreservation, thawing and transfer of an eight-cell embryo. Nature 305(5936):707–709. https://doi.org/10.1038/305707a0
Zeilmaker GH, Alberda AT, van Gent I, Rijkmans CM, Drogendijk AC (1984) Two pregnancies following transfer of intact frozen-thawed embryos. Fertil Steril 42(2):293–296. https://doi.org/10.1016/s0015-0282(16)48029-5
Roque M, Haahr T, Geber S, Esteves SC, Humaidan P (2019) Fresh versus elective frozen embryo transfer in IVF/ICSI cycles: a systematic review and meta-analysis of reproductive outcomes. Hum Reprod Update 25(1):2–14. https://doi.org/10.1093/humupd/dmy033
Devroey P, Polyzos NP, Blockeel C (2011) An OHSS-Free Clinic by segmentation of IVF treatment. Hum Reprod 26(10):2593–2597. https://doi.org/10.1093/humrep/der251
Roque M, Lattes K, Serra S, Sola I, Geber S, Carreras R, Checa MA (2013) Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril 99(1):156–162. https://doi.org/10.1016/j.fertnstert.2012.09.003
Zhu Q, Chen Q, Wang L, Lu X, Lyu Q, Wang Y, Kuang Y (2018) Live birth rates in the first complete IVF cycle among 20 687 women using a freeze-all strategy. Hum Reprod 33(5):924–929. https://doi.org/10.1093/humrep/dey044
Groenewoud ER, Cohlen BJ, Macklon NS (2018) Programming the endometrium for deferred transfer of cryopreserved embryos: hormone replacement versus modified natural cycles. Fertil Steril 109(5):768–774. https://doi.org/10.1016/j.fertnstert.2018.02.135
Cohen J, Alikani M (2013) The time has come to radically rethink assisted reproduction. Reprod Biomed Online 27(4):323–324. https://doi.org/10.1016/j.rbmo.2013.08.001
Argyle CE, Harper JC, Davies MC (2016) Oocyte cryopreservation: where are we now? Hum Reprod Update 22(4):440–449. https://doi.org/10.1093/humupd/dmw007
Sekhon L, Lee JA, Flisser E, Copperman AB, Stein D (2018) Blastocyst vitrification, cryostorage and warming does not affect live birth rate, infant birth weight or timing of delivery. Reprod Biomed Online 37(1):33–42. https://doi.org/10.1016/j.rbmo.2018.03.023
Son WY, Tan SL (2009) Comparison between slow freezing and vitrification for human embryos. Expert Rev Med Devices 6(1):1–7. https://doi.org/10.1586/17434440.6.1.1
Loutradi KE, Kolibianakis EM, Venetis CA, Papanikolaou EG, Pados G, Bontis I, Tarlatzis BC (2008) Cryopreservation of human embryos by vitrification or slow freezing: a systematic review and meta-analysis. Fertil Steril 90(1):186–193. https://doi.org/10.1016/j.fertnstert.2007.06.010
Wong JY, Wong AY (2011) Phasing-in of vitrification into routine practice: why, how, and what. Hong Kong Med J 17(2):119–126
Li Z, Wang YA, Ledger W, Edgar DH, Sullivan EA (2014) Clinical outcomes following cryopreservation of blastocysts by vitrification or slow freezing: a population-based cohort study. Hum Reprod 29(12):2794–2801. https://doi.org/10.1093/humrep/deu246
Karlstrom PO, Bergh C (2007) Reducing the number of embryos transferred in Sweden-impact on delivery and multiple birth rates. Hum Reprod 22(8):2202–2207. https://doi.org/10.1093/humrep/dem120
Veleva Z, Tiitinen A, Vilska S, Hyden-Granskog C, Tomas C, Martikainen H, Tapanainen JS (2008) High and low BMI increase the risk of miscarriage after IVF/ICSI and FET. Hum Reprod 23(4):878–884. https://doi.org/10.1093/humrep/den017
Salumets A, Suikkari AM, Makinen S, Karro H, Roos A, Tuuri T (2006) Frozen embryo transfers: implications of clinical and embryological factors on the pregnancy outcome. Hum Reprod 21(9):2368–2374. https://doi.org/10.1093/humrep/del151
Guerif F, Bidault R, Cadoret V, Couet ML, Lansac J, Royere D (2002) Parameters guiding selection of best embryos for transfer after cryopreservation: a reappraisal. Hum Reprod 17(5):1321–1326. https://doi.org/10.1093/humrep/17.5.1321
Peeraer K, Couck I, Debrock S, De Neubourg D, De Loecker P, Tomassetti C, Laenen A, Welkenhuysen M, Meeuwis L, Pelckmans S, Meuleman C, D’Hooghe T (2015) Frozen-thawed embryo transfer in a natural or mildly hormonally stimulated cycle in women with regular ovulatory cycles: a RCT. Hum Reprod 30(11):2552–2562. https://doi.org/10.1093/humrep/dev224
Bukulmez O, Yucel A, Yarali H, Bildirici I, Gurgan T (2001) The origin of spermatozoa does not affect intracytoplasmic sperm injection outcome. Eur J Obstet Gynecol Reprod Biol 94(2):250–255. https://doi.org/10.1016/s0301-2115(00)00347-x
Yu Z, Wei Z, Yang J, Wang T, Jiang H, Li H, Tang Z, Wang S, Liu J (2018) Comparison of intracytoplasmic sperm injection outcome with fresh versus frozen-thawed testicular sperm in men with nonobstructive azoospermia: a systematic review and meta-analysis. J Assist Reprod Genet 35(7):1247–1257. https://doi.org/10.1007/s10815-018-1206-5
(2011) The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod 26(6):1270-83. https://doi.org/10.1093/humrep/der037
Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G, Eestermans W, Gerris J (1999) Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod 14(9):2345–2349. https://doi.org/10.1093/humrep/14.9.2345
Ghanem ME, Ragab AE, Alboghdady LA, Helal AS, Bedairy MH, Bahlol IA, Abdelaziz A (2016) Difficult embryo transfer (ET) components and cycle outcome. Which is more harmful? Middle East Fertil Soc J 21(2):114–9. https://doi.org/10.1016/j.mefs.2015.10.004
Smith A, Tilling K, Lawlor DA, Nelson SM (2019) Live birth rates and perinatal outcomes when all embryos are frozen compared with conventional fresh and frozen embryo transfer: a cohort study of 337,148 in vitro fertilisation cycles. BMC Med 17(1):202. https://doi.org/10.1186/s12916-019-1429-z
Veleva Z, Orava M, Nuojua-Huttunen S, Tapanainen JS, Martikainen H (2013) Factors affecting the outcome of frozen-thawed embryo transfer. Hum Reprod 28(9):2425–2431. https://doi.org/10.1093/humrep/det251
Lashen H, Fear K, Sturdee DW (2004) Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod 19(7):1644–1646. https://doi.org/10.1093/humrep/deh277
Karlstrom PO, Bergh T, Forsberg AS, Sandkvist U, Wikland M (1997) Prognostic factors for the success rate of embryo freezing. Hum Reprod 12(6):1263–1266. https://doi.org/10.1093/humrep/12.6.1263
Ying-hui Y, Fan J, Chen-ming X, Lan-feng X (2002) Factors influencing the outcome of embryo freezing and thawing program. J Zhejiang Univ Sci A 3(4):493–496. https://doi.org/10.1007/BF02839497
Hydén-Granskog C, Unkila-Kallio L, Halttunen M, Tiitinen A (2005) Single embryo transfer is an option in frozen embryo transfer. Hum Reprod 20(10):2935–2938. https://doi.org/10.1093/humrep/dei133
Goldman RH, Racowsky C, Farland LV, Munne S, Ribustello L, Fox JH (2017) Predicting the likelihood of live birth for elective oocyte cryopreservation: a counseling tool for physicians and patients. Hum Reprod 32(4):853–859. https://doi.org/10.1093/humrep/dex008
Ghobara T, Gelbaya TA, Ayeleke RO (2017) Cycle regimens for frozen-thawed embryo transfer. Cochrane Database Syst Rev 7:CD003414. https://doi.org/10.1002/14651858.CD003414.pub3
Joshi BV, Banker MR, Patel PM, Shah PB (2010) Transfer of human frozen-thawed embryos with further cleavage during culture increases pregnancy rates. J Hum Reprod Sci 3(2):76–79. https://doi.org/10.4103/0974-1208.69340
Eftekhar M, Aflatoonian A, Mohammadian F, Tabibnejad N (2012) Transfer of blastocysts derived from frozen-thawed cleavage stage embryos improved ongoing pregnancy. Arch Gynecol Obstet 286(2):511–516. https://doi.org/10.1007/s00404-012-2303-9
Carvalho BR, Barbosa MW, Bonesi H, Gomes DBS, Cabral ÍO, Barbosa AC, Silva AA, Iglesias JR, Nakagawa HM (2017) Embryo stage of development is not decisive for reproductive outcomes in frozen-thawed embryo transfer cycles. JBRA Assist Reprod 21(1):23–26. https://doi.org/10.5935/1518-0557.20170007
Glujovsky D, Farquhar C, QuinteiroRetamar AM, Alvarez Sedo CR, Blake D (2016) Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev 6:Cd002118. https://doi.org/10.1002/14651858.CD002118.pub5
Ziebe S, Bech B, Petersen K, Mikkelsen AL, Gabrielsen A, Andersen AN (1998) Resumption of mitosis during post-thaw culture: a key parameter in selecting the right embryos for transfer. Hum Reprod 13(1):178–181. https://doi.org/10.1093/humrep/13.1.178
Tang R, Catt J, Howlett D (2006) Towards defining parameters for a successful single embryo transfer in frozen cycles. Hum Reprod 21(5):1179–1183. https://doi.org/10.1093/humrep/dei490
Solé M, Santaló J, Rodríguez I, Boada M, Coroleu B, Barri PN, Veiga A (2011) Correlation between embryological factors and pregnancy rate: development of an embryo score in a cryopreservation programme. J Assist Reprod Genet 28(2):129–136. https://doi.org/10.1007/s10815-010-9498-0
Tannus S, Cohen Y, Henderson S, Al Ma’mari N, Shavit T, Son WY, Dahan MH (2019) Fresh transfer of Day 5 slow-growing embryos versus deferred transfer of vitrified, fully expanded Day 6 blastocysts: which is the optimal approach? Hum Reprod 34(1):44–51. https://doi.org/10.1093/humrep/dey351
Rato ML, Gouveia-Oliveira A, Plancha CE (2012) Influence of post-thaw culture on the developmental potential of human frozen embryos. J Assist Reprod Genet 29(8):789–795. https://doi.org/10.1007/s10815-012-9793-z
Guo L, Luo C, Quan S, Chen L, Li H, Guo Y, Han Z, Ou X (2013) The outcome of different post-thawed culture period in frozen-thawed embryo transfer cycle. J Assist Reprod Genet 30(12):1589–1594. https://doi.org/10.1007/s10815-013-0120-0
Agha-Rahimi A, Omidi M, Akyash F, Faramarzi A, Farshchi FA (2019) Does overnight culture of cleaved embryos improve pregnancy rate in vitrified-warmed embryo transfer programme? Malays J Med Sci 26(2):52–58. https://doi.org/10.21315/mjms2019.26.2.6
Acknowledgements
Not applicable.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
IA: Project development, Data analysis, Manuscript writing. MG: Project development, Data Collection, Data analysis. LE: Project development, Data Collection. YM: Project development, Data Collection. AH: Data Collection. MA: Project development, Data analysis, Manuscript writing. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The MIFC review board approved this study. Consent to participate: waived due to anonymized unidentifiable data before enrollment in the study.
Consent for publication
Waived due to anonymized unidentifiable data before enrollment in the study.
Competing interests
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albahlol, I., Ghanem, M., Elboghdady, L. et al. Extended culture of cleavage embryo to blastocyst embryo is among the good predictors of successful outcome in vitrified-thawed ICSI cycles. Middle East Fertil Soc J 27, 13 (2022). https://doi.org/10.1186/s43043-022-00105-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-022-00105-7