Abstract
Epilepsy is a recurring neurological disease caused by the abnormal electrical activity in the brain. This disease has caused about 50 new cases in 100,000 populations every year with the clinical manifestations of awareness loss, bruising, and mobility abnormalities. Due to the lack understanding of the pathophysiology behind the illness, a wide variety of medications are available to treat epilepsy. Epileptogenesis is the process by which a normally functioning brain undergoes alterations leading to the development of epilepsy, involving various factors. This is related to the inflammation which is driven by cytokines like IL-1 and tumor necrosis factor-α (TNF-α) leads to neuronal hyperexcitability. Pro-inflammatory cytokines from activated microglia and astrocytes in epileptic tissue initiate an inflammatory cascade, heightening neuronal excitability and triggering epileptiform activity. The blood-brain barrier (BBB) maintains central nervous system integrity through its tight endothelial connections, but inflammation impact BBB structure and function which leads to immune cell infiltration. The mammalian target of rapamycin (mTOR) pathway’s excessive activation influences epileptogenesis, impacting neuronal excitability, and synapse formation, with genetic mutations contributing to epilepsy syndromes and the modulation of autophagy playing a role in seizure onset. The apoptotic pathway contribute to cell death through glutamate receptor-mediated excitotoxicity, involving pro-apoptotic proteins like p53 and mitochondrial dysfunction, leading to the activation of caspases and the disruption of calcium homeostasis. Ionic imbalances within neural networks contribute to the complexity of epileptic seizures, involving alterations in voltage-gated sodium and potassium channels, and the formation of diverse ion channel subtypes. Epileptogenesis triggers molecular changes in hippocampus, including altered neurogenesis and enhanced expression of neurotrophic factors and proteins. Oxidative stress leads to cellular damage, disrupted antioxidant systems, and mitochondrial dysfunction, making it a key player in epileptogenesis and potential neuroprotective interventions. Thalamocortical circuitry disruption is central to absence epilepsy, the normal circuit becomes faulty and results in characteristic brain wave patterns.
Similar content being viewed by others
Introduction
Epilepsy is one of the most prevalent neurological conditions that is caused by the abnormal electrical activity in the brain. It is a chronic, paroxysmal, and recurring disease marked by neurobiological, cognitive, psychological, and social factors that collectively contribute to recurrent seizures, alongside enduring risk factors for epileptic episodes [1, 2]. Epilepsy may significantly reduce quality of life, as it limits daily activities, social contacts, and even work chances. Moreover, this disease has caused about 50 new cases in 100,000 populations every year. About 75% of these cases start in childhood indicating the increased vulnerability of brain development to experience seizures [1, 2]. Clinical signs of epilepsy include loss of awareness, mobility abnormalities, sensation (vision, hearing, and taste), mood or cognitive capacities, bruising, and the danger of mortality. A study showed that medication will control the seizures of around 60% to 70% of persons with epilepsy. The general likelihood of epilepsy recurring after experiencing a solitary seizure ranges from 27-71%. Roughly 70% of children will enter a phase where they experience a span of at least 2 years without encountering a seizure. Due to the lack of a complete understanding of the pathophysiology behind the illness, a wide variety of medications are available to treat epilepsy. This circumstance results in a variety of distinct pharmaceutical agents to treat it. Epilepsy characterized by epileptic seizures starts in the gray matter of cortex or subcortex. Epileptic seizures results from an abrupt imbalance between excitation and inhibition in the network of cortical neurons. It starts when neurons exhibit high, coordinated, and sustained neuronal excitability activity.
The term hypersynchrony and hyperexcitability are two different words found in the epilepsy pathophysiology with a related significance among them. The abnormal reactivity of neurons to stimulation input is referred to as hyperexcitability. This condition happens when neurons react too strongly when they receive signals from other cells causing excessive firing of nerve cells in the brain. Neurons commonly start more than two or one electrical activity, which is known as hypersynchrony. This involves several neighboring neurons in aberrant electrical bursts. In this case, a small number of neurons first undergo abnormal stimulation. The normal inhibitory ion exchange and membrane conductance of the synaptic gap are altered, which raises neuronal excitability and synchronization and results in an epileptic seizure. Hyperexcitability is typically brought on by modifications to intrinsic neuronal components and synapse function. According to developments in molecular genetics, several distinct types of human epilepsy are considered to be brought on by mutations in ion channel genes [3,4,5,6,7,8]. This article aims to comprehensively delve into the intricate molecular underpinnings that give rise to epileptic seizures and the overarching epileptic condition, thereby contributing to a more profound understanding of the etiological complexities inherent to epileptogenesis.
Epileptogenesis
Epileptogenesis refers to the process through which a normal brain develops alterations that contribute to the formation of epilepsy, alluding brain transformation that was previously functioning normally into a brain that experiences seizures. Thus far, the definition of epileptogenesis remains a topic of ongoing discussion and lacks a universally accepted characterization. This considered involving two processes, including the development of epileptiform processes after brain injury and the process leading to the first spontaneous epileptic seizure. Research shows that neurological alterations during the latent period persist long after epilepsy has been identified and aid in the disease’s development, it means that the mechanisms involved in both starting and develo** epilepsy are counted as part of epileptogenesis. The subsequent development or changes that occur following epileptogenesis is called epileptic maturation. The processes of starting epilepsy and what happens afterward are different from each other, it involves the establishment of enduring alterations in neural circuitry and excitability, also often characterized by an increased propensity for recurrent seizures and the manifestation of clinical epileptic symptoms [4]. Prior to the occurrence of the epileptic seizure, the gradual changes of epileptogenesis occurs in neuronal excitability led to changes in interconnections and structure. This include the neurodegeneration, neurogenesis, gliosis, axonal damage or sprouting, dendritic plasticity, breakdown of the BBB, infiltration of inflammatory cells into the brain parenchyma, re-organization of the extracellular matrix, and re-organization of the molecular architecture of individual neurons [9].
Excitability also occurs in the membrane or metabolic components changes of individual neurons. It includes the ictogenesis from specific neurons, neuronal surroundings, and neuronal populations. This results from the suboptimal environmental control, extracellular ion concentration, and neurotransmitters. A neuron can develop into a population of hyperexcitable neurons through anatomical and physiological modifications [5, 10]. By blocking synaptic and voltage-gated inhibitory conductance or activating synapse and voltage-gated excitatory conductance, epileptic activity can be acutely produced. However, it differs from acute seizures in persistent epileptic seizures which are unexpected and less often. In chronic epilepsy, a second mechanism is required to account for the timing of the episodic change from regular activity to an epileptic seizure.
The biological processes, structural changes, and functional alterations play a crucial role in epileptogenesis. The fundamental physiology of an epileptic seizure includes the instability of the cell membrane or the surrounding or neighboring supporting cells. A contributing factor to cell membrane instability involves the deficiency of adenosine triphosphate (ATP) acetate associated with ion transport or anomalies in potassium ion conductance. Some examples of neurotransmitters that can boost excitability and expand neuronal activity are glutamate, aspartate, acetylcholine, norepinephrine, histamine, corticotropin-releasing factor, purines, peptides, cytokines, and steroid hormones. At the same time, dopamine and γ-amino butyric acid (GABA) restrict neuronal activity and growth. During an epileptic seizure, there is an increased blood flow requirement to the brain, facilitating the transportation of carbon dioxide and metabolic substrates essential for neuronal activity. Various forms of epilepsy are associated with mutations in a multitude of genes. It encompasses several types that are correlated with genes encoding protein subunits of voltage-sensitive and ligand-activated ion channels [4, 8].
Epileptic seizures and epilepsy arise from a multitude of causes and sustained through a process of positive reinforcement, where an initial imbalance between neural inhibition and excitation triggers further imbalances. The initial triggering activity not only initiates the seizure but also fosters ongoing neural excitation while simultaneously inhibiting the natural restraining mechanisms. This self-perpetuating cycle is facilitated by positive feedback, effectively prolonging the epileptic seizure once it has been initiated [11]. Epileptogenesis is influenced by factors including oxidative stress, neurochemical alterations in the brain due to neurotransmitters and ion channels, fluctuations in ion concentration, variations in cell surface receptors, and the presence of inflammation. Some targets in epileptogenesis include the mammalian target of rapamycin (mTOR), P-glycoprotein (P-gp), and mutations in voltage-gated ion channels like hyperpolarization-activated cyclic nucleotide-gated (HCN) channels and Kv7 channels (or M-channels), Na-K-2Cl cotransporter isoform 1 (NKCC1) [8, 12].
The role of inflammation in epileptic seizure and epilepsy
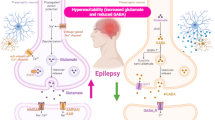
Inflammation indeed plays a significant role in the progression of epileptogenesis. It reduces the threshold for the initiation of epileptic seizures, and it becomes further exacerbated under conditions of SE [8]. Death of neuronal cells, malfunction of synapses, and the onset of hyperexcitability are all symptoms of brain injury brought on by concussions, hypoxia, or febrile convulsions. The release of cytokines, chemokines, lipid mediators, and protectins into the neuronal environment indicates that brain trauma has caused an organized cascade of biological processes. Depending on the part of the brain that is affected, dysregulation of these mediators and the expression of their receptors might result in clinical symptoms that include permanent neuronal injury [13] (Fig. 1).
The role of inflammation in epileptic seizure and epilepsy. A cascade of events unfolds after brain injury that triggers central inflammation and alters normal neuronal connections in the hippocampus. Meanwhile, systemic inflammatory diseases cause inflammation in the peripheral tissues, accelerating the accumulation of inflammatory agents. This dual inflammation, both in the peripheral and central systems, contributes to the weakening of the protective BBB by enhancing the levels of inflammatory agents. This compromised barrier permits the infiltration of immune cells, initiating heightened neuronal activity and further amplifying the production of inflammatory agents. The uncontrolled inflammation in both peripheral and central regions, coupled with the compromised blood-brain barrier, sets the stage for structural changes in synaptic connections within the hippocampus. These processes culminate in the progression of epilepsy. Adapted from Rana and Musto [13]
Brain inflammation in people with epilepsy
Epileptogenesis is closely linked to high degree of inflammation in the neural tissue’s milieu both acutely and persistently. The central nervous system may be the source of the inflammatory response with possible damage to the BBB. This inflammation can spread from the central nervous system into the systemic circulation, and exacerbations of pre-existing chronic neuroinflammation may also occur as a result of acute neuroinflammation [13]. Small amounts of the cytokine interleukin-1 (IL-1) are produced by activated astrocytes and microglia and expressed in the human central nervous system, these levels are increased during pathogenic processes. These cytokines cause astrocytes to consume less and release more glutamate, resulting in neuronal hyperexcitability. IL-1 is thought to cause epileptic seizures by increasing N-methyl-D-aspartate (NMDA) receptor expression in post-synaptic cells through activation of the GluN2B subunit of the NMDA receptor [13,14,15].
Active astrocytes and microglia emit the pro-inflammatory cytokine tumor necrosis factor-α (TNF-α). Several research shows that TNF-α controls N-cadherin which is essential for the development and structure of excitatory and inhibitory synapses. TNF-α also boosts glutaminase production at gap junctions, which in turn causes microglia to release more glutamate. TNF-α also increase the the expression of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, which amplifies glutamatergic transmission and results in excessive calcium ion influx and neurotoxicity. It also triggers GABA receptor endocytosis which reduces the inhibitory excitability, and results in significant alterations in excitability [13,14,15]. Another multifunctional cytokine that will increase along with the increment of TNF-α, IL-1β, and interferon-γ (IFN-γ) is the interleukin-6 (IL-6) which controls inflammation as immunological responses. The production of IL-6 in the central nervous system remains in low level. However, it can be boosted by the activation of astrocytes and microglia. The increasing levels of IL-6 expression reduces long-term potentiation (LTP), inhibits hippocampus neurogenesis, and increases gliosis, which lead to epileptogenesis [13,14,15]. The innate and acquired immune systems are activated in patients with epilepsy. Analysis of brain samples from patients with refractory epilepsy demonstrated heightened expression of IL-1β and high-mobility group box 1 (HMGB1), along with their corresponding receptors, namely interleukin-1 receptor type I (IL-1RI) and TLR4, in both glia cells and neurons. This clarifies that patients with epilepsy experience activation of inflammatory mechanisms [8, 13].
Targets and sources of cytokines and inflammatory mediators in epileptic tissue
Microglia and astrocytes as glial cells and non-neuronal parts of the central nervous system are the source of pro-inflammatory cytokines in epileptic tissue. In epileptogenesis, glial cells control inflammatory and immunological responses, it causes a rapid inflammatory response in epileptic seizures caused by chemo seizures or electrical stimulation. Within the first 30 minutes of an epileptic seizure, activated astrocytes and microglia trigger heightened levels of pro-inflammatory cytokines, such as IL-1β, IL-6, and TNF-α. This process initiates an inflammatory cascade that involves neurons and BBB endothelial cells, ultimately leading to the activation of the acquired immune system. This cascade includes the activation of NF-κB, COX-2, complement system, chemokines, and acute phase proteins. These cytokines have the potential to influence susceptibility to stimuli that trigger epileptic seizures, as well as contribute to the increased IL-1β levels resulting from epileptic convulsions. The initiation of this signaling cascade exacerbates epileptic seizures. The conversion of IL-1β into its active form is facilitated by the enzyme IL-1β converting enzyme (ICE/caspase-1). Considering this, exploring ICE/caspase-1 inhibitors as potential targets for antiseizure medications holds promise [4, 8, 12].
Rapid HMGB1 release from neurons, microglia, and astrocytes after pro-convulsant-induced brain injury was also shown to significantly influence the onset of brain inflammation and lower the threshold for epileptic seizures. Toll like receptor (TLR) signaling also plays a significant role in astrocytes and neurons. Injured or stressed cells emit danger signals to warn the surrounding environment of impending or ongoing damage, including in the HMGB1. The innate immune response and accompanying inflammatory pathways are activated in the tissue due to the interaction between HMGB1 and its cognate TLR4 [4, 8, 12]
The role of cytokines on neuronal excitability
Inflammatory cytokines play a role in changing neuronal excitability, producing toxic mediators, and making the BBB more impermeable. The proconvulsant effects are produced by NMDA receptors and IL-1β. Specifically, IL-1β can phosphorylate the NR2B subunit of the NMDA receptor via IL-1RI-dependent activation of Src kinases and neuronal sphingomyelinases. This phosphorylation amplifies NMDA-mediated calcium ion influx into neurons, thereby inducing neuronal hyperexcitability. Activated astrocytes release glutamate, which serves as the primary source, initiating a gradual influx of ions into neurons. This process involves NMDA receptors that incorporate the NR2B subunit. This influx of ions has a direct impact on excitatory events, exerting a substantial influence on neural synchronization and potentially giving rise to action potentials within neurons.
An essential biological mechanism that intensifies epileptic seizures involves the protein IL-1β. Furthermore, IL-1β has the capacity to reduce glutamate absorption by astrocytes, elevate glutamate release from glial cells through TNF-α, and induce hyperexcitability. The presence of IL-1β also leads to an inhibition of glutamate uptake by nitric oxide. Similar to IL-1β, TNF-α might boost the expression of AMPA receptors, facilitating the entry of calcium ions into neurons, while concurrently diminishing the expression of GABA receptors, thereby weakening the potency of inhibitory synapses. The signaling cascade mechanism governing glutamate exocytosis from astrocytes involves the participation of tumor necrosis factor (TNF-α). This process engages tumor necrosis factor receptor 1 (TNFR1) activation within astrocytes, thereby amplifying the signaling cascade responsible for glutamate release. This mechanism operates through the stimulation of CXCR4-dependent signaling in both astrocytes and microglia. Furthermore, it works synergistically to facilitate the release of TNF-α [4, 8, 12].
Inflammatory cytokines can lead to neuronal death through apoptosis, operating independently from excitotoxicity. This effect is potentially facilitated by the release of neurotoxic mediators. Additionally, glutamatergic excitotoxicity, which involves AMPA and NMDA receptors, can also contribute to neuronal demise. Inflammatory responses can also change the permeability of BBB. When BBB is damaged, astrocytes take up serum albumin. Within astrocytes, this albumin binds to TGF-β receptors, initiating a sequence of events that culminate in neuronal hyperexcitability and epileptiform activity. The impairment of the BBB leads to increased abnormal neuronal depolarization processes. The breach in the BBB allows leukocytes to enter the brain parenchyma and proteins to leak from the serum. These exogenous inflammatory mediators collectively reduce the threshold for epileptic seizures. This scenario underscores the significant impact of inflammatory processes on epileptogenesis within the brain [4, 8, 12]. The pathophysiology of epileptic seizures involves the adherence of inflammatory cells. After a pilocarpine hydrochloride-induced epileptic seizure, there is an increase in the production of vascular cell adhesion molecules (VCAM) and an increase in leukocyte adherence to endothelial cells in cerebral blood arteries, which is mediated by leukocyte mucin P-selectin glycoprotein ligand-1 and leukocyte integrins. Consequently, escalated leukocyte extravasation, brain inflammation, BBB leakage, increased neuronal excitation, and ultimately, the onset of epileptogenesis ensue [4]
Peripheral inflammation has been correlated with the stimulation of gene transcription through NF-κB, an unconventional intracellular signaling pathway activated by pro-inflammatory mediators within epileptogenic tissue. The recognition of this distinct mechanism provides insights into the genesis of epileptic seizures driven by neuronal hyperexcitability. This pathway regulates a subset of interactions between neuronal and glial elements that contribute to the reduction in the threshold for epileptic seizures [8, 16]. When pro-inflammatory molecules activate other kinase families, such as mitogen-activated protein kinase (MAPK), protein kinase A (PKA), and protein kinase C (PKC), voltage-dependent calcium, sodium, and potassium ion channels undergo rapid post-translational changes that have a significant effect on neuronal excitability. Increased extracellular glutamate levels are caused by IL-1 promoting glutamate release by glial cells and decrease glutamate absorption by astrocytes through the generation of TNF-α. Furthermore, the amplified glutamatergic transmission, a consequence of IL-1β produced by both neurons and astrocytes, yields pro-convulsant effects. Recent findings emphasize the critical role of astrocytic glutamate release in sha** the initiation and severity of epileptic convulsions. Additionally, IL-1 impedes inhibitory transmission by blocking GABA-mediated chloride ion influx. The presence of inflammatory compounds in the brain could also incite enduring transcriptional processes, thereby activating genes integral to the plasticity mechanisms underlying epileptogenesis [8, 16]
The role of P2X7 receptors in epilepsy
The P2X7 receptor is a cation-permeable ATP-gated non-selective ionotropic receptor expressed only by neurons and glia cells in the brain. Neuronal excitability in the hippocampus was shown to be modulated by activation of this receptor, which is also linked to microglia activation and neuro-inflammatory reactions. These receptors play a role in the neurological system disorders, such as epilepsy. P2X receptors are ligand-gated ion channels that ATP activates, and activating these receptors transfers signals between neurons and glia cells. Potassium ion concentration in the extracellular space rises during an epileptic episode. The Pannexin1 (Panx1) channels of hippocampal neurons and astrocytes activate in response to this alteration, releasing ATP. Neuronal hyperactivity brought on by the activation of ATP receptors leads to the onset of an epileptic seizure. Adenosine, as opposed to ATP, exhibits anti-epileptic action via P1A1 receptors. These purinergic receptors are inhibited from releasing glutamate when they are activated. Several P2X family receptors, including P2X2, P2X4, and P2X7, are damaged in the hippocampus during status epilepticus (SE). Following SE, a reduction in P2X2 receptor expression was also observed. In contrast, P2X7 receptor expression was higher in glial and neuronal injury regions. After SE, neuronal death is reduced by a lack of P2X4 receptors [12].
The structural, molecular, and functional alterations of BBB in epileptogenesis and epilepsy
BBB, which is impermeable to a wide range of chemicals, toxins, and cells due to the presence of non-fenestrated endothelial cells forming inter-endothelial tight connections, serves as a protective shield for the central nervous system, preventing any immune system reactions. The BBB is composed of both chemical and structural barriers. It comprises neovascular units such as the basement membrane, endothelial cells that line the blood arteries, neurons, astrocyte processes, tight junctions, and pericytes. These components collectively form the structural barrier of the BBB. Nectrin 1, functioning as a laminin-like protein responsible for regulating glial cell motility, is secreted by endothelial cells in response to signals from astrocytes, which concurrently produce the sonic hedgehog protein. In a concerted effort to fortify the BBB and diminish the infiltration of leukocytes, netrin 1 plays a crucial role in enhancing endothelial junctional proteins. These include occludins, claudins, junctional adhesion molecules (JAMs), and endothelial selective adhesion molecules (ESAM). This ensemble of proteins collectively widens the intercellular gaps, constituting the foundational elements of tight junctions and intercellular barriers. Members of the immunoglobulin superfamily, such as ESAM and JAMs, play a pivotal role in both the formation and upkeep of tight junctions. The basement membrane, constituting a foundational structure, embeds components like type 4 collagen, fibrillin, laminin, fibronectin, extracellular matrix proteins, and parasite matrix proteins, which collectively give rise to the basal capillaries or basement membrane. Within the brain capillaries, tight junctions are safeguarded by efflux transporters, forming a chemical barrier. These transporters, operating at the junctions between endothelial cells, necessitate the presence of ATP. Prominent among these are P-gp and breast cancer resistance protein (BCRP), functioning as flux transporters. Their active mechanism involves pum** potentially harmful lipophilic compounds back into the bloodstream, thereby restricting the assimilation of certain medicinal substances into the brain parenchyma. Furthermore, the chemical barrier of the BBB derives additional strength from the drug-metabolizing enzyme cytochrome P450 (CYP450), which is localized within the endothelial cells of brain capillaries. Studies by Rana & Musto [13] and Löscher & Friedman [17] have underscored these aspects. During epileptic seizures, the release of glutamate, facilitated by NMDA and COX-2 receptors, is accountable for the escalation in P-gp activity [12].
Seizures or the processes underlying them have the potential to impact the BBB, brain capillaries, and the neovascular unit in diverse ways. This can encompass thickening of the basement membrane, alterations in the constituent endothelial cells of the BBB, modifications in the neurons comprising the neovascular unit, and changes in the astrocyte processes forming the glia limitans—a secondary barrier. Epileptogenic brain injury can lead to the leakage of blood albumin and immune cells into the brain parenchyma. Notably, the escalated expression of efflux transporters such as P-gp and BCRP on the apical surface of endothelial cells, along with heightened activity of the enzyme CYP450 on these cells, has been associated with BBB damage. Concurrently, the presence of persistently activated microglia clusters may contribute to the disruption of the BBB. Furthermore, post brain injury, astrocytes undergo alterations in both morphology and function. These changes can collectively lead to a complex interplay of factors influencing the integrity and functionality of the BBB and related systems [17].
The mechanism by which epileptic convulsions impact the BBB remains uncertain. Observations in epilepsy patients and experimental animal models suggest that BBB failure can occur before, during, or after an epileptic seizure. Epileptic convulsions induce temporary changes in both the structural and functional aspects of the BBB. Within 30 min of an epileptic episode, there is a rapid increase in permeability that persists for hours. Elevated levels of glutamate during epileptic episodes disrupt the BBB. The expression and activity of MMP-2 and MMP-9 at the BBB also rise during seizures, contributing to BBB dysfunction. These matrix metalloproteinases influence the integrity of the BBB by altering the extracellular matrix surrounding brain capillaries and degrading the tight junction proteins that line the endothelium. The extracellular matrix, in turn, affects processes like AMPA receptor mobilization, paired-pulse depression, L-type voltage-dependent calcium channel activity, and the long-term potentiation (LTP) process. Changes in the expression of hyaluronic acid, a crucial component of the neuronal extracellular matrix, can lead to dysregulation of calcium ions and neuronal hyperexcitability. Inducing epileptic seizures can also permit ions to enter the parasite, thereby modifying its function and the constituents of the BBB both in vitro and in vivo. These defense system breaches, causing epileptic seizures, can establish a positive feedback loop. In this loop, seizures resulting from these breaches lead to a continuation of epileptic episodes, ultimately culminating in epilepsy. The breach of the cerebral blood barrier defense can trigger epileptic episodes and contribute to the development of epilepsy [6, 14, 17].
The BBB serves as a crucial barrier to maintain the peripheral immune cells in a healthy state, preventing their entry into the central nervous system. However, when breached, the BBB can allow both innate and acquired peripheral immune cells, including monocytes, neutrophils, B cells, and T cells, to infiltrate the central nervous system. These immune cells then carry out specific functions that could be either neuroprotective, neurotoxic, or even a combination of both. A significant facet of neuro-inflammation involves the entrapment of these immune cells within the central nervous system through the BBB. This orchestrated process hinges on adhesion interactions between lymphocytes and capillary endothelium. When immune cells come into contact with the activated endothelium, selectins facilitate loose binding, causing the leukocytes to roll along the endothelial surface. Additionally, chemokines present on the luminal surface of the endothelium trigger the activation of leukocytes, leading to the engagement of leukocyte integrins and subsequent halting of leukocyte movement on the endothelial surface. Once the appropriate adhesion occurs, immune cells can traverse into the perivascular space through either of two transmigration processes: the trans-cellular route, where they navigate through the endothelial cell body, or the paracellular route, utilizing the endothelial cleft. Upon infiltrating the perivascular space, these immune cells interact with resident perivascular immune cells before being guided by chemoattractants like chemokines and cytokines toward the brain parenchyma. Employing an enzyme-mediated mechanism, these infiltrating lymphocytes breach the glia limitans and access the brain parenchyma. Once within the brain parenchyma, they become stimulated to produce cytokines, contributing to the cascade of immune responses and inflammation. The BBB serves as a sentinel that regulates the entry of peripheral immune cells into the central nervous system. Breaching the BBB leads to a series of orchestrated events involving adhesion, activation, and migration of immune cells, ultimately culminating in their interaction with brain parenchymal cells and the release of cytokines [17].
Albumin extravasation plays a significant role in both epileptogenesis and the migration of immune cells across a compromised BBB. The initiation of acute epileptic seizures can be attributed to BBB impairment, and the progression from epileptic episodes to epilepsy is facilitated by the osmotic disruption of the BBB. Once extravasated, albumin enters the brain parenchyma and binds to various cellular components, including neuronal cells, astrocytes, and microglia. This binding triggers a sequence of events, including the entry of albumin into astrocytes through the TGF-β receptors. Consequently, the expression of critical components such as the Kir 4.1 channel, the water channel aquaporin 4 (AQP4), and glutamate transporters is reduced. This alteration results in a decreased ratio of extracellular potassium to glutamate, creating an environment that facilitates NMDA receptors in triggering epileptiform activity and amplifying neuronal hyperexcitability. The impact of TGF-β signaling extends further, encompassing changes in the extracellular matrix, excitatory synaptogenesis, pathological plasticity, and inflammation-related transcriptional alterations. These cumulative effects collectively contribute to the lowering of the threshold for epileptic seizures during the process of epileptogenesis. In essence, albumin extravasation sets in motion a complex cascade of events that involve multiple cellular components and signaling pathways. This interplay ultimately heightens neuronal excitability and paves the way for epileptogenesis and the progression towards epilepsy [17]. Albumin binding to TGF-RII receptors on astrocytes triggers the activation of the TGF-β signaling pathway, leading to the production of TGF-β. This, in turn, activates astrocytes, causing a disruption in the balance between cellular potassium and glutamate levels. Additionally, the ALK5/TGF-β pathway is responsible for inducing excitatory synaptogenesis [13]. In models of epileptogenesis, augmenting TGF-β signaling has been shown to have a preventive effect on the development of epilepsy. Furthermore, another study established a connection between compromised BBBs and irregular neuronal activity [17].
Damage to the BBB triggers gliosis and activation of astrocytes. After inducing SE, astrocytes positive for glial fibrillary acidic protein (GFAP) become activated within a span of 24 to 48 h. Reactive gliosis becomes evident around three to four months following the initial insult. The inability of these reactive astrocytes to effectively manage extracellular glutamate leads to hyperexcitability and neuronal damage. Furthermore, these activated astrocytes release C-C motif chemokine ligands 2, 3, and 5, fostering interactions with other inflammatory cells and giving rise to the production of pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α. This cascade contributes to heightened neuronal excitability, the onset of seizures, cell death, and the propagation of neuro-inflammation [13].
The role of mTOR pathway in epileptic seizure and epilepsy
The excessive activation of the mTOR signaling pathway directly influences the progression of epileptogenesis and neuronal excitability. This process involves the phosphorylation of molecules within this pathway. Additionally, the mTOR pathway plays a role in governing the expression of glutamate receptors. Recent research further underscores the potential for disrupted neural signaling, as mTOR contributes to both synapse formation and the mechanisms underlying plasticity [12]. Moreover, mTOR exerts control over the expression of diverse ion channels and neurotransmitter receptors, as well as influencing synaptic plasticity, neuronal morphology, and synaptic transmission [18].
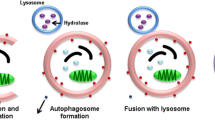
In prevalent causes of hereditary epilepsy such as focal cortical dysplasia (FCD) and tuberous sclerosis complex (TSC), the involvement of the mTOR pathway in epileptogenesis is notably evident. Beyond these conditions, the mTOR pathway plays a role in the development of both inherited and acquired epilepsies, encompassing conditions like Lafora disease (LD), temporal lobe epilepsy, brain injuries, and experimental epileptic states induced by chemically triggered convulsions. Additionally, the mTOR pathway is implicated in systemic lupus erythematosus, an inflammatory disorder that stands as a prominent contributor to epileptic seizures [19]. Genetic mutations impacting various components of the mTOR pathway, such as TSC1 and TSC2, STE20-related kinase adaptor-α (STRADA), phosphatase and tensin homologue (PTEN), AKT isoform predominant in the brain (AKT3), phosphatidylinositol-4,5-bisphosphate 3-kinase-α (PIK3CA), and MTOR itself, result in the hyperactivity of the mTOR pathway. This hyperactivity, in turn, triggers the initiation of epilepsy syndromes [20,21,22,23,24]. Conversely, the inhibition of mTOR can forestall the onset of epilepsy. The modifications in autophagy driven by mTOR are interconnected with the process of epileptogenesis. Following mTOR hyperactivation, autophagy experiences suppression, and the commencement of spontaneous epileptic seizures is associated with the breakdown of autophagy. Autophagy governs diverse processes including axon guidance, synapse development, dendritic spine architecture and pruning, vesicular release, and synaptic plasticity. It also exercises control over the proliferation and migration of both interneuronal and neuronal cortical progenitors.
Evidence points towards mTOR-mediated autophagy failure giving rise to aberrations in the clustering of GABAA receptors at synapses, thereby leading to an imbalance between excitation and inhibition—an essential factor in epileptogenesis. Perturbations with irregular activity of the dopamine system additionally influence the functioning of mTOR-mediated autophagy, contributing to epileptogenesis. This intricate interplay arises from bidirectional communication and shared biochemical pathways, involving cross-reactions between the immune and neurological systems. The connection between mTOR and cell-clearing mechanisms responsible for regulating the metabolic processes of lymphocytes and other immune cells, as well as the antigen-processing capabilities of antigen-presenting cells (APCs) in both the central and peripheral nervous systems, further bolsters this notion. Changes in mTOR-associated cell-clearing processes can disrupt and misalign the communication between the immune and neurological systems [19]. In parallel with its impact on autophagy, epilepsy also exerts effects on the ubiquitin-proteasome system (UPS), a regulatory network governing neuronal excitability, synapse plasticity, and neuro-inflammation/immunity. Disturbances in the UPS within the context of epilepsy are associated with mTOR hyperactivation, akin to the phenomenon observed with autophagy disruption. Recent investigations have elucidated the role of mTOR in orchestrating the convergence of autophagy and UPS morphological pathways, as well as their collective cell-clearing mechanisms. These findings underscore that mTOR-mediated autophagy and UPS activities collectively contribute to epilepsy by influencing brain plasticity and promoting neuroprotection against excitotoxicity. This interplay sheds light on the multifaceted mechanisms through which epilepsy shapes neurological processes and underscores the significance of mTOR regulation in these contexts [19].
Autophagy operates at the interface of the GABA, dopamine, and glutamate systems, contributing to the molecular mechanisms underlying epileptogenesis and the neuronal changes prompted by epileptic convulsions. In instances of autophagy failure, heightened p62 levels conceal the surface presentation of GABAA receptors, leading to a reduction in GABA signaling. Furthermore, the degradation of NMDAR and AMPAR glutamate receptors no longer takes place, resulting in irregular glutamate signaling and an influx of calcium ions. This disarray disrupts the delicate equilibrium between excitatory and inhibitory neurotransmission pivotal to epileptogenesis. On the dopaminergic front, the role of autophagy extends to curtailing dopamine release through the disintegration of synaptic vesicles at the dopamine terminal. In cases where autophagy falters, anomalous dopamine release ensues, accompanied by the stimulation of dopamine D1 receptors. This, in turn, exacerbates autophagy suppression through mTOR hyperactivation. This detrimental cycle leads to the accumulation of damaged cellular components, which combine with glutamate-associated excitotoxicity, ultimately culminating in neuronal demise [19] (Fig. 2).
The role of mTOR pathway in epileptogenesis. Dysmorphic neurons and balloon cells, which lack dendrites or axons, undergo alterations in neurotransmitter receptor subunit expression and uptake site distribution in conditions like TSC, FCD, and hemimegalencephaly (HME). Notably, changes are prominent in GluR, NMDAR, and mGluR subtypes. The direct causation of these alterations—whether they arise from heightened mTOR signaling, tissue cytoarchitecture changes, or adaptations stemming from recurrent seizures—remains uncertain. The accompanying diagram illustrates various locations where dysregulation of mTORC1 (influenced by both phosphoactivation and phosphoinhibition effects) is implicated in human neurological disorders collectively referred to as “mTORopathies,” which encompass epilepsy. Components such as PTEN, STRADA, TSC1/TSC2, and S6K1 might play roles in this context. Experimental animal models involving these proteins also exhibit compromised seizure susceptibility and/or deficits in social and behavioral functions. Rapamycin and other mTOR inhibitors emerge as primary potential therapeutic agents for modulating mTORC1 signaling. These interventions hold promise for regulating the mTOR pathway, offering prospects for addressing the underlying mechanisms of mTOR-related neurological disorders, including epilepsy [21, 25]. Adapted from Crino [21]
The role of apoptotic pathway in epileptic seizure and epilepsy
Beyond its pivotal role in neuronal development, differentiation, and synaptic plasticity [26, 27], glutamate receptor-mediated excitotoxicity is also recognized as a major mechanism contributing to cell death in various disorders of the central nervous system (CNS). These include conditions like brain injury, neurodegenerative diseases, and epilepsy [ Availability of data and materials is not applicable in this study. A Correction to this paper has been published: https://doi.org/10.1186/s42494-024-00157-4 α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid Adenosine triphosphate Blood-brain barrier Cyclic adenosine monophosphate Endothelial selective adhesion molecules Focal cortical dysplasia γ-Amino butyric acid Hyperpolarization-activated cyclic nucleotide-gated High-mobility group box 1 Interleukin-1β converting enzyme Inducible cAMP early repressor Interleukin-1 Interleukin-6 Interleukin-1 receptor type I Junctional adhesion molecules Lafora disease Low-voltage-activated Mammalian target of rapamycin Na-K-2Cl cotransporter isoform 1 N-methyl-D-aspartate N-methyl-D-aspartate receptors Paroxysmal depolarization shifts P-glycoprotein Phosphatidylinositol-4,5-bisphosphate 3-kinase-α Phosphatase and tensin homolog Status epilepticus STE20-related kinase adaptor-α Tumor necrosis factor receptor 1 Tuberous sclerosis complex Stafstrom CE, Carmant L. Seizures and epilepsy: an overview for neuroscientists. Cold Spring Harb Perspect Med. 2015;5:a022426. Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–82. Greenfield LJ. Molecular mechanisms of antiseizure drug activity at GABAA receptors. Seizure. 2013;22(8):589–600. Hui YY, Ahmad N, Makmor-Bakry M. Pathogenesis of epilepsy: challenges in animal models. Iran J Basic Med Sci. 2013;16(11):1119–32. Cai Y, Yang Z. Ferroptosis and its role in epilepsy. Front Cell Neurosci. 2021;15:1–10. Di Maio R. Neuronal mechanisms of epileptogenesis. Front Cell Neurosci. 2014;8:29. Stafstrom CE. The pathophysiology of epileptic seizures: a primer for pediatricians. Pediatr Rev. 1998;19(10):342–51. Wei F, Yan LM, Su T, He N, Lin ZJ, Wang J, et al. Ion channel genes and epilepsy: functional alteration, pathogenic potential, and mechanism of epilepsy. Neurosci Bull. 2017;33:455–77. Jerome EJ. Biomarkers for epileptogenesis and its treatment. Physiol Behav. 2020;176:139–48. Kambli L, Bhatt LK, Oza M, Prabhavalkar K. Novel therapeutic targets for epilepsy intervention. Seizure. 2017;51:27–34. Humairani A, Atmojo BS, Wijayanto I, Hadiyoso S. Fractal based feature extraction method for epileptic seizure detection in long-term EEG recording. J Phys Conf Ser. 2021;1844(1):012019. Staley K. Molecular mechanisms of epilepsy. Nat Neurosci. 2015;18(3):367–72. Rana A, Musto AE. The role of inflammation in the development of epilepsy. J Neuroinflammation. 2018;15(1):1–12. Youn Y, Sung IK, Lee IG. The role of cytokines in seizures: interleukin (IL)-1β. Korean J Pediatr. 2013;56:271–4. Bronisz E, Kurkowska-Jastrzębska I. Matrix Metalloproteinase 9 in Epilepsy: The Role of Neuroinflammation in Seizure Development. Mediators Inflamm. 2016;2016:7369020. Vezzani A. Epilepsy and inflammation in the brain: overview and pathophysiology. Epilepsy Curr. 2014;14(1):3–7. Löscher W, Friedman A. Structural, molecular, and functional alterations of the blood-brain barrier during epileptogenesis and epilepsy: a cause, consequence, or both? Int J Mol Sci. 2020;21(2):591. Abdel-Maksoud MS, El-Gamal MI, Benhalilou DR, Ashraf S, Mohammed SA, Oh CH. Mechanistic/mammalian target of rapamycin: Recent pathological aspects and inhibitors. Med Res Rev. 2019;39:631–64. Limanaqi F, Biagioni F, Busceti CL, Fabrizi C, Frati A, Fornai F. MTOR-related cell-clearing systems in epileptic seizures, an update. Int J Mol Sci. 2020;21:1642. Oluşturulmuş RSP. The effect of rose oil on penicillin-induced epileptiform activity in rats: an electrophysiological study. Konuralp Tıp Derg. 2018;10:360–8. Crino PB. mTOR: a pathogenic signaling pathway in developmental brain malformations. Trends Mol Med. 2011;17(12):734–42. Lee JS, Lim BC, Chae JH, Hwang YS, Seong MW, Park SS, et al. Mutational analysis of paediatric patients with tuberous sclerosis complex in Korea: Genotype and epilepsy. Epileptic Disord. 2014;16:449–55. Wang L, Zhou K, Fu Z, Yu D, Huang H, Zang X, et al. Brain development and Akt signaling: the crossroads of signaling pathway and neurodevelopmental diseases. J Mol Neurosci. 2017;61:379–84. El-megiria N, El-azaba MF, Moustafaa YM. Role of m-TOR pathway in epilepsy: a review and consideration. Records Pharm Biomed Sci. 2022;6(3):136–41. Goldberg EM, Coulter DA. Mechanisms of epileptogenesis: a convergence on neural circuit dysfunction. Nat Rev Neurosci. 2013;14:337–49. Beghi E, Giussani G. Aging and the epidemiology of epilepsy. Neuroendocrinology. 2018;51:216–23. Wang Y, Qin ZH. Molecular and cellular mechanisms of excitotoxic neuronal death. Apoptosis. 2010;15(11):1382–402. **ong L, Sun CF, Zhang J, Gao YB, Wang LF, Zuo HY, et al. Microwave exposure impairs synaptic plasticity in the rat hippocampus and PC12 cells through over-activation of the NMDA receptor signaling pathway. Biomed Environ Sci. 2015;28:13–24. Moujalled D, Strasser A, Liddell JR. Molecular mechanisms of cell death in neurological diseases. Cell Death Differ. 2021;28:2029–44. Srinivasan M, Bayon B, Chopra N, Lahiri DK. Novel nuclear factor-KappaB targeting peptide suppresses β-amyloid induced inflammatory and apoptotic responses in neuronal cells. PLoS One. 2016;11(10):e0160314. Lei L, Yang S, Lu X, Zhang Y, Li T. Research progress on the mechanism of mitochondrial autophagy in cerebral stroke. Front Aging Neurosci. 2021;13:698601. Ginet V, Spiehlmann A, Rummel C, Rudinskiy N, Grishchuk Y, Luthi-Carter R, et al. Involvement of autophagy in hypoxic-excitotoxic neuronal death. Autophagy. 2014;10(5):846–60. Wang Y, Qin ZH. Coordination of autophagy with other cellular activities. Acta Pharmacol Sin. 2013;34:585–94. Zhao X, Liang L, Xu R, Cheng P, Jia P, Bai Y, et al. Revealing the antiepileptic effect of α-asaronol on pentylenetetrazole-induced seizure rats using NMR-based metabolomics. ACS Omega. 2022;7:6322–34. Moya GE, Rivera PD, Dittenhafer-reed KE. Evidence for the role of mitochondrial dna release in the inflammatory response in neurological disorders. Int J Mol Sci. 2021;22:7030. Verma M, Lizama BN, Chu CT. Excitotoxicity, calcium and mitochondria: a triad in synaptic neurodegeneration. Transl Neurodegener. 2022;11(1):3. Cava C, Manna I, Gambardella A, Bertoli G, Castiglioni I. Potential role of miRNAs as theranostic biomarkers of epilepsy. Mol Ther Nucleic Acids. 2018;13:275–90. Lorigados L, Orozco S, Morales L, Estupiñán B, García I, Rocha L. Excitotoxicity and neuronal death in epilepsy. Biotecnol Apl. 2013;30(1):1–8. Avanzini G, Franceschetti S. Mechanisms of epileptogenesis. Treat Epilepsy Third Ed. 2009;14:67–79. Kostrzewa RM. Handbook of neurotoxicity. 2nd ed. Springer Reference; 2014. Koda S, Hu J, Ju X, Sun G, Shao S, Tang RX, et al. The role of glutamate receptors in the regulation of the tumor microenvironment. Front Immunol. 2023;14:1123841. Stafstrom CE, Velíšek L. Developmental epilepsy: From clinical medicine to neurobiological mechanisms. New. Jersey: World Scientific Publishing; 2019. Babtain FA. Impact of a family history of epilepsy on the diagnosis of epilepsy in southern Saudi Arabia. Seizure. 2013;22:542–7. Maljevic S, Reid CA, Petrou S. Models for discovery of targeted therapy in genetic epileptic encephalopathies. J Neurochem. 2017;143:30–48. Pitkänen A, Lukasiuk K, Edward Dudek F, Staley KJ. Epileptogenesis. Cold Spring Harb Perspect Med. 2015;5(10):a022822. Thom M. New perspectives in epilepsy neuropathology. Neuropathol Appl Neurobiol. 2018;44(1):3–5. Althaus AL, Zhang H, Parent JM. Axonal plasticity of age-defined dentate granule cells in a rat model of mesial temporal lobe epilepsy. Neurobiol Dis. 2016;86:187–96. Clynen E, Swijsen A, Raijmakers M, Hoogland G, Rigo JM. Neuropeptides as targets for the development of anticonvulsant drugs. Mol Neurobiol. 2014;50:626–46. Wilson DN, Chung H, Elliott RC, Bremer E, George D, Koh S. Microarray analysis of postictal transcriptional regulation of neuropeptides. Journal of Molecular Neuroscience. 2005;25:85–298. André ES, Bruno-Neto R, Marino-Neto J, do Valle AC, Timo-Iaria C. Spontaneous absence-like activity in Wistar rats: behavioral and electrographic characteristics and the effects of antiepileptic drugs. Acta Sci Biol Sci. 2014;36:231–9. Nadler JV, Tu B, Timofeeva O, Jiao Y, Herzog H. Neuropeptide Y in the recurrent mossy fiber pathway. Peptides. 2007;28(2):357–64. Lagos-Quintana M, Rauhut R, Yalcin A, Meyer J, Lendeckel W, Tuschl T. Identification of tissue-specific microRNAs from mouse. Curr Biol. 2002;12(9):735–9. Roncon P, Soukupovà M, Binaschi A, Falcicchia C, Zucchini S, Ferracin M, et al. MicroRNA profiles in hippocampal granule cells and plasma of rats with pilocarpine-induced epilepsy - comparison with human epileptic samples. Sci Rep. 2015;5:14143. Li MM, Li XM, Zheng XP, Yu JT, Tan L. MicroRNAs dysregulation in epilepsy. Brain Res. 2014;1584:94–104. Wang J, Yu JT, Tan L, Tian Y, Ma J, Tan CC, et al. Genome-wide circulating microRNA expression profiling indicates biomarkers for epilepsy. Sci Rep. 2015;5:9522. Wang X, Sun Y, Tan Z, Che N, Ji A, Luo X, et al. Serum MicroRNA-4521 is a potential biomarker for focal cortical dysplasia with refractory epilepsy. Neurochem Res. 2016;41(4):905–12. Ma Y. The challenge of microRNA as a biomarker of epilepsy. Curr Neuropharmacol. 2017;16(1):37–42. O’Brien J, Hayder H, Zayed Y, Peng C. Overview of microRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol. 2018;9:402. Tiwari D, Peariso K, Gross C. MicroRNA-induced silencing in epilepsy: opportunities and challenges for clinical application. Dev Dyn. 2018;247:94–110. Reschke CR, Silva LFA, Norwood BA, Senthilkumar K, Morris G, Sanz-Rodriguez A, et al. Potent anti-seizure effects of locked nucleic acid antagomirs targeting miR-134 in multiple mouse and rat models of epilepsy. Mol Ther Nucleic Acids. 2017;6:45–56. Alsharafi WA, **ao B, Abuhamed MM, Luo Z. miRNAs: biological and clinical determinants in epilepsy. Front Mol Neurosci. 2015;8:59. An N, Zhao W, Liu Y, Yang X, Chen P. Elevated serum miR-106b and miR-146a in patients with focal and generalized epilepsy. Epilepsy Res. 2016;127:311–6. Acknowledgements is not applicable in this study. There is no financial support for this study. All authors participated in the writing of the manuscript. KTS prepared the figures and conceptualized the content scope of the article. SH wrote, reviewed, and edited the manuscript. DCT proofread and edited the final manuscript. The author(s) read and approved the final manuscript. Ethics approval and consent to participate is not applicable in this study. Consent for publication is not applicable in this study. All authors declare that there is no competing interests. The original version of this article was revised: “Sections "Sodium ion channels" and "Potassium ion channels" were duplicated twice and the duplicated parts have been removed. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Sumadewi, K.T., Harkitasari, S. & Tjandra, D.C. Biomolecular mechanisms of epileptic seizures and epilepsy: a review.
Acta Epileptologica 5, 28 (2023). https://doi.org/10.1186/s42494-023-00137-0 Received: Accepted: Published: DOI: https://doi.org/10.1186/s42494-023-00137-0Availability of data and materials
Change history
12 April 2024
Abbreviations
References
Acknowledgements
Funding
Author information
Authors and Affiliations
Contributions
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Consent for publication
Competing interests
Additional information
Rights and permissions
About this article
Cite this article
Keywords