Abstract
Background
Pheochromocytoma is a rare catecholamine-producing tumour originating from adrenal chromaffin cells. Classic clinical presentation includes headache, diaphoresis and palpitation. Syncope is uncommon and may result from hypotension or arrhythmia. We report a case of neurally mediated syncope in pheochromocytoma associated with cardiac repolarization abnormalities, a unique presentation of the disease.
Case presentation
This case report presents a 28 year-old woman, describing recurrent syncope usually preceded by prodromes such as headache, visual blurring, heart palpitations and psychomotor agitation. Firstly she was diagnosed with anxiety and depression, but there was no improvement of symptoms with psychiatric treatment. Previous Holter revealed long QT interval. Echocardiogram showed normal dimensions, preserved left ventricular function and no valvopathies. The patient was referred for a Head-up tilt test (HUTT) in order to investigate reflex syncope. The electrocardiogram (ECG) exhibited normal sinus rhythm and diffuse cardiac repolarisation abnormalities. HUTT was positive for vasodepressor type neurally mediated syncope and ECG showed U waves after a syncope episode. This electrocardiographic finding motivated further clinical investigation. The patient also described abdominal pain, increased abdominal volume, weight loss and blood pressure instability. Based on clinical history and ventricular repolarisation abnormalities uncovered by HUTT, pheochromocytoma was suspected. Urinary test was positive for catecholamines and the abdominal imaging revelead expansive lesion. She underwent surgery to remove the pheochromocytoma, confirmed by immunohistochemistry.
Conclusions
After surgery she had no recurrency of symptoms, remaining asymptomatic after six years of follow-up, suggesting a cause-effect relationship between neurally mediated syncope and pheochromocytoma.
Similar content being viewed by others
Background
Pheochromocytoma is a rare neuroendocrine tumour that produce catecholamines and originate from the chromaffin cells of the adrenal medulla. It may be caused hereditarily, associated or not with genetic syndromes such as Neurofibromatosis or due to random genetic mutations. The classic clinical presentation includes headache, diaphoresis, palpitation, and psychomotor agitation [1]. Regarding cardiovascular involvement, secondary hypertension is frequent. Syncope is uncommon and usually is a consequence from orthostatic hypotension or arrhythmias. These arrhythmias include sinus tachycardia, atrial fibrillation and ventricular tachycardia [2]. This case report presents a patient with recurrent syncope and cardiac repolarisation abnormalities+ due to pheochromocytoma, a unique presentation of the disease.
Case presentation
Patient information and clinical findings
A 28-year-old woman, reporting more than 20 episodes of syncopes started one year before referral to our service. Events were preceded by visual blurring, nausea and sudden heart palpitations and were not related with body position changes. At the time, she sought medical care several times, receiving a diagnosis of major depressive disorder and generalized anxiety disorder with a prescription for neuroleptics (10 mg of Escitalopram and 2 mg of Clonazepam per day for a few weeks). As the symptoms persisted despite treatment, she was referred for a Head-up Tilt Test (HUTT) by the assistant neurologist to investigate reflex syncope. Medications were discontinued several days before HUTT.
Diagnostic assessment
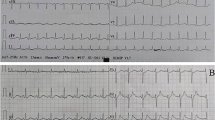
A previous Holter, requested by patient’s assistant neurologist and performed in another healthcare clinic (prior to HUTT execution), described a long QT and QTc interval. Though, the electrocardiogram at rest done just before HUTT showed a normal sinus rhythm (heart rate was 105 bpm), nonspecific ventricular repolarisation abnormalities (Fig. 1A) and normal QT interval of 320 ms (QTc 423 ms). Then, QT prolongation was not confirmed by our assessment. Echocardiogram showed normal dimensions and preserved left ventricular function without structural disease.
A Resting electrocardiogram shows normal sinus rhythm with nonspecific ventricular repolarisation abnormalities and normal QTc (423 ms). B HUTT’s electrocardiographic registry shows junctional rhythm with the presence of U wave. C Junctional rhythm with ventricular ectopy after syncopal event. D Normal sinus rhythm at recovery phase of the follow-up head-up tilt test, six years after tumour removal
The HUTT was performed in the morning, in a calm environment, with an 8-h fast and consisted of a rest phase in a supine position for 10 min followed by the baseline phase with passive inclination of the table with plantar support at 70º (20 min). The sensitisation phase, that normally occurs in the tenth minute, using 1.25 mg of isosorbide dinitrate (if the patient remains asymptomatic in the first phase) was not necessary, because patient presented symptoms during orthostatic stress (between sixth and eighth minute).
In the resting phase, the blood pressure (BP) and heart rate (HR) were 110/70 mmHg and 98 beats per minute (bpm), respectively. After adopting orthostatic posture, there was an immediate and rapid drop in BP and significant increase in HR. It reached 90/50 mmHg in the second minute, 70/50 mmHg in the fourth minute and 60/30 mmHg in the sixth minute. Regarding the behaviour of heart rate, during orthostatic stress, it reached out 137 bpm in the second minute, 151 bpm in the fourth minute and 157 bpm in the sixth minute (Fig. 2A).
Syncope happened around sixth and eighth minute and it was preceded by an increase in heart rate (sinus tachycardia). After assuming a lying position, electrocardiography revealed a junctional rhythm and even more evident abnormalities in ventricular repolarization with the presence of U wave (Fig. 1B) and ventricular ectopy (Fig. 1C) after syncopal event. Thus, HUTT was positive for vasodepressor type neurally mediated syncope.
These electrocardiographic peculiarities unmasked by HUTT motivated further clinical investigation. In a more detailed anamnesis, the patient complained about abdominal pain, increased abdominal volume, unintentional weight loss, sugar craving, blood pressure instability and burning chest pain not associated with exertion. Physical examination showed a palpable abdominal mass.
Based on clinical history and ventricular repolarisation abnormalities uncovered by HUTT, urinary catecholamines, thyroid function and abdominal ultrasound (US) were requested. One month later, the patient underwent laboratory and imaging tests. US showed a large heterogeneous expansive lesion occupying the right flank, with the hypothesis of pheochromocytoma being suspected. Abdominal computed tomography (CT) scan confirmed the US finding, revealing solid-cystic lesion located in the right adrenal gland (Fig. 3A). Urine normetanephrine was 5.693 mcg/24 h (reference < 732), metanephrine 213,8 (reference < 280), adrenaline 13,8 (reference < 27), noradrenaline 1.154,7 (reference < 97) and dopamine 330,4 (reference < 540). Patient was hospitalised for surgery. At admission she did not have any hydro electrolyte disorder. During hospitalization, she presented a syncope episode with undocumented ventricular tachycardia only seen on the cardiac monitor in the intensive care unit. The pre-operative preparation included alfa (12 mg of prazosin) and beta (200 mg of metoprolol) blockade lasting for 37 days prior to surgery. In the subsequent preoperative care, the 15 × 20 cm in diameter tumour was removed (Fig. 3B). The diagnoses of pheochromocytoma were endorsed by immunohistochemistry.
Follow-up and outcomes
After surgery the patient had no recurrency of symptoms, including no other episodes of syncopes, remaining asymptomatic after six years of follow-up, without needing any medication.
At the present time, a second HUTT was performed. It showed regular hemodynamic parameters during orthostatic stress (Fig. 2B) and no signs of neurally mediated syncope. It also exposed normal sinus rhythm and no evidence of ventricular repolarizations irregularities (Fig. 1D).
Discussion and conclusions
Cardiac manifestations related to pheochromocytoma result from exaggerated, continuous or episodic release of catecholamines by the tumour. They are noradrenaline, epinephrine and dopamine.
The main effect of catecholamines on peripheral vessels is vasoconstriction through activation of alpha receptors. This phenomenon of elevated vascular tone results in increased peripheral resistance and higher BP levels, although the relationship between circulating catecholamine levels and BP is not direct [3]. On the other hand, the action of catecholamines on beta-adrenergic receptors may result in increased HR and inotropism when beta 1 receptors in the myocardium are activated, favouring the occurrence of tachycardia. The beta 2 receptors in the peripheral vascular bed activation can lead to vasodilation and, therefore, a reduction in vascular resistance and hypotension.
A prior case report associated the occurrence of syncope caused by postural hypotension to pheochromocytoma [4]. However, until the present time, there are no reports that documented the presence of neurally mediated syncope in pheochromocytoma.
HUTT can play an interesting role in the evaluation of syncopal mechanisms in pheochromocytoma and may help to distinguish neurally mediated syncope from cardiovascular autonomic neuropathy (dysautonomia). In this case report, we considered HUTT was positive for vasodepressor type neurally mediated syncope. Although the drop in BP levels occurred in an early phase of HUTT, which may favour orthostatic hypotension diagnosis, BP falling was rapid and accompanied by increase in HR, condition not seen in neurogenic orthostatic hypotension characterized by inability to increment HR [5].
Some mechanisms can be postulated to explain the hypotension: desensitisation of peripheral vessels to catecholamines; reduced circulatory volume; epinephrine-induced vasodilation with increased epinephrine/noradrenaline secretion rate; and adrenal insufficiency [6]. The first and second mechanisms cited above are the most likely to justify the occurrence of hypotension in the current case.
The desensitisation of blood vessels to catecholamines can be explained by recurrent exposure to these neurotransmitters during adrenergic crises, resulting in down regulation of receptors and shifts in their metabolic pathways. The reduction in circulating volume could occur due to an adaptive response to sustained vasoconstriction [4].
The correlation between arterial hypertension and pheochromocytoma is already well established [7]. It can lead to hypertensive emergencies that along with ventricular arrhythmias, are responsible for significant mortality rates [8]. Around 50 to 70% of patients with pheochromocytoma complain of palpitations and 10% have cardiac arrhythmias [9]. Sinus tachycardia and atrial fibrillation are the most common ones. Ventricular arrhythmias and bradyarrhythmias are less frequent. Prolongation of the QT interval is observed in 16% to 35% of patients that have pheochromocytomas [9, 10]. The mechanism of the prolonged QT is still unclear. Also, it can manifest as sudden cardiac death. These manifestations depend on tumour phenotype, since noradrenergic, adrenergic, dopaminergic or mixed release may happen [8].
Abnormalities in ventricular repolarisation are described in patients presenting with pheochromocytoma. A retrospective study published in 2019 evaluated U wave presence in patients with pheochromocytoma and the occurrence of this finding before and after surgery to remove the tumour. More than 80% of patients had U wave before surgery, but only 37% maintained this abnormality after tumour extraction. Furthermore, an interesting correlation was identified between urinary metanephrine levels, tumour size and U wave amount. Thus, the larger the tumour and the higher the urinary metanephrine levels, the greater the U wave load [9].
The U wave is the last electrical event of the cardiac cycle detectable on the electrocardiogram [9]. Three theories seek to explain the pathophysiological mechanisms of U wave genesis: electro-mechanical stretch; activation of M cells and depolarisation of the papillary muscles delays the onset of the action potential [5].
U wave presence associated with pheochromocytoma could be explained by increases in systemic blood pressure and heart rate. It may overstretch cardiac cells, leading to microcirculation dysfunction and ischemia, which can also delay depolarisation of papillary muscles and adjacent tissues [5, 11]. Nevertheless, in this case report, U waves became more evident just after the syncopal event, while the patient was in a supine position. Also, she was in a bradycardic junctional rhythm at that moment. Thereby, U wave occurrence cannot be explained by standard mechanisms in this case.
Finally, regarding the second HUTT, it is important to emphasize that the patient did not remember how the test worked, given the time that passed between the two HUTT. This, as a matter of fact, excludes confusion bias.
This case reports the occurrence of cardiac repolarization abnormalities and neurally mediated syncope in a patient with pheochromocytoma. There was a resolution of syncope after surgery to remove the tumour confirmed by a second HUTT performed after six years of follow-up, which could indicate a causal relationship between the tumour and the neurally mediated syncope. However, this connection and its mechanisms are not yet fully elucidated, and further studies are needed for a better understanding.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BP:
-
Blood pressure
- CT:
-
Computed tomography
- ECG:
-
Electrocardiogram
- HR:
-
Heart rate
- HUTT:
-
Head-up tilt test
- US:
-
Ultrasound
References
Cerqueira A, Seco T, Costa A, Tavares M, Cotter J. Pheochromocytoma and paraganglioma: a review of diagnosis, management and treatment of rare causes of hypertension. Cureus. 2020;12(5):e7969. https://doi.org/10.7759/cureus.7969.
Ueda T, Oka N, Matsumoto A, Miyazaki H, Ohmura H, Kikuchi T, et al. Pheochromocytoma presenting as recurrent hypotension and syncope. Int Med. 2005;44(3):222–7. https://doi.org/10.2169/internalmedicine.44.222.
Pereira MAA, Souza BF, Freire DS, Lucon AM. Feocromocitoma. Arq Bras Endocrinol Metab. 2004;48(5):751–75. https://doi.org/10.1590/S0004-27302004000500022.
Prejbisz A, Lenders JWM, Eisenhofer G, Januszewicz A. Cardiovascular manifestations of phaeochromocytoma. J Hypertens. 2011;29(11):2049–60. https://doi.org/10.1097/HJH.0b013e32834a4ce9.
Rocha EA, Mehta N, Távora-Mehta MZP, Roncari CF, Cidrão AAL, Neto JE. Dysautonomia: a forgotten condition. Arq Bras Cardiol. 2021;116(4):814–35. https://doi.org/10.36660/abc.20200420.
Nazari MA, Rosenblum JS, Haigney MC, Rosing DR, Pacak K. Pathophysiology and acute management of tachyarrhythmias in pheochromocytoma. JACC Rev Top Week. 2020;76(4):451–64. https://doi.org/10.1016/j.jacc.2020.04.080.
Y-Hassan S, Falhammar H. Cardiovascular manifestations and complications of pheochromocytomas and paragangliomas. J Clin Med. 2020;9(8):2435. https://doi.org/10.3390/jcm9082435.
Di Stolfo G, Mastroianno S, Maggio A, De Luca G, Potenza DR, Salvatori MP, Russo A. Electrical remodeling of ventricular repolarization abnormality after treatment in pheochromocytoma: U wave finding in a retrospective analysis. Biomed Res Int. 2019. https://doi.org/10.1155/2019/2605323.
Kihlgren M, Almqvist C, Amankhani F, Jonasson L, Norman C, Perez M, Ebrahimi A, Gottfridsson C. The U-wave: a remaining enigma of the electrocardiogram. J Electrocardiol. 2023;79:13–20. https://doi.org/10.1016/j.jelectrocard.2023.03.001.
Butt K, Ali S, Sattar Z, Rahman AU, Burt JR. Funny lumps, flaming pheo, and a broken heart: a rare case of pheochromocytoma. Cureus. 2018;10(11):e3646. https://doi.org/10.7759/cureus.3646.
Viskin S, Zeltser D, Antzelevitch C. When U Say, “U waves”, what do u mean? Pacing Clin Electrophysiol. 2004;27(2):145–7. https://doi.org/10.1111/j.1540-8159.2004.00403.x.
Acknowledgements
Not applicable.
Funding
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conception and design of the research were done by EPZC and JEN. Acquisition of data was done by EPZC and JEN and LFMG. Analysis and interpretation of the data were done by EPZC and JEN and RK and MAS. Writing of the manuscript was done by EPZC and JEN. Critical revision of the manuscript for intellectual content was done by RK and MAS and JEN and EPZC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The case was discussed and approved by Hospital Universitário Cassiano Antonio de Moraes da Universidade Federal do Espírito Santo. Number 6.341.545.
Consent for publication
The patient has given its approval to publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cotias, E.P.Z., Neto, J.E., Gomes, L.F.M. et al. Cardiac repolarization abnormalities and neurally mediated syncope: overlooked aspects in the diagnosis of pheochromocytoma. Int J Arrhythm 25, 8 (2024). https://doi.org/10.1186/s42444-024-00116-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-024-00116-7