Abstract
Objective
The objective of this randomized controlled trial (RCT) was to investigate the effectiveness of the lower limb rehabilitation protocol (LLRP) combined with mobile health (mHealth) applications on knee pain, mobility, functional activity and activities of daily living (ADL) among knee osteoarthritis (OA) patients who were overweight and obese.
Methods
This study was a single-blind, RCT conducted at Teaching Bay of Rehmatul-Lil-Alameen Post Graduate Institute of Cardiology between February and November 2020. 114 knee OA patients who were overweight and obese were randomly divided by a computer-generated number into the rehabilitation group with mHealth (RGw-mHealth) to receive LLRP + instructions of daily care (IDC) combined with mHealth intervention, rehabilitation group without mHealth (RGwo-mHealth) to receive LLRP + IDC intervention and control group (CG) to receive IDC intervention. All three groups were also provided leaflets explaining about their intervention. The primary outcome measure was knee pain measured by the Western Ontario and McMaster Universities Osteoarthritis Index score. The secondary outcome measures were mobility measured by the Timed up and go (TUG) test, functional activity measured by the patient-specific functional scale (PSFS), and ADL measured by the Katz Index of independence in ADL scores.
Results
Among the 114 patients who were randomized (mean age, 53 years), 96 (84%) completed the trial. After 3-months of intervention, patients in all three groups had statistically significant knee pain reduction (RGw-mHealth: 2.54; RGwo-mHealth: 1.47; and CG: 0.37) within groups (P < 0.05). Furthermore, patients in the RGw-mHealth and RGwo-mHealth had statistically significant improvement in mobility, functional activity, and ADL within groups (P < 0.05), but no improvement was noted in the CG (p > 0.05). As indicated in the overall analysis of covariance, there were statistically significant differences in the mean knee pain, mobility, functional activity, and ADL changes between groups after 3-months (p < 0.001). The pairwise between-group comparisons (Bonferroni post hoc analysis) of the knee pain, mobility, functional activity, and ADL scores at 3-months revealed that patients in the RGw-mHealth had significantly higher mean change in the knee pain, TUG test, functional activity, and ADL scores compared to patients in the RGwo-mHealth or CG.
Conclusion
Reduction in knee pain, improvement in mobility, functional activity, and ADL were more among patients in the RGw-mHealth compared with the RGwo-mHealth or CG.
Trial registration National Medical Research Registry: NMRR-20-1094-52911. Date of registration: 05–05-2020. URL: https://www.nmrr.gov.my.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) causes a considerable burden in the quality of life and medical treatment of patients [1]. In OA, the knee is the most commonly affected weight-bearing joint with the cardinal symptoms of pain and loss of function [2, 3]. In 2015, knee OA was the most frequent type of OA diagnosed and ranked the thirteenth leading cause of disability globally [4]. Knee OA is a joint destruction and active disease process driven by proinflammatory and biomechanical factors [5]. Knee OA is the most frequent cause of mobility dependency [6] and is highly prevalent in overweight and obese individuals [7].
Patients with knee OA possess 20–40% weaker relative strength of the quadriceps muscles compared to control subjects [8, 9]. The weakness of the quadriceps muscles precedes the onset of knee OA and therefore it could increase the risk of disease development, particularly in women [10]. The Ottawa Panel found evidence to support the use of therapeutic exercises, especially strengthening exercises and general physical activity, combined with manual therapy or separately for the improvement of pain and functional characteristics in OA patients [11]. The American College of Rheumatology Foundation reported a guideline in which physical activity is recommended as a core component of knee OA management [12]. There are different trials of exercise and physical activity-based interventions for the treatment of knee OA. These interventions reported improvement in knee pain, function, and other outcomes among knee OA patients [13]. A current systematic review on non-pharmacological interventions for treating symptoms of knee OA in overweight or obese patients concluded that strengthening exercise played a vital role in relieving knee pain and improving function [14]. Non-pharmacological interventions, primarily strengthening exercise and more recently strengthening exercises of the lower limb rehabilitation protocol (LLRP) in non-weight-bearing positions, are recommended as the first line of treatment among overweight or obese knee OA patients [15].
A current systematic review found that mobile health application (mHealth app) users were more satisfied to manage their health than those of conventional care. The mHealth app users have reported a positive impact on health outcomes and health-related behaviors [16]. Smart phone’s mHealth apps have the potential to play an important role in supporting personal health management [17] and to increase access to healthcare services [18]. A study reported that consistent contact via phone can improve the clinical status of knee OA patients [19]. Effectiveness of rehabilitation combined with mHealth may provide more objective data than the standard rehabilitation approaches we are using today to treat overweight and obese knee OA patients. However, there is a gap in knowledge and a dearth of information regarding whether mHealth can improve the effects of LLRP among overweight and obese knee OA patients. Hence, the current randomized controlled trial (RCT) investigated the effects of LLRP combined with mHealth on knee pain, mobility, functional activity, and activities of daily living (ADL) among overweight and obese knee OA patients. The novelty of the current study could have been mediated by two factors, firstly it was provided as WhatsApp messages and secondly the researchers designed a LLRP to treat overweight and obese knee OA patients. The training sessions of LLRP are the strengthening exercises of the major muscle groups of the lower limbs in non-weight-bearing positions to reduce the mechanical load on the knee.
Methods
Study design and setting
The current study was a single-blind RCT of 3-month duration involving patients with knee OA who were overweight and obese. The study was conducted in the Teaching Bay of Rehmatul-Lil-Alameen Postgraduate Institute of Cardiology (RAIC), Punjab Employees Social Security Institution (PESSI) between February and November 2020. The study was approved by the Ethical Committee of RAIC PESSI with approval number RAIC PESSI/Estt/2020/33 and the trial was registered in the National Medical Research Registry, Malaysia, with ID NMRR-20-1094-52911. Pre-defined questionnaire of inclusion and exclusion criteria was used for screening of the patients. Written informed consent was obtained from all patients before participation in the study.
Sample size
Sample size estimation was performed using the G* Power 3.1.3 software. By assuming the medium effect size f = 0.70, setting α = 0.05, power (1 − B) = 0.90, the total sample size estimated was 84 patients for the three groups. After considering 30% of drop-out or research mortality, the sample size of 114 patients for the three groups was decided (n = 38 per group).
Study patients’ recruitment and selection
The inclusion criteria of the patients were as follows: both males and females, age between 45 and 60 years, overweight and obese, diagnosed with 2-mild or 3-moderate OA according to Kellgren and Lawrence radiographic [20] on one or both knees by an orthopaedic surgeon, symptoms of knee OA for more than 3-months, familiar with WhatsApp applications and residing in the Urban community of Lahore, Pakistan. Exclusion criteria were one or more of the following: diagnosed with flat foot or spinal deformities; history of cardiac or hormonal problems; previous surgery of the knee/s; corticosteroid injection of the knee/s for the last 6-months. Eligibility was determined using a predefined questionnaire of inclusion and exclusion criteria.
Patients were recruited using convenience sampling by active recruitment strategies through urban political and welfare organizations. The list of patients with knee OA in the studied area was obtained from the Welfare Organization upon explaining on the potential benefits of study participation. Two study coordinators prepared the list of potential patients in the recruitment area. After obtaining the list of potential patients, the researcher arranged a meeting with the potential patients through phone call. The meeting was held at the teaching bay of RAIC, PESSI, Lahore, Pakistan, in the presence of a medical specialist. Patients were screened for eligibility to participate in the study. Only patients fulfilling the inclusion and exclusion criteria of the study were invited to participate in this study. The experimental procedures, risks, and benefits associated with the study were explained (verbally and through participants’ information sheets) to all patients prior to providing written informed consent.
Randomization
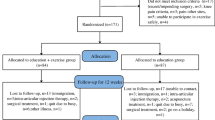
After completing the screening, the selected patients were randomized into three groups; Rehabilitation Group with mHealth (RGw-mHealth), Rehabilitation Group without mHealth (RGwo-mHealth) and the Control Group (CG) (Fig. 1), using a simple random technique (computer generated number). Each group consisted of 38 patients. All patients were also given a diary and asked to record the attendance of completion their interventions based on leaflets.
Study flow diagram: RGw-mHealth = Rehabilitation group with mobile health; RGwo-mHealth = Rehabilitation group without mobile health; CG = Control group; LLRP = Lower limb rehabilitation protocol; IDC = Instructions of daily care; LLRP + IDC-mHealth = Lower limb rehabilitation protocol plus instructions of daily care combined with mobile health
Blinding and allocation
The coordinators collecting data were independent individuals from the trials and were unaware of the group allocation. There were different coordinators at the baseline and post-test evaluation. Individuals performing the statistical analysis were kept blinded by labelling the groups with nonidentifying terms (such as X and Y).
Research procedures
Rehabilitation group with mHealth (RGw-mHealth)
Patients in the RGw-mHealth were prescribed with LLRP + IDC combined with mHealth (LLRP + IDC-mHealth) intervention. The LLRP focused on strengthening exercises for the lower limbs in non-weight bearing sitting or lying positions (Additional file 1) to reduce mechanical pressure on the knee. In the current study, the researcher with the help of several experts in the field of rehabilitation, designed a LLRP (Additional file 1) to be used in the RCT. The LLRP is designed to be a progressive exercise program that begins as a low intensity which gradually increases (frequency, intensity, and duration) to high intensity to ensure that patients could cope with the intervention.
The sequence of the training program started with ten minutes’ warm-up with whole body range of motion (ROM) and dynamic stretching exercises. Patients performed ten repetitions of ROM of each muscle group and 5 repetitions of dynamic stretching of each muscle group as a part of warm-up. A study demonstrated that dynamic stretching is recommended for warm-up to avoid a decrease in strength and performance [21]. When static stretching is used as part of a warm-up immediately prior to exercise, then it causes harm to muscle strength [22]. After warm-up, the patients performed the strengthening exercises of the lower limbs for 3-months (Additional file 1).
Patients were advised to follow the IDC, which included advice on general guidelines of mobility and healthy eating (Table 1). The IDC was translated into Urdu language by two language experts to ensure better patients’ understanding based on a recent pilot study [15]. After completing the strengthening exercises, the patients performed ten minutes cool-down with whole body ROM and static stretching exercises. Patients performed ten repetitions of ROM of each muscle group and 3 repetitions of static stretching of each muscle group as a part of cool-down. A study explained that after two to four repetitions of static stretching, there is no increase in muscle elongation [23].
Additionally, patients in the RGw-mHealth group receive regular reminders to carry out of the LLRP through mHealth in the form of WhatsApp messages. Two text messages per day for three days a week for a period of 3-months were sent to patients in the RGw-mHealth throughout the study period. Patients in the RGw-mHealth received a total 72 text messages. The text messages were sent between 7:00 to 9:00 a.m. and 5:00 to 7:00 p.m. during the days of Wednesday, Friday, and Sunday. A study reported that sending text messages in the morning was to ensure that the patients have enough time to plan and do exercise during the day [24]. In addition, every patient was actively followed by phone at least once a week to ensure that they read the messages and performed the intervention.
Rehabilitation group without mobile health (RGwo-mHealth)
Patients in RGwo-mHealth received LLRP + IDC intervention, but did not receive any reminders to carry out the LLRP exercises. Patients in the RGwo-mHealth were trained on how to perform the LLRP 3-times a week and to adhere to the IDC for 3-months at home. Each training session started with ten minutes of warm-up, forty-five to sixty minutes of strengthening exercises for the lower limbs, and ten minutes of cool down at the end of the training protocol (Additional file 1).
Control group (CG)
Patients in the CG were only advised to follow the IDC intervention for the duration of 3-months (Table 1). No reminders through mHealth application (WhatsApp) were sent to patients in the CG. The feasibility and acceptability of the IDC among knee OA participants have been proved effective in a recent RCT [25].
Measurements and procedures
All patients were assessed at enrolment (baseline) and again at 3-months follow-up. Patients’ assessment includes demographics, exercise adherence, primary and secondary outcome measures of interest. Patients demographic information gathered including age, gender, educational status, and marital status were recorded. The assessment of the patients’ self-reported exercise adherence was collected after 3-months of intervention. A self-reported exercise adherence was measured using a numerical rating scale (NRS) ranging from zero = never performed intervention to 10 = always performed intervention. NRS have also been widely used in other trials [26, 27]. Outcome measures gathered were categorized into primary and secondary outcome measures.
Primary outcome measure
Primary outcome measure was knee pain symptoms assessed using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) that was already adapted and validated. The WOMAC score ranges from 0 to 4 on a Likert-type scale. The researcher used the section on pain of the WOMAC questionnaire. There were five items of WOMAC questionnaire for assessing knee pain. The total scores for the 5 items range from 0 to 20: the higher the score, the worse the pain [28].
Secondary outcome measures
The secondary outcome measures were mobility, functional activity, and ADL. Patients’ mobility was assessed using the Timed Up and Go (TUG) test as described by Podsiadlo and Richardson [29]. The patients were observed and timed while they rose from an armchair, walked three meters, turned, walked back, and sat down again. Assessment was performed in accord with the technique as described in the literature [29].
The Patient-Specific Functional Scale (PSFS) was used for the measurement of functional activity. This is a valid and reliable tool that allows patients to report on their function at baseline and follow-up [30]. The patients were asked to identify up to three difficult activities to perform at enrolment. The patients were then asked to rate each of their identified activities on a numerical scale ranging from 0 = ‘unable to perform an activity’ to 10 = ‘able to perform activities. After 12 weeks of intervention, the patients were again asked to rate their same difficult activities they had identified at baseline. The mean of the scores was used for the analysis of the nominated activities, with higher scores reflecting greater function.
The Katz Index of Independence in ADL was used to assess patients’ ADL. In Katz ADL, six functions were assessed such as feeding, continence, toileting, dressing one self, bathing, and transferring. Each activity has a potential of either zero or one point. One point was used as independence with subheadings, no supervision, direction, or personal assistance. A score of zero is given to indicate that a participant is dependence on subheadings, supervision, direction, personal assistant, or total care in their daily activities. The overall score ranges from zero (patient very dependent) to six (patient fully independent) [31]. In Katz ADL, a total score of 2 or less indicates severe functional impairment, 4 indicates moderate impairment, and a score of 6 indicates full functional independence in ADL [32].
Statistical analysis
The Statistical Package for Social Sciences, version 22, Chicago, IL, was used to analyze the data. Continuous variables were presented as mean (standard deviation [SD]) based on data distribution. The Shapiro–Wilk test was used to assess the normality of all variables. Categorical variables were presented as frequencies (n) and percentages (%). For categorical demographic variables, the One-Way Analysis of Variance (ANOVA) was used to compare for differences between variables. Since all data was normally distributed; the Paired Samples t-test was used to analyze differences between the baseline and 3-months measurements within the groups.
The overall treatment effects on change in clinical outcome measures were estimated using the One Way ANOVA (unadjusted results) and Analyses of Covariance (ANCOVA, adjusted results) for mean changes (95% confidence interval [CI]) from baseline in the continuous outcome data. ANCOVA should be the preferred method for the analysis of pretest–posttest data. The use of ANCOVA in a randomized design is to reduce error variance, because the random assignment of subjects to groups guards against systematic bias [33]. The ANCOVA model included the changes as the dependent variable, with group as a main effect and the baseline scores as an additional covariate. The purpose of using the pretest (baseline) scores as a covariate in ANCOVA with a pretest–posttest design is to reduce the error variance and eliminate systematic bias [33]. The pairwise comparisons between groups were estimated using Bonferroni post hoc analysis. The value of P < 0.05 was considered statistically significant.
Results
There were 114 patients with knee OA enrolled in the 3-months trial. Patients were randomized into LLRP + IDC-mHealth intervention (n = 38), LLRP + IDC intervention (n = 38), and IDC intervention (n = 38). The retention rate in all groups was 84%. The safety coordinator determined that two serious adverse events were unrelated to the study. Both patients were in the RGw-mHealth, one patient had appendix surgery, and the other underwent gallbladder surgery. Patients in the CG had one nonserious adverse event of muscle spasm related to the study.
Figure 1 demonstrates the study flow chart. A total of 18 patients (6 LLRP + IDC-mHealth intervention, 6 LLRP + IDC intervention, and 6 IDC intervention) did not complete the study, resulting in 96 patients (32 LLRP + IDC-mHealth intervention, 32 LLRP + IDC intervention and 32 IDC intervention) included in the analysis of WOMAC pain for knee pain, TUG test for mobility, Katz Index of Independence for ADL and PSFS for functional activity scores. Figure 1 demonstrates the study flow chart including reasons given by patients who did not complete the study.
The patients’ baseline demographics and clinical outcome measures are described in Table 2. No significant differences were observed in the baseline demographic characteristics between the three groups. No statistically significant difference in the Katz Index of Independence for ADL and the PSFS for functional activity scores between the groups. A significant difference in the WOMAC pain and TUG scores was observed at baseline. No significant differences were observed between patients who completed and those who withdrew on baseline demographic and clinical outcome measures (Table 3). Mean and 95% CI of WOMAC pain, TUG test, Katz ADL and PSFS scores at baseline and 3-month follow-up across the three groups are shown in Fig. 2.
Mean and 95% CI of the outcomes measures across the three groups. a mean and 95% CI of WOMAC pain score at baseline and 3-month follow-up, b mean and 95% CI of TUG test score at baseline and 3-month follow-up, c mean and 95% CI of Katz ADL score at baseline and 3-month follow-up, d mean and 95% CI of PSFS score at baseline and 3-month follow-up. WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; TUG = Timed Up and Go; ADL = Activities of daily living; PSFS = Patient specific functional scale; CI = Confidence interval
After participation in 3-months of intervention, a statistically significant improvement compared to baseline was observed for knee pain, mobility, functional activity, and ADL scores (p < 0.05) in the RGw-mHealth, and RGwo-mHealth. In the CG, knee pain score was also significantly improved (p < 0.05) (Table 4).
The mean changes in knee pain scores at 3-months from baseline were 2.54 (95% CI 1.99, 3.09), 1.47 (95% CI 0.93, 2.01) and 0.37 (95% CI − 0.16, 0.90) for patients in the RGw-mHealth, RGwo-mHealth and CG, respectively (Table 5). The pairwise between-group comparisons of WOMAC Pain score at 3-months revealed that patients in the RGw-mHealth demonstrated a statistically significantly higher mean change in WOMAC pain score compared to the patients in the RGwo-mHealth (p = 0.022) and CG (p < 0.001). Additionally, there was also a statistically significant higher mean change in the WOMAC pain score in patients of the RGwo-mHealth compared to the CG (p = 0.013) (Table 6).
The mean changes in TUG test scores at 3-months from baseline were 2.64 s (95% CI 2.26, 3.02 s), 1.34 s (95% CI 0.97, 1.70 s), and 0.29 s (95% CI − 0.06, 0.65 s) for patients in the RGw-mHealth, RGwo-mHealth and CG respectively (Table 5). As indicated by the overall ANCOVA, there was a statistically significant difference in the mean change in the TUG test scores between groups after 3-months interventions (p < 0.001). The pairwise between-group comparisons of the TUG test score at 3-months revealed that patients in the RGw-mHealth demonstrated a significantly higher mean change in the TUG test score compared to the RGwo-mHealth and CG (p < 0.001). Additionally, the mean change in the TUG test score among patients in the RGwo-mHealth was significantly higher compared to the CG (p < 0.001) (Table 6).
The mean changes in functional activity scores were − 2.65 (95% CI − 2.82, − 2.48), − 1.00 (95% CI − 1.17, − 0.83) and − 0.06 (95% CI − 0.22, 0.10) for patients in the RGw-mHealth, RGwo-mHealth and CG respectively (Table 5). The pairwise between-group comparisons of functional activity at 3-months revealed that patients in the RGw-mHealth had significantly higher mean change in the functional activity score relative to both RGwo-mHealth (difference, 1.65 [1.35, 1.94]; p < 0.001) and CG (difference, − 2.59 [− 2.89, − 2.30]; p < 0.001). There was also a statistically significant difference in the mean change in the functional activity scores between the RGwo-mHealth and CG (difference, − 0.94 [− 1.24, − 0.65]; p < 0.001) (Table 6).
Patients in the RGw-mHealth reported the greatest improvement in the ADL score of − 1.13 (95% CI − 1.36, − 0.91) compared to baseline. Improvement in the ADL scores of − 0.51 (95% CI − 0.73, − 0.29) and − 0.12 (95% CI − 0.38, 0.03) was noted in the RGwo-mHealth and CG respectively (Table 5). The pairwise between-group comparisons of the ADL score at 3-months revealed that patients in the RGw-mHealth had a significantly higher mean change in the ADL score compared to both RGwo-mHealth (difference, 0.62 [0.23, 1.01]; p = 0.001) and CG (difference, − 0.94 [− 1.33, − 0.56]; p < 0.001). There was not a statistically significant difference in the mean change in the ADL scores between the RGwo-mHealth and CG (difference, − 0.32 [− 0.71, 0.06]; p = 0.127) (Table 6).
As indicated by the ANOVA, there was a statistically significant difference in self-reported exercise adherence between the groups after 3-months of intervention (p < 0.001). The pairwise between-group comparisons of self-reported exercise adherence at 3-months revealed that patients in the RGw-mHealth had more self-reported adherence to their intervention relative to both patients in the RGwo-mHealth (difference, 0.79 [0.10, 1.47]; p = 0.017) and CG (difference, 3.00 [2.31, 3.68]; p < 0.001) in favour of the RGw-mHealth. There was also a statistically significant difference in self-reported exercise adherence between patients of the RGwo-mHealth and CG (difference, 2.20 [1.52, 2.89]; p < 0.001).
Discussion
To the best of our knowledge, this was the first RCT to investigate the effectiveness of LLRP combined with mHealth on knee pain, mobility, functional activity, and ADL among knee OA patients who were overweight and obese. In this study, patients who were assigned to the RGw-mHealth had significantly less pain, faster mobility, better functional activity, and better ADL scores over a 3-month period than patients in the RGwo-mHealth and CG. The results indicated that patients in the RGw-mHealth who received additional reminders in the form of periodic manual WhatsApp messages showed greater improvements in reducing knee pain and improving mobility, functional activity and ADL than did patients in the RGwo-mHealth or CG. In the current study, the RGw-mHealth produced a clinically relevant reduction in knee pain and improvement in mobility, functional activity, and ADL, and this may explain why clinical improvement of outcome measures occurred. A potential reason why the RGw-mHealth had a significant result is that patient adherence to the LLRP combined with mHealth was good.
Two systematic reviews of randomized controlled trials reported that exercise therapy reduces pain for OA of the knee [34, 35]. In the current study, the pain score was significantly reduced in all three groups (p < 0.05), but a marked reduction in pain score was reported by the patients in the RGw-mHealth (p < 0.001). This may be due to the reminders of using mHealth that were sent to the patients of RGw-mHealth. The reminders of using mHealth stimulated the patients to follow their intervention more efficiently.
A randomized controlled trial reported significantly greater improvement in mobility scores following dietary intervention combined with an exercise program compared with either a dietary or exercise program [36]. Moreover, mobility improvement was also reported following dietary intervention combined with an exercise group of the arthritis, diet, and activity promotion trial [37]. The current study showed that the patients in all three groups reported a reduction in TUG test scores. However, statistically significant improvement in mobility score was only observed in patients of the RGw-mHealth and RGwo-mHealth. The rating of Katz ADL was recommended by the observation of health care professionals [38]. In the current study, a trained health professional recorded the score of Katz ADL. The patients in the RGw-mHealth and RGwo-mHealth reported statistically significant improvement in ADL score than the CG.
A current study demonstrated that a combination of dietary weight loss and exercise intervention was consistently better in improving a combination of performance and functional outcomes among participants with knee OA compared with exercise alone, diet alone, or a control group [37]. Many trials of different physical activity and exercise-based interventions reported improvement of function among knee OA patients [39]. The current study demonstrated a statistically significant improvement in functional activity in patients of RGw-mHealth and RGwo-mHealth, but not in the CG. It is noteworthy that the improvement in functional activity was greater among patients in the RGw-mHealth than the RGwo-mHealth and CG. This may be due to the reminders of using mHealth that were sent to the patients of RGw-mHealth.
Similarly, the results of the current study indicated that patients in the RGw-mHealth reported greater exercise adherence to their interventions compared to patients in the RGwo-mHealth or CG. The patients who got reminders by using mHealth to perform their intervention in the current study reported better adherence than those patients who received their intervention with home exercise programs with an app with remote support [13].
Clinically meaningful results of the outcome measures in the current study could have been mediated by a couple of factors. Apart from serving as mHealth appointment reminders, the LLRP helped to increase the clinical significant results of pain, mobility, functional activity, and ADL.
Based on these findings, this LLRP + IDC-mHealth intervention is expected to be more effective in terms of reducing pain, improving mobility, functional activity, and ADL than any other rehabilitation intervention among knee OA patients who are overweight and obese. In addition, this intervention is easy to use in the home care setting and can also be used for hemiplegia, paraplegia, or wheelchair patients with lower limb weakness.
Study limitations
This study has several limitations. Firstly, the current study was conducted in a single centre to recruit patients. Secondly, patients in the current study were followed up only until 3-months, hence the long-term effects of the interventions cannot be ascertain. Thus, further research across multiple centres and with long-term follow-up are required to confirm the results of LLRP + IDC-mHealth intervention. Thirdly, psychosocial, physical activity, and comorbidity factors may influence the outcomes. Therefore, further research considering these additional factors is required to confirm the findings of the study.
Conclusion
Among knee OA patients who were overweight and obese, after 3-months, patients in the RG-mHealth had less knee pain, better functional activity, faster mobility, and better improvement in ADL scores than those in the RGwo-mHealth and CG. The results of the current study suggest that less knee pain, faster mobility, better functional activity, and ADL score among knee OA patients who were overweight and obese, are augmented better by the implementation of the rehabilitation protocol by using mHealth for rehabilitation or general treatment without mHealth. In this study, the importance of mHealth was revealed in rehabilitation programs for overweight and obese knee OA patients.
Highlights
Knee osteoarthritis (OA) among patients who are overweight or obese has been shown to cause progressive changes in the muscles and articular cartilage of the joint that may not be sufficiently targeted with current rehabilitation approaches.
Using the strengthening exercises of LLRP combined with mHealth may have the potential to reduce pain, improve mobility, functional activity, and ADL among knee OA patients who are overweight or obese. The training sessions of the strength exercises of LLRP combined with mHealth may have the greatest contribution to the body of knowledge internationally because these strengthening exercises are performed in non-weight-bearing sitting or lying positions to reduce the mechanical load on the knee.
Availability of data and materials
Not applicable.
Abbreviations
- RCT:
-
randomized controlled trial
- LLRP:
-
lower limb rehabilitation protocol
- mHealth:
-
mobile health
- Apps:
-
applications
- BMI:
-
body mass index
- OA:
-
osteoarthritis
- RGw-mHealth:
-
rehabilitation group with mobile health
- RGwo-mHealth:
-
rehabilitation group without mobile health
- CG:
-
control group
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
- TUG:
-
timed up and go
- ADL:
-
activities of daily living
- PSFS:
-
Patient Specific Functional Scale
- IDC:
-
instruction of daily care
- ANOVA:
-
one-way analysis of variance
- ANCOVA:
-
analysis of covariance
- NMRR:
-
National Medical Research Registry
- RAIC:
-
Rehmatul-Lil-Alameen Postgraduate Institute of Cardiology
- PESSI:
-
Punjab Employees Social Security Institution
- ROM:
-
range of motion
- CI:
-
confidence interval
- SD:
-
standard deviation
- N:
-
number
- Kg:
-
kilogram
- M:
-
meter
- %:
-
percentage
References
Maetzel A, Li LC, Pencharz J, Tomlinson G, Bombardier C, Community Hypertension and Arthritis Project Study Team. The economic burden associated with osteoarthritis, rheumatoid arthritis, and hypertension: a comparative study. Ann Rheum Dis. 2004;63(4):395–401. https://doi.org/10.1136/ard.2003.006031.
Felson DT. Clinical practice. Osteoarthritis of the knee. N Engl J Med. 2006;354(8):841–8. https://doi.org/10.1056/NEJMcp051726. Erratum in: N Engl J Med. 2006;354(23):2520.
Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. The Lancet. 2005;365(9463):965–73. https://doi.org/10.1016/S0140-6736(05)71086-2.
Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1545–602.
Griffin TM, Guilak F. The role of mechanical loading in the onset and progression of osteoarthritis. Exerc Sport Sci Rev. 2005;33(4):195–200. https://doi.org/10.1097/00003677-200510000-00008.
Helmick CG, Felson DT, Lawrence RC, Gabriel S, Hirsch R, Kwoh CK, National Arthritis Data Workgroup, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 2008;58(1):15–25. https://doi.org/10.1002/art.23177.
Martin KR, Kuh D, Harris TB, Guralnik JM, Coggon D, Wills AK. Body mass index, occupational activity, and leisure-time physical activity: an exploration of risk factors and modifiers for knee osteoarthritis in the 1946 British birth cohort. BMC Musculoskelet Disord. 2013;14:219. https://doi.org/10.1186/1471-2474-14-219.
Jamtvedt G, Dahm KT, Christie A, Moe RH, Haavardsholm E, Holm I, et al. Physical therapy interventions for patients with osteoarthritis of the knee: an overview of systematic reviews. Phys Ther. 2008;88(1):123–36. https://doi.org/10.2522/ptj.20070043.
Rutjes AW, Nüesch E, Sterchi R, Kalichman L, Hendriks E, Osiri M, et al. Transcutaneous electrostimulation for osteoarthritis of the knee. Cochrane Database Syst Rev. 2009;2009(4):CD002823. https://doi.org/10.1002/14651858.CD002823.pub2.
Bennell KL, Hunt MA, Wrigley TV, Lim BW, Hinman RS. Muscle and exercise in the prevention and management of knee osteoarthritis: an internal medicine specialist’s guide. Med Clin N Am. 2009;93(1):161–77. https://doi.org/10.1016/j.mcna.2008.08.006.
Ottawa Panel Members, Ottawa Methods Group, Brosseau L, Wells GA, Tugwell P, Egan M, et al. Ottawa panel evidence-based clinical practice guidelines for therapeutic exercises and manual therapy in the management of osteoarthritis. Phys Ther. 2005;85(9):907–71.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2020;72(2):220–33. https://doi.org/10.1002/art.41142.
Verhagen AP, Ferreira M, Reijneveld-van de Vendel EA, Teirlinck CH, Runhaar J, van Middelkoop M, et al. Do we need another trial on exercise in patients with knee osteoarthritis? No new trials on exercise in knee OA. Osteoarthr Cartil. 2019;27(9):1266–9. https://doi.org/10.1016/j.joca.2019.04.020.
Rafiq MT, Hamid MSA, Hafiz E. Non-pharmacological interventions for treating symptoms of knee osteoarthritis in overweight or obese patients; A review. J Postgrad Med Inst. 2020;34(3):142–8.
Rafiq MT, Hamid MSA, Hafiz E, Amin S. Rehabilitation protocol with or without mobile health in overweight and obese knee osteoarthritis patients-a pilot study. Balneo Res J. 2019;10(4):580–4. https://doi.org/10.12680/balneo.2019.306.
Han M, Lee E. Effectiveness of mobile health application use to improve health behavior changes: a systematic review of randomized controlled trials. Healthc Inform Res. 2018;24(3):207–26. https://doi.org/10.4258/hir.2018.24.3.207.
Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6(4):e40. https://doi.org/10.2196/jmir.6.4.e40.
World Health Organization (WHO). mHealth: new horizons for health through mobile technologies: based on the findings of the second global survey on eHealth. Geneva: WHO; 2011.
Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthr Cartil. 2007;15(9):981–1000. https://doi.org/10.1016/j.joca.2007.06.014.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. https://doi.org/10.1136/ard.16.4.494.
Page P. Current concepts in muscle stretching for exercise and rehabilitation. Int J Sports Phys Ther. 2012;7(1):109–19.
McHugh MP, Nesse M. Effect of stretching on strength loss and pain after eccentric exercise. Med Sci Sports Exerc. 2008;40(3):566–73. https://doi.org/10.1249/MSS.0b013e31815d2f8c.
Taylor DC, Dalton JD Jr, Seaber AV, Garrett WE Jr. Viscoelastic properties of muscle-tendon units. The biomechanical effects of stretching. Am J Sports Med. 1990;18(3):300–9. https://doi.org/10.1177/036354659001800314.
Gell NM, Wadsworth DD. The use of text messaging to promote physical activity in working women: a randomized controlled trial. J Phys Act Health. 2015;12(6):756–63. https://doi.org/10.1123/jpah.2013-0144.
Rafiq MT, Hamid MSA, Hafiz E, et al. Feasibility and acceptability of instructions of daily care in overweight and obese knee osteoarthritis participants. Curr Rheumatol Rev. 2021. https://doi.org/10.2174/1573397117666210727095552.
Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. European Palliative Care Research Collaborative (EPCRC). Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manag. 2011;41(6):1073–93. https://doi.org/10.1016/j.jpainsymman.2010.08.016.
Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. https://doi.org/10.1111/j.1365-2702.2005.01121.x.
Alexandre Tda S, Cordeiro RC, Ramos LR. Factors associated to quality of life in active elderly. Rev Saude Publica. 2009;43(4):613–21. https://doi.org/10.1590/s0034-89102009005000030.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
Horn KK, Jennings S, Richardson G, Van Vliet D, Hefford C, Abbott JH. The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. J Orthop Sports Phys Ther. 2012;42(1):30–42.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–9. https://doi.org/10.1001/jama.1963.03060120024016.
Shelkey M, Wallace M. Katz Index of independence in activities of daily living. J Gerontol Nurs. 1999;25(3):8–9. https://doi.org/10.3928/0098-9134-19990301-05.
Dimitrov DM, Rumrill PD Jr. Pretest–posttest designs and measurement of change. Work. 2003;20(2):159–65.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a cochrane systematic review. Br J Sports Med. 2015;49(24):1554–7. https://doi.org/10.1136/bjsports-2015-095424.
Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66(3):622–36. https://doi.org/10.1002/art.38290.
Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, DeVita P, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263–73. https://doi.org/10.1001/jama.2013.277669.
Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the arthritis, diet, and activity promotion trial. Arthritis Rheum. 2004;50(5):1501–10. https://doi.org/10.1002/art.20256.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. https://doi.org/10.1001/jama.1963.03060120024016.
Lambert TE, Harvey LA, Avdalis C, Chen LW, Jeyalingam S, Pratt CA, et al. An app with remote support achieves better adherence to home exercise programs than paper handouts in people with musculoskeletal conditions: a randomised trial. J Physiother. 2017;63(3):161–7. https://doi.org/10.1016/j.jphys.2017.05.015.
Acknowledgements
We would like to thank Dr. Shariff for his invaluable feedback on an earlier draft for reviewing this article. This RCT was not supported by any grant. The sponsor of RAIC, PESSI had no role in the design of the study; data collection, analysis, and interpretation; review of the manuscript; approval and decision to submit the manuscript for publication.
Funding
This study did not receive financial resources.
Author information
Authors and Affiliations
Contributions
MTR developed the design and protocol of the study, wrote the manuscript and original draft, under the supervision of EH and MSAH. MSAH reviewed the manuscript and corrected the draft twice. EH contributed with the literature search and revision of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the Rehmatul-Lil-Alameen Postgraduate Institute of Cardiology, Punjab Employees Social Security Institution, Lahore, Pakistan (RAIC PESSI/Estt/2020/33) and the trial was registered in the National Medical Research Registry, Malaysia (NMRR-20-1094-52911). All participants gave their informed consent before participation.
Consent for publication
All participants signed the consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Lower limb rehabilitation protocol (LLRP).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rafiq, M.T., Abdul Hamid, M.S. & Hafiz, E. The effect of rehabilitation protocol using mobile health in overweight and obese patients with knee osteoarthritis: a clinical trial. Adv Rheumatol 61, 63 (2021). https://doi.org/10.1186/s42358-021-00221-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-021-00221-4