Abstract
Background
Preoperative airway assessment is essential to predict difficult airway so that adequate planning could be made to secure the airway. Various airway tests have been devised to improve diagnostic accuracy but none of the tests individually have proven to be adequate. Recently, a new airway predictor thyromental height test (TMHT) appears to be a more accurate predictor of difficult laryngoscopy than the existing anatomical measurements. The aim of this study is to evaluate the accuracy of the TMHT and compare it with various screening tests to determine whether TMHT can prove to be a more comprehensive and accurate test for predicting difficult laryngoscopy. Total 150 patients aged > 18 years of either sex with American Society of Anaesthesiologist physical status I—III scheduled for elective surgery under general anaesthesia requiring tracheal intubation were included in this prospective observational study. All patients were subjected to a preoperative airway assessment test including TMHT, modified Mallampati test, upper lip bite test, interincisior gap, thyromental distance and sternomental distance. Intraoperatively direct laryngoscopy was done and the grading of laryngoscopic view was done according to CL.
Results
The preoperative data and CL grading were used to evaluate the accuracy of TMHT and compared the sensitivity, specificity, positive and negative predictive value with other tests.
Twenty six (17.33%) patients had difficult laryngoscopy and 18 patients (12%) required bougie/stylet to facilitate intubation. TMHT had the highest sensitivity (76.92%), specificity (98.38%), PPV (90.90%), NPV (95.31%) and accuracy (94.67%) when compared to other tests.
Conclusions
TMHT is a simple bedside test with higher sensitivity and specificity for predicting difficult laryngoscopy as compared to other screening tests.Future study should be done to define ethinicity, race, age groups and gender specific cut off values of TMHT for accurate validation of prediction in difficult laryngoscopy.
Similar content being viewed by others
Background
In the operation theatre, the rate of difficult and unsuccessful intubation is 1.5–13% and 0.13–0.30%, respectively (Jimson et al. 1995). If airway management is failed, morbidity and mortality is increased in anaesthetized patients. Any difficulty in intubation which has not been anticipated or evaluated can lead to respiratory related adverse outcomes such as varying degree of hypoxia, hypercarbia, and aspiration of vomitus in addition to a rising level of consciousness in a paralyzed patient (McKenna and Wilton 1973).
Therefore, airway assessment tests such as modified mallampati grading (MMPG), sternomental distance (SMD), thyromental distance (TMD), upper lip bite test (ULBT), interincisor gap (IIG), and ratio of height and thyromental distance (RHTMD) have been used to predict difficult intubation but neither single test nor combination of these tests has been validated to predict difficult intubation (Gupta et al. 2005; Badhekha et al. 2016).
From the frequently cited anthropometric measurements, the thyromental height test (TMHT) has been proposed as a promising bed side test, to predict a difficult laryngoscopy. In the supine posture, the TMHT measures the distance between the anterior margin of mentum and the thyroid cartilage (Etezadi et al. 2013). Later, with varied degrees of success, some authors have attempted to assess and validate the prognostic usefulness of TMHT at 50 mm in a variety of ethnic populations (Jain et al. 2017; Panjiar et al. 2019; Rao et al. 2018; Yabuki et al. 2019; Palczynski et al. 2018). Hence, we hypothesize that TMHT is the most accurate method for analyzing difficult laryngoscopy. So we conducted this prospective observational study to evaluate the accuracy of the thyromental height test (TMHT) and compare with various screening tests such as ULBT, TMD, SMD, IIG and MMPG to establish a more reliable and accurate test to predict difficult laryngoscopy.
Methods
After obtaining approval from the Institutional Research Ethics Board, this prospective, observational study was conducted between 2018 to 2019. The study protocol was explained to all the patients and informed consent was taken. Total 150 patients aged > 18 years of either sex with American Society of Anaesthesiologist (ASA) physical status I—III undergoing elective surgery who required tracheal intubation were included in this study. Patients with malformation of the upper airway, pregnant patients, body mass index > 35 kg/m2, emergency surgeries, patients who needed awake intubation, neck mass, and cervical spine injury were excluded from this study.
Preoperative airway evaluation was performed by an anesthesiologist who was not doing laryngoscopy. Demographic data like age, sex, weight, height, BMI, ASA physical status were recorded.
The following airway assessment tests were done preoperatively:
-
MMPG: Patients were asked to open their mouth maximally with tongue protruding without phonation. MMPG classified as CLASS I soft palate, fauces, uvula, anterior and posterior tonsil pillars visible; CLASS II soft palate, fauces, uvula were visible; CLASS III soft palate and base of uvula were visible and CLASS IV only hard palate was visible. MMPG class III and IV were considered as predictor of difficult intubation (Mallampati et al. 1985).
-
ULBT: Upper lip bite test was done by instructing the patient to bite their upper lip with lower incisor to evaluate the range of the mandibular movement and structure of the teeth. The upper lip mucosa can be concealed by a lower incisor in Class I, partially by a lower incisor in Class II, and not at all by a lower incisor in Class III. Class III was considered as predictor of difficult laryngoscopy (Eberhart et al. 2005).
-
IIG: Inter Incisor Gap is the distance between upper and lower incisors at the midline which was measured by instructing the patient to open his mouth to maximum extent and ≤ 3.5 cm was considered as predictor of difficult laryngoscopy.
-
TMD: Thyromental distance was calculated between the bony point of the mentum and the thyroid notch with the mouth closed and was classified as CLASS I if it was less than 6.5 cm, CLASS II if it was between 6.5 cm and 6 cm, and CLASS III if it was greater than 6 cm. A challenging laryngoscopy was one with a TMD of less than 6.5 cm (Krobbuaban et al. 2005).
-
SMD: Sternomental distance, is the distance from the sternal notch to the mentum in centimeters which is measured with the mouth closed and the head extended on the neck. A difficult laryngoscopy was defined as SMD ≤ 13.5 cm (Al Ramadhani et al. 1996).
-
TMHT: The distance between the anterior border of the thyroid cartilage (on the thyroid notch just between the two thyroid laminae) and the anterior border of the mentum (on the mental protuberance of the mandible) was measured with the patient’s mouth closed and lying supine with digital depth gauze (INSIZE Electronic Depth Gage, INSIZE Co Ltd., Suzhou New District China) (Figs. 1 and 2).
Fig. 1
Preoperative vitals were recorded using standard monitors such non-invasive blood pressure, ECG, and pulse oximeter probes. All patients received the intravenous preoperative medications injection glycopyrrolate 4 μg/kg, injection ranitidine 1 mg/kg, injection ondansetron 0.08 mg/kg, and injection fentanyl 2 μg/kg. After pre-oxygenation with 100% O2 for 3 min, injection propofol 2–2.5 mg/kg and injection succinylcholine 1.5 mg/kg intravenously was given for induction. Laryngoscopy was done with Macintosh blade No. 3 or 4 in sniffing position and Cormack and Lehane (CL) view was evaluated by a qualified and experienced anaesthesiologist, who had more than 10 years of experience and was not aware to findings of preoperative airway assessment. CL grading was done as Grade I: Full glottic view, Grade II: Only posterior commissure of glottis is seen, Grade III: Only epiglottis is seen, Grade IV: Epiglottis not seen. CL Grade III or Grade IV was assigned in difficult laryngoscopy group, while CL Grade I or Grade II was assigned in easy laryngoscopy group (Cormack and Lehane 1984). The CL grading were noted by the same anaesthesiologist doing the intubation in all cases.
Adjuvant maneuvers such as backward-upward-rightward pressure (BURP) were given for proper visualization of larynx in difficult laryngoscopy group. Endotracheal intubation was done with appropriate size of tube and confirmed by ETCO2 and bilateral air entry. Stylet, bougie or video-laryngoscope were used for difficult intubation. Number of attempts, failed intubation and complications during intubation were also noted.
Sample size was calculated by considering power of study 90% with confidence level 95%, and incidence of difficult laryngoscopy (10%) (Panjiar et al. 2019). Thus minimum sample of 142 patients were required for the study so we took 150 patients considering dropout cases.
Statistical analysis was performed using SPSS version 16 (SPSS, Chicago, IL, USA). Data were presented as number/percent or mean ± SD. The area under the receiver operating characteristic (ROC) curve for the TMHT was utilised to determine the predictive values of different thyromental height distances and to calculate the optimal cutoff point for TMHT. The validity indices (sensitivity, specificity, accuracy, positive and negative predictive values) and p value were calculated using pre-operative airway assessment data and the findings during intubation for each test. Chi square test was used for statistical comparison for qualitative variables and p < 0.05 was taken to denote significant difference.
Results
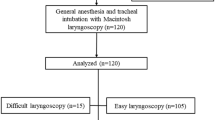
A total 150 patients (male/female: 64/86) undergoing elective surgery under general anaesthesia requiring endotracheal intubation were included in the study (Fig. 3). The demographic profile of all patients are shown in Table 1. Twenty six (17.33%) patients had difficult laryngoscopy and 18 patients (12%) required bougie/stylet to facilitate intubation. The incidence of difficult intubation was 0% in easy laryngoscopy groups (CL grade I and II) but incidence of easy intubation was found 15% in CL grade III and 0% in CL grade IV. BURP was given in 28 patients (18.6%) to proper visualization of larynx and requirement of BURP was increased with increasing CL grade (CL grade 1 = 0%, CL grade 2 = 10.52%, CL grade III = 90%, CL grade IV = 100%). A single attempt intubation was accomplished in 125 patients while two attempt required in 20 patients and three attempt in 5 patients. There was no failed intubations.
Comparison between Cormack-Lehane and preoperative airway predictors of difficult laryngoscopy are shown in Table 2.
TMHT had the highest sensitivity (76.92%), specificity (98.38%), PPV (90.90%), NPV (95.31%) and accuracy (94.67%) among all the tests. Validity indexes for TMHT, MMPG, IIG, ULBT, TMD, SMD to predict difficult laryngoscopy are shown in Table 3. TMD had least sensitivity (26.92%) while SMD had least specificity, PPV, NPV and accuracy.
The ROC of TMHT show the cutoff value for TMHT was 5.15 cm (Fig. 4).
Discussion
Airway assessment is essential to predict difficult intubation so, necessary arrangements to secure the airway could be done. Approximately 30% of the deaths occurred due to hypoxic brain damage secondary to inability to maintain a patent airway (Benumof 1991).
The incidence of difficult laryngoscopy and intubation who required general anaesthesia is 1.3% to 13%, while a higher incidence of up to 20% has been reported (Etezadi et al. 2013; Panjiar et al. 2019; Palczynski et al. 2018). In our study incidence of DVL ( difficult visualization of larynx) was found in 26 (17.3%) patients and no failed intubation was found. BURP was used in 28(18.6%) patients while bougie /styletwas used in 18(12%) patients. Similar incidence of DVL was found by Palczynski et al. (2018) (16.5%) and Allahayari et al. (2008) (18.2%) while Etazadi F et al. (7.3%), Jain N et al. (9.3%), Panjiar P et al. (10%), Rao KV et al. (8.2%), Yabuki S et al. (12%) found lesser incidence of DVL (Etezadi et al. 2013; Jain et al. 2017; Panjiar et al. 2019; Rao et al. 2018; Yabuki et al. 2019). This variation in incidence of DVL can be due to ethnic differences among populations, head position during laryngoscopy, external laryngeal manoeuvre, and varied standards used to define difficult laryngoscopy and intubation.
Although various airway tests have been devised to improve diagnostic accuracy but none of the tests individually have proven to be adequate. However, combining these tests have been proposed to improve their predictive value.
Etezadi et al. 2013 found that TMHT was a more accurate predictor of difficult laryngoscopy, rather than the pre-existing anatomical measurements. The area under ROC curve was used to find out the cut-off point for TMHT which was found to be 5 cm (Etezadi et al. 2013).
The cutoff value for TMHT in our study was found to be 5.15 cm by ROC curve. We performed the statistical analysis of TMHT by taking cutoff value of TMHT as 5 cm which was similar to the study done by Etezadi et al. In our study TMHT at a 5 cm cutoff had the highest sensitivity (76.92%), specificity (98.38%), PPV (90.90%), NPV (95.31%) and accuracy (94.67%) and was found the most accurate airway predictor test when compared with MMPG, IIG, ULBT, TMD and SMD. Similarly the sensitivity, specificity, PPV and NPV was found to be 82.6%, 99.31%, 90.47%, and 98.63% respectively by Etezadi et al. in a study done on 314 Iranian population (Etezadi et al. 2013).
Jain N et al. assessed the TMHT in 345 Indian patients undergoing coronary artery bypass grafting under general anaesthesia and found sensitivity, specificity, PPV, NPV and accuracy of 75%, 97%, 73%, 97% and 97% respectively which was similar to this study (Jain et al. 2017). Similar findings by Panjiar P. et al. revealed that the TMHT is the most accurate and best predictive test with sensitivity, specificity, PPV, NPV and accuracy 78.18%, 93.94%, 58.90%, 97.48%, 92.36% respectively in 550 Indian patients (Panjiar et al. 2019). Panjiar et al. and Jain N et al. also found similar cutoff point for TMHT (5.1 cm and 5.2 cm). Rao KV et al. reported sensitivity, specificity, PPV, NPV and accuracy 84.62%, 98.97%, 88%, 98.63%, 97.7% respectively in 340 Indian patients that also suggest TMHT is the most sensitive and accurate test for predicting difficult laryngoscopy (Rao et al. 2018).
However Yabuki et al. (2019) did a study on 609 Japanese patients and found a cut-off value for TMHT 5.4 cm without BURP and 5.0 cm with BURP. They also found different cut-off value of TMHT for men and women (5.5 cm and 5.6 cm). They found less sensitivity (49.3%), specificity (70.5%), PPV (18.6%), NPV (91.1%) and accuracy (68%) of TMHT at 5 cm cutoff value without BURP so they concluded TMHT to be a poor predictor of DVL when used alone which was contradictory to our results. Palczynski P et al. evaluated the TMHT in 237 patients from Poland and found less sensitivity (70%), specificity (70%), PPV (17%) and NPV (85%) (Palczynski et al. 2018). Selvi et al. also re-evaluated TMHT in Turkish population and found sensitivity (64.8%), specificity (78%), PPV (20.87%), NPV (96.1%) at 4.3 cm cutoff value of TMHT (Selvi et al. 2017). These studies also indicate that TMHT is not a good predictor of difficult laryngoscopy when used alone. This may be due to important factors like racial differences, different incidence of DVL and different cut-off value of TMHT.
MMPG being one of the most widely reported methods used for prediction of difficult laryngoscopy. Although this approach has a low predictive value when used alone, but it can be useful in a multivariate model to predict difficult laryngoscopy. The grading of MMPG is prone to error with phonation, susceptible for incorrect evaluation and interobserver variability. In this study MMPG had sensitivity (46.15%), PPV (66.66%), specificity (95.16%), NPV (89.39%) and good accuracy (86.67%) for prediction of difficult intubation which was less than TMHT. Panjiar et al. (2019) also found similar results while Yabuki et al. (2019) found less sensitivity, specificity and accuracy.
We observed high specificity (98.38%) and NPV (88.40%) of ULBT which predicts easy intubation more confirmatory while sensitivity (38.4%) and positive predictive value (83.33%) was nearly moderate which shows that this test is not much significant in prediction of difficult visualization of larynx. Badheka JP et al. found high sensitivity (96.44%), PPV (92.74%), specificity (82.35%), NPV (91.3%) and concluded ULBT is good predictor for difficult laryngoscopy (Badhekha et al. 2016). ULBT score of predicting difficult laryngoscopy has also some limitations. It is not appropriate for edentulous patients. The craniofacial structure of populations varies by ethnicity. The predictive value of ULBT must be calculated in each population independently for prediction of difficult laryngoscopy (Safavi et al. 2014).
IIG in our study found to be an inadequate predictor of difficult intubation due to low sensitivity but it could be a good predictor for easy laryngoscopy as it had high specificity. Similarly Rao KV et al. also found less sensitivity (69.23%), PPV (17.65%) and high specificity (71.03%), NPV (96.26%) for IIG (Rao et al. 2018).
TMD has been used as a predictor of difficult intubation from earlier days but was found to vary with the patient’s size and body proportion. In our study we observed that TMD has very high specificity (91.13%) and NPV (85.61%), though it had very low sensitivity (26.92%) and low PPV (38.89%). The accuracy of TMD in our study was found to be 80% which is lower as compared to other predictors for difficult intubation. Similarly Panjiar P et al. also found low sensitivity (20%) and low PPV (28.95%) while specificity (94.55%) and NPV (91.41%) for TMD was found to be high (Panjiar et al. 2019). Etezadi F et al. also found low sensitivity (21.73%) and low PPV (8.06%) and high specificity (80.41%) and NPV (92.65%) for TMD (Etezadi et al. 2013).
SMD had very low sensitivity (38.46%) and PPV (25%) but had higher specificity (75.81%) and NPV (85.45%) and the accuracy of SMD was found to be 69.33% which is very low as compared to other predictors of difficult intubation in our study. Similarly other studies (Etezadi et al. 2013; Jain et al. 2017) also found poor sensitivity and PPV while Palczynski P et al. and Basunia SR et al. found high sensitivity (60%, 60% respectively) which was contrary to our study (Palczynski et al. 2018; Basunia et al. 2013).
Limitations of the study: Study group included only patients scheduled for elective surgery with no history of significant difficult intubation. The validity indices of tests were measured only individually and hence combinations of tests were not measured for validity index. Cut-off value of TMHT for males and females was not calculated separately.
Future study should be done to define ethinicity, race, age groups and gender specific cut off values of TMHT for accurate validation of prediction in difficult laryngoscopy. Pilot testing for interobserver variability should also be planned.
Conclusions
TMHT has highest sensitivity, specificity, PPV, NPV and accuracy for predicting difficult laryngoscopy when compared to other tests. TMHT is a simple bedside test that could be used as a single anatomical measure to predict difficult laryngoscopy.
Availability of data and materials
Yes. The datasets generated and/or analysed during the current study are not publicly available, to prevent disclosure of patients identity but are available from the corresponding author on reasonable request.
Abbreviations
- TMHT:
-
Thyromental height test
- MMPG:
-
Modified Mallampati test
- ULBT:
-
Upper lip bite test
- IIG:
-
Inter incisior gap
- TMD:
-
Thyromental distance
- SMD:
-
Sternomental distance
- CL:
-
Cormack-Lehane
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
References
Al Ramadhani S, Mohamed LA, Rocke DA, Gouws E, Ramadhani SA (1996) Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia. Br J Anaesth 77:312–316
Allahyary E, Ghaemei SR, Azemati S (2008) Comparison of six methods for predicting difficult intubation in obstetrics patients. Iran Red Crescent Med J 10(3):197–204
Badhekha JP, Doshi PM, Vyas AM, Kacha NV, Parmar VS (2016) Comparison of upper lip bite test and ratio of height to thyromental distance with other airway assessment tests for predicting difficult endotracheal intubation. Indian J Crit Care Med 20(1):3–8
Basunia SR, Ghosh S, Bhattacharya S, Saha I, Biswas A, Prasad A (2013) Comparison between different tests and their combination for prediction of difficult intubation: an analytical study. Anesth Essays Res 7:105–109
Benumof JL (1991) Management of the difficult airway: with special emphasis on awake tracheal intubation. Anaesthesiology 75:1087–1110
Cormack RS, Lehane J (1984) Difficult tracheal intubation in obstetrics. Anaesthesia 39:1105–1111
Eberhart LH, Arndt C, Cierpka T, Schwanekamp J, Wulf H, Putzke C (2005) The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: an external prospective evaluation. AnesthAnalg 101:284–289
Etezadi F, Ahangari A, Shikri H, Najafi A, Khajavi MR, Daghigh M et al (2013) Thyromental height- a new clinical test for prediction of difficult laryngoscopy. AnesthAnalg 117:1347–1351
Gupta S, Sharma KR, Jain D (2005) Airway assessment: predictors of difficult airway. Indian J Anaesth 49(4):257–262
Jain N, Das S, Kanchi M (2017) Thyromental height test for prediction of difficult laryngoscopy in patients undergoing coronary artery bypass graft surgical procedure. Ann Card Anaesth 20:207–211
Jimson CT, Eric BR, Ayyaz H (1995) Predicting difficult endotracheal intubation in surgical patients scheduled for general anaesthesia: a prospective blind study. AnesthAnalg 81:254–258
Krobbuaban B, Diregpoke S, Kumkeaw S, Tanomsat M (2005) The predictive value of the height ratio and thyromental distance: four predictive tests for difficult laryngoscopy. Anesth Analg 101:1542–1545
Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, Liu PL (1985) A clinical sign to predict difficult tracheal intubation: a prospective study. Can AnaesthSoc J 32:429–434
McKenna T, Wilton TN (1973) Awareness during endotracheal intubation. Anesthesia 28:599–602
Palczynski P, Bialka S, Misiolek H, Copik M, Smelik A, Szarpak L et al (2018) Thyromental height test as a new method for prediction of difficult intubation with double lumen tube. PLoS One 13(9):e0201944
Panjiar P, Kochhar A, Bhat KM, Bhat MA (2019) Comparison of thyromental height test with ratio of height to thyromental distance, thyromental distance, and modified Mallampati test in predicting difficult laryngoscopy: a prospective study. J Anaesthesiol Clin Pharmacol 35:390–395
Rao KV, Dhatchinamoorthi D, Nandhakumar A, Selvarajan N, Akula HR, Thiruvenkatarajan V (2018) Validity of thyromental height test as a predictor of difficult laryngoscopy: a prospective evaluation comparing modified Mallampati score, interincisor gap, thyromental distance, neck circumference, and neck extension. Indian J Anaesth 62:603–608
Safavi M, Honarmand A, Amoushahi M (2014) Prediction of difficult laryngoscopy: extended mallampati score versus the MMT. ULBT and RHTMD Adv Biomed Res 3:133
Selvi O, Kahraman T, Senturk O, Tulgar S, Serifsoy E, Ozer Z (2017) Evaluation of the reliability of preoperative descriptive airway assessment tests in prediction of the Cormack-Lehane score: a prospective randomized clinical study. J ClinAnesth 36:21–26
Yabuki S, Iwaoka S, Murakami M, Miura H (2019) Reliability of the thyromental height test for prediction of difficult visualisation of the larynx: a prospective external validation. Indian J Anaesth 63:270–276
Acknowledgements
Not applicable.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
a. AKB contributed for – concept, Statistical analysis, Manuscript preparation. b. CS contributed for – Definition of intellectual content, Manuscript review. c. SG contributed for- Design of study and manuscript editing. d. AT contributed for- Literature search, clinical studies. e. ABK contributed for- data analysis. f. VC contributed for- data acquisition. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was done after taking ethical approval from Institutional Research Ethics Board geetanjali medical college and hospital, Udaipur (GU/HREC/EC/2017/1499) and consent from participants.
Consent for publication
Consent for publication was taken from all participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bhiwal, A.K., Sharma, C., Tripathi, A. et al. Evaluation of thyromental height test as a single anatomical measure for prediction of difficult laryngoscopy: a prospective observational study. Ain-Shams J Anesthesiol 15, 75 (2023). https://doi.org/10.1186/s42077-023-00372-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-023-00372-0