Abstract
Background
End-stage renal disease has a high prevalence worldwide. Quiet often, we come across patients with end-stage renal disease surviving on haemodialysis or peritoneal dialysis who need surgery. The management of such patients is a challenging task for the anaesthesiologist.
Case presentation
A patient suffering from end-stage renal disease on peritoneal dialysis was posted for removal of supratentorial space occupying lesion in our operation theatre. We describe the successful management of this case by the technique of awake craniotomy.
Conclusion
Awake craniotomy can be a safe alternative for high-risk patients undergoing craniotomy for brain tumours.
Similar content being viewed by others
Background
Excision of brain tumours by awake craniotomy is a well-established procedure performed for mainly neurosurgical indications. There are several benefits of this technique over craniotomy performed under general anaesthesia (Zhang and Gelb 2018; Gupta et al. 2001). Patients with renal dysfunction when administered general anaesthesia are at high risk for perioperative complications. Therefore, awake craniotomy can be considered as an anaesthetic technique for neurosurgery in such patients who are otherwise at high risk for receiving general anaesthesia.
Case presentation
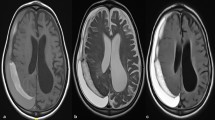
Our patient was a 34-year-old female, who presented with left-sided weakness for the last 4 months and absence seizure for a year. She was a known case of hypertension and end-stage renal disease with anuria and on continuous peritoneal dialysis for 3 years. Her regular medications included amlodipine 5 mg once daily, clonidine 100mcg twice daily, elemental iron 30 mg once daily and injection erythropoietin 4000 U SC twice weekly. MRI showed a supratentorial space occupying lesion on the right parietal region (Fig. 1). Investigations revealed a Hb of 7.3 gm%, creatinine of 13.28 mg%, potassium of 3.5 meq/L and sodium of 133 mg/dl with a normal echocardiogram. After extensive discussion with the neurosurgical team and the patient, it was decided to proceed with navigation guided excision of the lesion under awake craniotomy.
Following a detailed explanation about the risks and benefits of the technique, written informed consent was taken. She was 5 feet 3 inches tall weighing 52 kg, without any obvious airway abnormality. Neurologically, she was fully conscious and oriented with mild left-sided weakness. Peritoneal dialysis was done the night before operation, and she was administered all the regular medications. In the operation theatre, after attaching all standard monitors (ECG, SpO2, NIBP, respiration), large bore intravenous cannulation was done, and the arterial line was secured under local anaesthesia. The patient was covered with warming blanket, and oxygen @ 2 L/min was given through nasal cannula. Scalp nerve block was performed bilaterally with 2 ml of 0.25% bupivacaine being administered for each nerve along with infiltration at the pin insertion sites, the total volume of bupivacaine not exceeding 2 mg/kg. The surgical team was asked to proceed after checking the adequacy of the block. Intermittent boluses of 1–2 ml of 1% propofol were administered during the fixation of Mayfield head clamp and drilling of the bone. No further sedation was required for the rest of the surgical period which lasted for 3 h.
Paracetamol (1gm), levetiracetam (500 mg) and ondansetron 8 mg were administered intravenously along with 0.9% saline 200 ml and 1 unit packed red blood cell to compensate for blood loss. No additional brain relaxation techniques either pharmacological or non-pharmacological were required. The vitals were well maintained throughout the operative procedure and so was the neurological status. The patient complained of mild headache for the first time 2 h after the completion of surgery for which she was put on intravenous paracetamol (1 gm) every 8 h for 1 day and converted to oral paracetamol over the next 2 days. The postoperative imaging showed complete excision of the intracranial space occupying lesion (Fig. 2).
In the postoperative period, the patient had smooth recovery with improvement of left-sided weakness and was satisfied with her perioperative experience. She underwent peritoneal dialysis at bedside after 4 h. She had an uneventful postoperative recovery and discharged after few days.
Discussion
Patients with end-stage renal disease have specific pathophysiology and therefore present unique challenges to anaesthesiologists and surgeons. End-stage renal disease causes multi system dysfunction. The effects are seen in all organ systems and are mediated by accumulation of toxic metabolite products and endocrine dysfunction. Haemodialysis and peritoneal dialysis are renal replacement therapies to remove the metabolic wastes but may themselves cause physiological disturbances. General anaesthesia in such patients has its own challenges like cardiovascular instability and unpredictable drug effects (Verma et al. 2015).
Awake craniotomy is a technique where the patient remains awake during whole or part of the surgery. It has mainly been used by neurosurgeons for surgery on eloquent areas of brain. The awake approach has increasingly being used due to advantage of better neurological and perioperative outcomes like better analgesia, decreased postoperative nausea and vomiting and shorter hospital stay. Medications like propofol, dexmedetomidine and remifentanil are used for conscious sedation. Anaesthetic regimens range from light to moderate sedation, with or without regional anaesthesia using Scalp nerve blocks. In all regimens, patients are awake and able to speak and or move during the monitoring phase. Conducting awake craniotomy is very challenging, so it is very important that the anaesthesiologists be well conversant with this technique (Rath et al. 2014).
This technique is particularly advantageous for conditions as seen in our patient who was at high risk for general anaesthesia. By adapting this method, we could perform neurosurgery without subjecting an end-stage renal disease patient to the side effects of multiple anaesthetic drugs. Since the patient was awake the whole time except during fixation of the head clamp and drilling of the bone, additional neuromonitoring or brain map** techniques were not considered which was also beneficial from the point of view of procedural cost. Similarly, since brain relaxation was not required as the patient was awake, we could avoid the use of mannitol which otherwise could have been highly detrimental for patients with end-stage renal disease (Lin et al. 2015).
There are very few reports on the use of awake technique during neurosurgery for non-neurosurgical indications. Lingzhong Meng et al. (Meng et al. 2015) reported the use of awake craniotomy in a patient with dilated cardiomyopathy and low-output cardiac failure posted for low-grade oligodendroglioma resection.
Our patient had a brain tumour which needed urgent excision because of the progressive neurodeficit and repeated seizures. She was not able to undergo neurosurgery because anaesthesia and neurosurgical team considered her to be at too high risk for receiving general anaesthesia. The use of awake craniotomy in her case proved to be a novel application of a well-known technique which benefited the patient without subjecting her to undue risk.
Conclusions
Hence, we advocate the use of awake craniotomy as an alternative and safer approach of anaesthetic technique in such conditions. This case highlights an uncommon indication of the awake technique.
Availability of data and materials
Not applicable
Abbreviations
- ECG:
-
Electrocardiogram
- SpO2 :
-
Pulse oximetry
- NIBP:
-
Non-invasive blood pressure
References
Gupta A, Singh VP, Dash HH (2001) A review of awake craniotomy: waking up to an old technique. Neurosci Today 5:52–55
Lin SY, Tang SC, Tsai LK, Yeh SJ, Shen LJ, Wu FL et al (2015) Incidence and risk factors for acute kidney injury following mannitol infusion in patients with acute stroke: a retrospective cohort study. Medicine (Baltimore) 94(47):e2032. https://doi.org/10.1097/MD.0000000000002032
Meng L, Weston SD, Chang EF, Gelb AW (2015) Awake craniotomy in a patient with ejection fraction of 10%: considerations of cerebrovascular and cardiovascular physiology. J Clin Anesth 27(3):256–261. https://doi.org/10.1016/j.jclinane.2015.01.004
Rath GP, Mahajan C, Bithal PK (2014) Anaesthesia for awake craniotomy. J Neuroanaesthesiol Crit Care 1(03):173–177. https://doi.org/10.4103/2348-0548.139098
Verma VK, Kumar A, Bhardwaj G, Kumar S, Kumar M, Chandan KK (2015) Anaesthesia for chronic renal disease and renal transplant: an update. J of vol Med Dent Sci 4(19):3346–3364. https://doi.org/10.14260/jemds/2015/482
Zhang K, Gelb AW (2018) Awake craniotomy: indications, benefits, and techniques. Rev Colomb Anestesiol 46:46–51. https://doi.org/10.1097/CJ9.0000000000000045
Acknowledgements
Not applicable
Funding
None
Author information
Authors and Affiliations
Contributions
DR and SG are the primary authors (wrote most of the manuscript or drafted the manuscript), DS provided revisions to the scientific content of the manuscript, and IG is the advisor or provided grammatical revisions to the manuscript. All authors read and approved the final case report (manuscript).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for the publication of this case report was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roy, D., Guha, S., Shah, D. et al. Excision of brain tumour in a peritoneal dialysis dependent patient by awake craniotomy: a case report. Ain-Shams J Anesthesiol 13, 65 (2021). https://doi.org/10.1186/s42077-021-00186-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-021-00186-y