Abstract
Past literatures have reported that changes in serum vitamin D levels are related to cognitive dysfunctions, such as dementia, including Alzheimer’s disease (AD). However, these past studies vary in results on whether vitamin D levels correlated with the development of AD. This meta-analysis aimed to assess the associations between low vitamin D serum levels as risk factor of AD based on the latest evidence. We systematically searched Pubmed and additional references for relevant articles according to PRISMA guidelines from the beginning up to December 2022. The risk estimate of AD was determined using a pooled hazard ratio (HR) with 95% confidence intervals (CIs). five prospective trials and one cross-sectional study were analyzed. The meta-analysis showed that patients with low vitamin D serum levels (< 25 ng/ml) had an increased risk of develo** AD compared to patients with normal vitamin D levels (≥ 25 ng/ml) (HR: 1.59, 95% CI: 1.09, 2.33, I2=77%). Further research is required to provide evidence on whether maintaining sufficient vitamin D serum levels may lower the risk of AD.
Similar content being viewed by others
Introduction
Dementia is a term to describe a clinical syndrome of acquired, progressive decline in cognitive functions in the loss of one or more cognitive abilities caused by brain disease or injury, severe enough to reduce a person's ability to perform daily activities [1]. Alzheimer's disease is a subtype of dementia, characterized by the formation of neuritic plaques and neurofibrillary tangles. The extracellular deposition of Aβ peptide, known as amyloid plaques. The neurofibrillary tangle consists of abnormal intracellular accumulations of phosphorylated tau protein within the perikaryal cytoplasm of certain neurons [2]. AD is the most common type of dementia, accounting for at least 75% of dementia cases in the elderly population. Approximately, there are around 50 million AD patients in the world and expected to increase by threefold in 2050 [2]. AD puts a heavy burden on healthcare systems around the world, costing more than $80 billion each year [3].
A past study by Perez-Lopez and colleagues reported the crucial role of vitamin D in maintaining cognitive function [4] another study also suggests the vitamin D receptors present in the brain regions responsible for cognitive functions and memory development [5]. The roles of Vitamin D in neurotrophy, neurotransmission, neuroprotection, and neuroplasticity may explain vitamin D deficiency involvement in the progression of AD [6]. Several past studies have reported the relationship between vitamin D deficiency and cognitive decline. An updated meta-analysis by Chai and colleagues reported significant associations between vitamin D deficiency and AD, with severe vitamin D deficiency having the strongest association [7] other meta-analyses also reported that Plasma or serum 25-hydroxyvitamin D concentration related to the risk of AD in inverse association [8]. The meta-analysis of the prospective cohort studies of Vitamin D concentration and the risk of AD reported that serum vitamin D deficiency or insufficiency was not statistically significant and associated with the risk of AD ([9]); this finding showed the inconsistent result between past meta-analysis. Thus, we are conducting an updated meta-analysis of vitamin D and AD association.
Methods
This study followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [10].
Literature searching and selection method
Initially, two authors independently filtered the databases of the selected studies on PubMed up to December 2022, using specific keywords: “vitamin D” AND “Alzheimer.” We used the following inclusion criteria to select eligible studies that assess the relationship between low vitamin D serum levels and Alzheimer’s disease: (1) Observational studies that evaluated the association between low vitamin D serum levels at baseline and subjects with AD; (2) studies that reported hazard ratio (HR) alongside 95% confidence intervals (CIs) as risk estimates. The literature search was particularly for English language studies only. We excluded the following studies: (i) non-original articles (narratives, systematic review, meta-analyses, abstracts, comments, or editorials); (ii) case report/ series; (iii) studies assessing other conditions not within our scope; (iv) incomplete data. The main outcome was the risk estimates of low vitamin D serum levels as risk factor of develo** AD.
Data extraction and quality assessment
two independent authors read and inspected the titles and abstract according to the inclusion criteria—next, these authors examined a full-text review. If there were a lack of agreement between the two authors, the primary author would settle the disagreement and make a final judgment. Articles that matched the inclusion criteria were selected, and additional studies were retrieved according to the references of the articles collected.
We collected and summarized the subsequent data: Main author(s), publication years, study design, nation of origin, serum 25(OH)D levels, follow-up duration, and statistical adjustment. The Oxford Center for Evidence-Based Medicine (OCEBM) scale assessed each study's ratings. The scale categorized each study with ratings ranging from 1 to 5, with 1 meaning high-quality studies such as clinical trials and 5 representing case series/reports [11].
Statistical analysis
We conducted the analyses using Review Manager (RevMan) statistic software (version 5.3). The hazard ratio (HR) and 95% confidence interval (CI) were analyzed as effect size. We also analyzed I2 statistics to assess heterogeneity between studies. I2 of more than 50% was considered high heterogeneity. A Fixed-effects model was performed when there was no heterogeneity between studies. On the contrary, A random effects model will be used when data are considered heterogeneous. P-values of less than 0.05 (P ≤ 0.05) were statistically significant [12, 13].
Results
Study characteristics
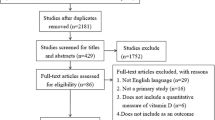
The initial search strategy identified 562 articles. After removing copies, followed by abstract screening, 24 full-text articles were evaluated for their eligibility. The final review included six articles [14,15,16,17,18,19] of five prospective studies and one cross-sectional. Figure 1. displays the PRISMA flow chart.
This process resulted in the selection of 6 studies that evaluated the relationship between vitamin D deficiency and AD, involving 10,884 participants for the meta-analysis. Of the included studies, author(s), publication years, study design, nation of origin, serum 25(OH)D levels, follow-up duration, statistical adjustment, and study ratings. Overall, most of the studies had high-quality ratings (Table 1). All selected studies observed patients with low vitamin D serum levels (< 25 ng/ml) as a risk factor of AD.
Low vitamin D serum levels and risk of AD
A meta-analysis with random effects model was conducted to summarize the estimated risk of AD in patients with low levels of serum vitamin D. The analysis showed that patients with low levels of vitamin D (< 25 ng/ml) had a greater risk of develo** AD compared with those who had normal serum vitamin D levels (HR: 1.59, 95% CI: 1.09, 2.33, I2 = 77%, Fig. 2). The I2 value was 77% indicating heterogeneity between studies.
Discussion
This meta-analysis provided additional evidence of low vitamin D levels and the risk of Alzheimer's disease. A total of 6 studies were included in this study, involving 10,884 participants. The analysis showed that patients with vitamin D deficiency (< 25 ng/ml) had a higher risk of AD compared to patients with adequate vitamin D supply (≥ 25 ng/ml). A previous meta-analysis [8] in 2018 reported the inverse association between 25-hydroxyvitamin D concentration to the risk of dementia. This study included Ten cohort studies with more than 20.000 participants. A year later, a meta-analysis involving twelve prospective cohort studies and four cross-sectional studies reported the same results as the previous meta-analysis. This meta-analysis reported a significant association between Vitamin D deficiency and dementia, with severe deficiency (< 10 ng/ml) having the strongest association compared to moderate vitamin D deficiency (10–20 ng/ml). [7] within the same year, other meta-analyses reported different results. Meta-analyses by Yang K and colleagues reported that the relation between vitamin D deficiency and insufficiency with the risk of AD was not statistically significant. This study involved six prospective cohort studies with more than 1000 AD cases [9].
The pathomechanism of AD may cause by two types of neuropathology changes. The first neuropathology change is a positive lesion due to the accumulation of neurofibrillary tangles, amyloid plaques, and other deposits in the AD patient's brain. The second neuropathology change is due to the loss of neuropil, neural and synaptic. Besides, neurodegeneration can cause by factors such as oxidative stress and neuroinflammation [2].
Several studies have reported vitamin D's potential benefit and relationship with AD. Vitamin D may affect the first neuropathology change by promoting the clearing of amyloid plaques, as reported in animal and human studies [20, 21]. Vitamin D also prevents cognitive dysfunction via its roles in neuroprotection, neurotrophy, neurotransmission, and neuroplasticity, although its mechanism is still unclear [6]. Vitamin D also showed the potential to prevent neuroinflammation by inhibiting the production of TNF-a and IL 6 in in-vitro studies [22].
This study has limitations. Firstly, this study included one cross-sectional study, thus increasing the possibility of bias. Secondly, our study focused mainly on the relationship between Alzheimer's disease risk and low vitamin D levels. It was unclear whether the vitamin D level had changed in further follow-up. Lastly, the patients involved in this study are mainly from Europe and America. Thus this study may not be applied to the world population.
Conclusion
This meta-analysis provided evidence of the relationship between low vitamin D levels with the risk of AD. The random effects model analysis showed that low vitamin D levels (< 25 ng/ml) are a risk factor for develo** AD. Maintaining normal vitamin D levels may lower the risk of AD.
Availability of data and materials
Not applicable.
Abbreviations
- AD:
-
Alzheimer’s disease
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- I 2 :
-
Heterogeneity statistic
- IL-6:
-
Interleukin-6
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- TNF-a:
-
Tumor necrosis factor alpha
References
Arvanitakis Z, Shah RC, Bennett DA. Diagnosis and management of dementia: review. JAMA. 2019;322(16):1589–99. https://doi.org/10.1001/jama.2019.4782.
Breijyeh Z, Karaman R. Comprehensive review on Alzheimer’s disease: causes and treatment. Molecules. 2020;25(24):5789. https://doi.org/10.3390/molecules25245789.
Kelley AS, McGarry K, Gorges R, Skinner JS. The burden of health care costs for patients with dementia in the last 5 years of life. Ann Intern Med. 2015;163(10):729–36. https://doi.org/10.7326/M15-0381.
Pérez-López FR, Chedraui P, Fernández-Alonso AM. Vitamin D and aging: beyond calcium and bone metabolism. Maturitas. 2011;69(1):27–36.
Annweiler C, Schott AM, Berrut G, Chauviré V, le Gall D, Inzitari M, et al. Vitamin D and ageing: neurological issues. Neuropsychobiology. 2010;62(3):139–50.
Anjum I, Jaffery SS, Fayyaz M, Samoo Z, Anjum S. The role of vitamin D in brain health: a mini literature review. Cureus. 2018. https://doi.org/10.7759/cureus.2960.
Chai B, Gao F, Wu R, Dong T, Gu C, Lin Q, et al. Vitamin D deficiency as a risk factor for dementia and Alzheimer’s disease: an updated meta-analysis. BMC Neurol. 2019;19(1):284.
Chen H, Xue W, Li J, et al. 25-Hydroxyvitamin D levels and the risk of dementia and Alzheimer’s disease: a dose-response meta-analysis. Front Aging Neurosci. 2018;10:368.
Yang K, Chen J, Li X, Zhou Y. Vitamin D concentration and risk of Alzheimer disease: a meta-analysis of prospective cohort studies. Medicine (Baltimore). 2019;98(35):e16804. https://doi.org/10.1097/MD.0000000000016804.
Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. https://doi.org/10.1136/bmj.g7647.
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, et al. The 2011 Oxford CEBM levels of evidence. Oxford Centre for Evidence-Based Medicine; 2011.
Higgins JPT, Green S. Medians and interquartile ranges. In: Higgins JPT, Green S, editors. Co-chrane handbook for systematic reviews of interventions 5.1. Oxford: Cochrane Collaboration; 2011.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Afzal S, Bojesen SE, Nordestgaard BG. Reduced 25-hydroxyvitamin D and risk of Alzheimer’s disease and vascular dementia. Alzheimers Dement. 2014;10(3):296–302. https://doi.org/10.1016/j.jalz.2013.05.1765.
Littlejohns TJ, Henley WE, Lang IA, Annweiler C, Beauchet O, Chaves PH, et al. Vitamin D and the risk of dementia and Alzheimer disease. Neurology. 2014;83(10):920–8. https://doi.org/10.1212/WNL.0000000000000755.
Karakis I, Pase MP, Beiser A, Booth SL, Jacques PF, Rogers G, et al. Association of serum vitamin D with the risk of incident dementia and subclinical indices of brain aging: the Framingham Heart Study. J Alzheimers Dis. 2016;51(2):451–61. https://doi.org/10.3233/JAD-150991.
Feart C, Helmer C, Merle B, Herrmann FR, Annweiler C, Dartigues JF, et al. 2017 Associations of lower vitamin D concentrations with cognitive decline and long-term risk of dementia and Alzheimer’s disease in older adults. Alzheimers Dement. 2017;13(11):1207–16. https://doi.org/10.1016/j.jalz.2017.03.003.
Licher S, de Bruijn RFAG, Wolters FJ, Zillikens MC, Ikram MA, Ikram MK. Vitamin D and the risk of dementia: the Rotterdam study. J Alzheimers Dis. 2017;60(3):989–97. https://doi.org/10.3233/JAD-170407.
Aguilar-Navarro SG, Mimenza-Alvarado AJ, Jiménez-Castillo GA, Bracho-Vela LA, Yeverino-Castro SG, Ávila-Funes JA. Association of vitamin D with mild cognitive impairment and alzheimer’s dementia in older mexican adults. Rev Invest Clin. 2019;71(6):381–6. https://doi.org/10.24875/RIC.19003079.
Briones TL, Darwish H. Vitamin D mitigates age-related cognitive decline through the modulation of pro-inflammatory state and decrease in amyloid burden. J Neuroinflammation. 2012;9:244. https://doi.org/10.1186/1742-2094-9-244.
Masoumi A, Goldenson B, Ghirmai S, Avagyan H, Zaghi J, Abel K, et al. 2009 1alpha,25-dihydroxyvitamin D3 interacts with curcuminoids to stimulate amyloid-beta clearance by macrophages of Alzheimer’s disease patients. J Alzheimers Dis. 2009;17(3):703–17. https://doi.org/10.3233/JAD-2009-1080.
Lefebvre d’Hellencourt C, Montero-Menei CN, Bernard R, Couez D. Vitamin D3 inhibits proinflammatory cytokines and nitric oxide production by the EOC13 microglial cell line. J Neurosci Res. 2003;71(4):575–82. https://doi.org/10.1002/jnr.10491.
Acknowledgements
Not applicable.
Funding
This study is personally funded by the authors.
Author information
Authors and Affiliations
Contributions
RP, TH, VOW: conceptualization. VOW, RBB: methodology and formal analysis: VOW, RBB: Original draft the manuscript. RP, TH: visualization. RP, TH: validation, review and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pinzon, R.T., Handayani, T., Wijaya, V.O. et al. Low vitamin D serum levels as risk factor of Alzheimer’s disease: a systematic review and meta-analysis. Egypt J Neurol Psychiatry Neurosurg 59, 88 (2023). https://doi.org/10.1186/s41983-023-00676-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00676-w





