Abstract
Background
Interleg systolic blood pressure difference (ILSBPD) is associated with peripheral artery disease, but the relationship between ILSBPD and apparent peripheral neuropathy in diabetic patients remains unclear. We explored the relationship between ILSBPD and apparent peripheral neuropathy and examined the possible effect modifiers in US adults with diabetes.
Methods
One thousand and fifty-one diabetic participants were included in the study with complete data on systolic blood pressure of the lower extremities and Semmes–Weinstein 10-g monofilament testing from the 1999–2004 National Health and Nutritional Examination Surveys. Systolic blood pressure in the lower extremities was measured using an oscillometric blood pressure device with the patient in the supine position. Apparent peripheral neuropathy was defined as the presence of monofilament insensitivity.
Results
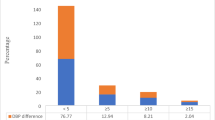
Every 5-mmHg increment in ILSBPD is associated with an about 14% increased risk of apparent peripheral neuropathy in crude model, but after adjustment for covariates, the correlation became nonsignificant (P = 0.160). When participants were divided into groups based on ILSBPD cutoffs of 5, 10 and 15 mmHg in different analyses, there was a significantly increased risk of apparent peripheral neuropathy in the ILSBPD ≥ 15 mmHg group (OR 1.79, 95% CI 1.11–2.91, P = 0.018), even after adjusting for confounders. In subgroup analysis, no interaction effect was found (all P for interaction > 0.05).
Conclusions
In US adults with diabetes, an increase in the ILSBPD (≥ 15 mmHg) was associated with a higher risk of apparent peripheral neuropathy.
Similar content being viewed by others
Background
Peripheral neuropathy covers a variety of clinicopathologies that may be associated with dysfunction of the peripheral nervous system [1]. Diabetes mellitus is the most common cause of peripheral neuropathy in Western societies, with a prevalence of up to 30–66% of diabetic patients [2]. In addition to the production of advanced glycation endproducts, reactive oxygen species and inflammatory factors caused by chronic hyperglycemia, structural microvasculature damage is an important cause of nerve dysfunction, as neuropathy is essentially a microvascular disorder [3,4,5,6,40, 41].
The current study has several limitations. First, it was a cross-sectional study without follow-up data; therefore, the causal relationship between ILSBPD and apparent peripheral neuropathy cannot be clarified. Second, the presence of apparent peripheral neuropathy was evaluated by the Semmes–Weinstein 10-g monofilament test, which is commonly used as a screening tool for apparent peripheral neuropathy but is likely to be interfered with by subjective factors, such as patient inattention and thickening of the skin. Additionally, as demographic data were self-reported by participants, there may be potential memory bias. Third, the NHANES excluded subjects deemed unsuitable for the examination of lower-extremity disease, such as participants with bilateral amputations, lesions and severe obesity, who are indeed at high risk of lower-extremity disease. Therefore, the actual prevalence of lower-extremity disease is underestimated, which might have influenced our conclusion.
Conclusions
In a population of US adults with diabetes, an increase in ILSBPD (≥ 15 mmHg) was associated with higher risk of apparent peripheral neuropathy.
Availability of data and materials
The datasets analyzed in the current study are available in the National Health and Nutritional Examination Surveys repository, https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
Abbreviations
- ILSBPD:
-
Interleg systolic blood pressure difference
- PAD:
-
Peripheral artery disease
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- SBP:
-
Systolic blood pressure
- ABI:
-
Ankle-brachial index
- TBI:
-
Toe-brachial index
- NHANES:
-
National Health and Nutritional Examination Surveys
- HbA1c:
-
Glycosylated hemoglobin
- SD:
-
Standard deviations
References
Wang Y, Li W, Peng W, Zhou J, Liu Z. Acupuncture for postherpetic neuralgia: systematic review and meta-analysis. Medicine. 2018;97(34):e11986.
Watson JC, Dyck PJ. Peripheral neuropathy: a practical approach to diagnosis and symptom management. Mayo Clin Proc. 2015;90(7):940–51.
Singh R, Kishore L, Kaur N. Diabetic peripheral neuropathy: current perspective and future directions. Pharmacol Res. 2014;80:21–35.
Jack M, Wright D. Role of advanced glycation endproducts and glyoxalase I in diabetic peripheral sensory neuropathy. Transl Res. 2012;159(5):355–65.
Oates PJ. Polyol pathway and diabetic peripheral neuropathy. Int Rev Neurobiol. 2002;50:325–92.
Low PA, Lagerlund TD, McManis PG. Nerve blood flow and oxygen delivery in normal, diabetic, and ischemic neuropathy. Int Rev Neurobiol. 1989;31:355–438.
**a P, Kramer RM, King GL. Identification of the mechanism for the inhibition of Na+, K(+)-adenosine triphosphatase by hyperglycemia involving activation of protein kinase C and cytosolic phospholipase A2. J Clin Invest. 1995;96(2):733–40.
Gordon Smith A, Robinson Singleton J. Idiopathic neuropathy, prediabetes and the metabolic syndrome. J Neurol Sci. 2006;242(1–2):9–14.
Oh J. Clinical spectrum and diagnosis of diabetic neuropathies. Korean J Intern Med. 2020;35(5):1059–69.
Sumpio BE. Foot ulcers. N Engl J Med. 2000;343(11):787–93.
Davies M, Brophy S, Williams R, Taylor A. The prevalence, severity, and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care. 2006;29(7):1518–22.
Bodman MA, Varacallo M. Peripheral diabetic neuropathy. Treasure Island: StatPearls; 2020.
Feng Y, Schlosser FJ, Sumpio BE. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg. 2009;50(3):675–82.
Müller-Bühl U. K.H. Bilaterality and symmetry of peripheral arterial occlusive disease. Perfusion. 2003;16:100–4.
Singh S, Sethi A, Singh M, Khosla S. Prevalence of simultaneously measured interarm systolic blood pressure difference and its clinical and demographic predictors: a systemic review and meta-analysis. Blood Press Monit. 2015;20(4):178–85.
Shadman R, Criqui M, Bundens W, Fronek A, Denenberg J, Gamst A, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44(3):618–23.
Herráiz-Adillo Á, Soriano-Cano A, Martínez-Hortelano JA, Garrido-Miguel M, Mariana-Herráiz J, Martínez-Vizcaíno V, et al. Simultaneous inter-arm and inter-leg systolic blood pressure differences to diagnose peripheral artery disease: a diagnostic accuracy study. Blood Press. 2018;27(2):121–2.
Okada H, Fukui M, Tanaka M, Matsumoto S, Mineoka Y, Nakanishi N, et al. A difference in systolic blood pressure between arms and between lower limbs is a novel risk marker for diabetic nephropathy in patients with type 2 diabetes. Hypertens Res. 2013;36(5):403–7.
Song X, Li G, Qiao A, Chen Z. Association of simultaneously measured four-limb blood pressures with cardiovascular function: a cross-sectional study. Biomed Eng Online. 2016;15(Suppl 2):147.
Yu S, Lu Y, **ong J, Bai B, Teliewubai J, Chi C, et al. The association of four-limb blood pressure differences with cardiovascular risk factors and target organ changes in elderly Chinese: the Northern Shanghai Study. Clin Exp Hypertens. 2020;42(3):275–80.
Su HM, Lin TH, Hsu PC, Lee WH, Chu CY, Chen SC, et al. Association of interankle systolic blood pressure difference with peripheral vascular disease and left ventricular mass index. Am J Hypertens. 2014;27(1):32–7.
Guo H, Sun F, Zhang H, Dong L, Gu X, Tian Y. Interankle systolic blood pressure difference is a marker of prevalent stroke in Chinese adults: a cross-sectional study. J Clin Hypertens. 2017;19(1):58–66.
Sheng CS, Liu M, Zeng WF, Huang QF, Li Y, Wang JG. Four-limb blood pressure as predictors of mortality in elderly Chinese. Hypertension. 2013;61(6):1155–60.
Chen SC, Chang JM, Tsai YC, Tsai JC, Su HM, Hwang SJ, et al. Association of interleg BP difference with overall and cardiovascular mortality in hemodialysis. Clin J Am Soc Nephrol. 2012;7(10):1646–53.
Sheen YJ, Li TC, Lin JL, Tsai WC, Kao CD, Bau CT, et al. Association between thermal threshold abnormalities and peripheral artery disease in patients with type 2 diabetes. Medicine. 2018;97(51):e13803.
Adler AI, Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Smith DG. Risk factors for diabetic peripheral sensory neuropathy. Results of the seattle prospective diabetic foot study. Diabetes Care. 1997;20(7):1162–7.
Kärvestedt L, Mårtensson E, Grill V, Elofsson S, von Wendt G, Hamsten A, et al. Peripheral sensory neuropathy associates with micro- or macroangiopathy: results from a population-based study of type 2 diabetic patients in Sweden. Diabetes Care. 2009;32(2):317–22.
National Center for Health Statistics. National Health and Nutrition Examination Survey: Analysis and Reporting Guideline. Available from: https://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf.
McGill M, Molyneaux L, Spencer R, Heng LF, Yue DK. Possible sources of discrepancies in the use of the Semmes-Weinstein monofilament. Impact on prevalence of insensate foot and workload requirements. Diabetes Care. 1999;22(4):598–602.
Mayfield JA, Sugarman JR. The use of the Semmes-Weinstein monofilament and other threshold tests for preventing foot ulceration and amputation in persons with diabetes. J Fam Pract. 2000;49(11 Suppl):S17-29.
Gregg EW, Sorlie P, Paulose-Ram R, Gu Q, Eberhardt MS, Wolz M, et al. Prevalence of lower-extremity disease in the US adult population >=40 years of age with and without diabetes: 1999–2000 national health and nutrition examination survey. Diabetes Care. 2004;27(7):1591–7.
National Center for Health Statistics. National health and nutrition examination survey: lower extremity disease - peripheral neuropathy (LEXPN). Available from: https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/LEXPN.htm.
Papanas N, Symeonidis G, Mavridis G, Georgiadis G, Papas T, Lazarides M, et al. Ankle-brachial index: a surrogate marker of microvascular complications in type 2 diabetes mellitus? Int Angiol J Int Union Angiol. 2007;26(3):253–7.
National Guideline C. National Institute for Health and Care Excellence: Clinical Guidelines. In: Hypertension in adults: diagnosis and management. 2019, National Institute for Health and Care Excellence (UK) Copyright © NICE 2019: London.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Liu S, Li P, Su H. Four-limb blood pressure measurement with an oscillometric device: a tool for diagnosing peripheral vascular disease. Curr Hypertens Rep. 2019;21(2):15.
Gong Y, Cao KW, Xu JS, Li JX, Hong K, Cheng XS, et al. Valuation of normal range of ankle systolic blood pressure in subjects with normal arm systolic blood pressure. PLoS ONE. 2015;10(6):e0122248.
Herráiz-Adillo Á, Soriano-Cano A, Martínez-Hortelano JA, Garrido-Miguel M, Mariana-Herráiz J, Martínez-Vizcaíno V, et al. Simultaneous inter-arm and inter-leg systolic blood pressure differences to diagnose peripheral artery disease: a diagnostic accuracy study. Blood Press. 2018;27(2):112–9.
Singh S, Sethi A, Singh M, Khosla K, Grewal N, Khosla S. Simultaneously measured inter-arm and inter-leg systolic blood pressure differences and cardiovascular risk stratification: a systemic review and meta-analysis. J Am Soc Hypertens. 2015;9(8):640–50.
Nukada H. Ischemia and diabetic neuropathy. Handb Clin Neurol. 2014;126:469–87.
Ylitalo K, Sowers M, Heeringa S. Peripheral vascular disease and peripheral neuropathy in individuals with cardiometabolic clustering and obesity: National Health and Nutrition Examination Survey 2001–2004. Diabetes Care. 2011;34(7):1642–7.
Acknowledgements
We thank Kelly Zammit, BVSc, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows: ZL, HW, XL and SL designed the study; JL provided mentoring and guidance throughout the project. ZL acquired the data with help from HW; XL, ZL, HW, XL and SL analyzed the data; XL, ZL and XL wrote and rechecked the manuscript; XL and ZL checked and re-analyzed the data, revised the manuscript and polished the language; and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The National Center for Health Statistics Ethics Review Board approved the study, and informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, X., Liu, Z., Weng, H. et al. Association between interleg systolic blood pressure difference and apparent peripheral neuropathy in US adults with diabetes: a cross-sectional study. J Health Popul Nutr 42, 131 (2023). https://doi.org/10.1186/s41043-023-00475-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-023-00475-2