Abstract
Background
This study aims to validate two predictive formulas of weight estimating strategies in children with special needs, namely the Cattermole formula and the Mercy formula.
Methodology
A cross-sectional study with a universal sampling of children and adolescents with special needs aged 2–18 years old, diagnosed with cerebral palsy, down syndrome, autism and attention-deficit/hyperactivity disorder was conducted at Community-Based Rehabilitation in Central Zone Malaysia. Socio-demographic data were obtained from files, and medical reports and anthropometric measurements (body weight, height, humeral length, and mid-upper arm circumference) were collected using standard procedures. Data were analysed using IBM SPSS version 26. The accuracy of the formula was determined by intraclass correlation, prediction at 20% of actual body weight, residual error (RE) and root mean square error (RMSE).
Result
A total of 502 children with a median age of 7 (6) years were enrolled in this study. The results showed that the Mercy formula demonstrated a smaller degree of bias than the Cattermole formula (PE = 1.97 ± 15.99% and 21.13 ± 27.76%, respectively). The Mercy formula showed the highest intraclass correlation coefficient (0.936 vs. 0.858) and predicted weight within 20% of the actual value in the largest proportion of participants (84% vs. 48%). The Mercy formula also demonstrated lower RE (0.3 vs. 3.6) and RMSE (3.84 vs. 6.56) compared to the Cattermole formula. Mercy offered the best option for weight estimation in children with special needs in our study population.
Similar content being viewed by others
Introduction
Body weight is a crucial anthropometric measure that health care professionals frequently use to analyse children's growth charts and developmental patterns. In clinical and community settings, body weight is an important indicator for dietary and medical intervention. Several techniques have been developed to assess body weight in children who are typically developed (TD). Children with both physical and intellectual disabilities lacked the validity of the body weight predictive equation. These distinct individuals could have varying morphologies, body types, and distinctive traits that are compromised [1].
Nutritional status is an important indicator of the overall health status and well-being of disabled children [2]. Low nutritional status was a prime contributor to poor-growth children [3]. Malnutrition is common in children with special needs due to feeding difficulties [4–6], frequent illness [5], poor nutrient absorption [7] and poor care [8]. Children with cerebral palsy (CP) and Down syndrome (DS) are at risk of nutritional deficiency due to poor oral motor feeding and swallowing problems [9].
In Malaysia, the prevalence of underweight ranged from 22.2 to 78.2% among children with CP. Children with DS are at risk for overweight and obesity, with a prevalence of 33.5–43.5% [2]. With a prevalence of 7.8% underweight and 24.8% overweight or obese, children with autism spectrum disorder (ASD) are at risk for double-burden malnutrition [2].
Using a calibrated weighing scale is the gold standard for determining a child's weight [10]. Various methods have been established for measuring body weight in children who are typically developed (TD). These distinct individuals could have varying morphologies, physiques, or other distinctive traits [1]. Due to their oppositional behaviour and physical impairments, children with special needs may make it challenging to gauge their body weight. Thus, alternative weight equations/formulas are required to estimate weight in this unique group. According to other research [11, 12], body length/height, humeral length (HL) and mid-upper arm circumference (MUAC) are the usual alternative measurements for weight in children. A weight estimation formula includes at least one of the alternate metrics given. Several methods of paediatric weight estimation were developed based on age, body length and MUAC. In particular, the Broselow emergency tape was frequently utilised in Malaysia to estimate the body weight of paediatric patients in the emergency room based on their length and height [13]. However, the Broselow method could not be applied to children with severe joint contractures or neurologic defects [13, 14]. In addition, most age-based weight estimation methods, such as Advanced Pediatric Life Support (APLS), are restricted to healthy children up to 15 years only [11]. Hence, this study only involves length and habitus-based weight estimation methods, namely the Cattermole (MUAC) and Mercy (Humerus Length & MUAC) methods. These methods could be applied in children with special needs regardless of their age and height limitations.
It is still unclear how accurate weight assessment is in children with special needs (CWSNs). Only one study estimated weight in children with Down syndrome [15]. To date, no published research has been conducted to evaluate the performance of weight estimating methods in CWSNs in Malaysia.
This research was therefore critical in attempting to determine an accurate method of weight estimation among CWSNs. Hence, this study was conducted to validate two predictive formulas of weight estimation strategies in children with special needs, namely the Cattermole (MUAC) formula and the Mercy (HL and MUAC) formula. Furthermore, this study could help health care practitioners estimate weight whenever direct weight measurement is impossible or impractical.
Methodology
Study design and population
A cross-sectional study design with universal sampling was conducted at selected Community-Based Rehabilitation Centres (CBRs) in Central Zone Malaysia (Selangor, Federal Territory of Putrajaya and Kuala Lumpur and Seremban). Children diagnosed with Down Syndrome (DS), Cerebral Palsy (CP) and autism spectrum disorder (ASD)/Attention Deficit Hyperactive Disorder (ADHD) aged 2 to 18 years who attended Community-Based Rehabilitation Centres (CBR) were included in this study. Meanwhile, children diagnosed with other disabilities and suffering from oedema, ascites, pleural effusion, large tumour condition and hydrocephalus were excluded from the study. Study protocol approval was obtained from the National Medical Research Registry Malaysia (NMRR) (ID: NMRR-17-2743-35970). The ethics of the protocol was approved by the Medical Research and Ethics Committee (MREC) Malaysia with confidentiality maintained for all subjects. Written consent was obtained from the parent/caregiver prior to data collection. Out of 3,436 children who enrolled in CBR, 502 children met the inclusion criteria and consented to participate in this study.
Data collection
Socio-demographic data were obtained from individual files, and medical reports and anthropometric measurements were performed for body weight, height, humeral length (HL) and mid-upper arm circumference (MUAC). The actual body weight of the children was measured by a SECA 674 platform weighing scale in any position, either standing upright, sitting, or lying down, and readings were recorded to the nearest 0.01 kg. Body height was measured with a standard procedure using a stadiometer SECA 213 to the nearest 0.1 cm [16]. Humeral length and MUAC were measured using the retractable measuring tape SECA 201 to the nearest 0.1 cm. HL was measured from the top of the shoulder (acromion) to the point of the elbow (olecranon process) [17], while MUAC was measured at the midpoint of the distance between the shoulder bone (acromion) and the elbow (electron process). Data on HL and MUAC were applied to the Mercy equation, while MUAC alone was applied to the Cattermole equation [(MUAC in cm − 10) × 3] [18].
Statistical analysis
All data obtained were analysed using IBM SPSS (Statistical Package for Social Science) version 26. The normality of the continuous data was determined by using Shapiro‒Wilk’s and Kolmogorov‒Smirnov tests. Demographic data are presented as frequencies and percentages for categorical variables. Meanwhile, the mean ± standard deviation (SD) or median ± interquartile range (IQR) was described in the continuous data. Spearman correlation was used to determine the relationship between variables. The mean error (ME), mean percentage error (MPE) and root mean square error (RMSE) were determined. Residual error (RE) was calculated by taking the difference in estimated weight and actual weight. Next, percentage error (PE) was calculated by dividing the actual weight into the mean error (ME) and multiplying by 100. The root mean square error (RMSE) was calculated by taking the square root of the average squared error. The percentages of estimated weights and actual weight are targeted at the level of 20% from actual weight by analysis of Variance (ANOVA) and Bland‒Altman plots. In addition, the intraclass correlation (ICC) was calculated using a 2-way random-effects model, and absolute agreement with a significant level was determined at p < 0.05.
Results
A total of 502 special needs children aged 2 to 18 years participated in this study. The median age of the children was 7 (6) years; two-thirds of them (66.7%) were boys, and the majority were of Malay ethnicity (91.2%). Approximately, 31.5% of the studied population was diagnosed with cerebral palsy, and half of them were in GMFCS I to GMFCS III. Detail socio-demographic as presented in Table 1.
Anthropometric measurements are stated in Table 2. Body height, mid-upper arm circumference and humeral length showed a strong correlation with body weight, as presented in Table 2.
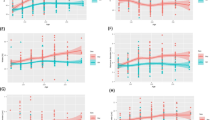
The results show that the Mercy formula demonstrated a smaller degree of bias than the Cattermole formula (PE = 1.97 ± 15.99% and 21.13 ± 27.76%, respectively). The Mercy formula showed a higher intraclass correlation coefficient (0.936 vs. 0.858) and predicted weight within 20% of the actual value in the largest proportion of participants (84% vs. 48%). The Mercy formula also demonstrated lower RE (0.3 vs. 3.6) and RMSE (3.84 vs. 6.56) compared to the Cattermole formula. Figure 1 shows the regression between predictive weight and actual weight and the Bland‒Altman plot for both predictive equations.
The predictive performance of the Cattermole and Mercy weight estimation methods are shown in Table 3.
Discussion and conclusion
This study offered important insight into weight estimation for children with special needs aged 2–18 years whenever the standard weight measurement was impossible. Due to the physical constraints and cognitive disability among children with special needs, alternative weight measurements are required to predict their actual weight. In this study, the Cattermole and Mercy weight estimation methods were comparable, and surprisingly, both methods were predictors of the actual weight. The Mercy weight estimate method (partial weight of HL + partial weight of MUAC) was more accurate in predicting the real weight than the Cattermole weight estimation method. Findings from this study were in agreement with a previous study conducted by Talib et al. [15] in the United States of America, which demonstrated Mercy as the best option to estimate weight in Down syndrome children aged 18 years and below compared with other methods, including the Cattermole, Broselow tape and APLS methods.
In addition, the agreement within 20% of the actual weight between the current study and the previous study [15] was comparable. The Mercy method in this study demonstrated the closest proportion of children’s estimated weight within 20% of actual weight with the Mercy method in a previous study (85% vs. 88%). Similarly, the Cattermole method in this study proposed a near proportion of children’s estimated weight within 20% of actual weight with the Cattermole method in the previous study (48% vs. 40%). Nevertheless, the Mercy method in the current study was found to overestimate the actual weight, while the Mercy method in the previous study [15] was reported to underestimate the actual weight (RE 0.287 kg vs. − 1.4 kg).
The Mercy method performed better than the Cattermole method in this study because the two-dimensional systems were always far superior in accuracy to the one-dimensional system [19]. The Mercy method incorporates two-dimensional systems (HL and MUAC), which results in more accurate weight estimation than the Cattermole method, which only relies on MUAC [15, 11, 19]. To date, no study has reported that one-dimensional systems are more accurate than two-dimensional systems [19].
Furthermore, the finding of low accuracy of the Cattermole method in this study was in line with the studies conducted among Korean children by Choi et al. [21] and Suh et al. [20], which revealed that the Cattermole method was the worst accurate method and was only highly precise in children aged 6 to 14 years. Moreover, the accuracy of the Cattermole weight estimation method to predict weight in children with special needs is unclear. The existing studies related to Cattermole estimation weight were conducted among normal children [18, 21, 20] and were reliable in school-age children [18].
Instead of special needs children, the Mercy weight estimation method was also accurate in predicting weight in normal children [22–25]. Additionally, the Mercy approach proved more accurate than other methods in a wider range of ages [11]. Hence, it has been observed that the Mercy weight estimation method was more applicable in both normal and special needs children with a wide age range.
Several limitations to this study need to be acknowledged. This study did not engage with normal children or other special needs children diagnosed beyond Down syndrome, autism/ADHD and cerebral palsy. In addition, the current study merely focused on children with special needs aged 2–18 years, and findings from this study could not be extrapolated to other age populations, such as adults and elderly individuals. Moreover, the accuracy of weight estimation methods decreases with increasing age [23]. Furthermore, this study only involved two weight estimation methods, namely the Cattermole and Mercy methods, that could predict the weight of the children in this study. The accuracy of other weight estimation methods could not be determined in the current study. In addition, there is no reference standard or benchmark for assessing the accuracy of the weight estimation methods. Therefore, further local research is required to explore the accuracy of other weight estimation methods.
In conclusion, the humeral length and mid-upper arm circumference were the most robust factors for predicting actual weight in children with special needs. The most apparent finding that emerged from this study was that the Mercy weight estimation method performed well in Malaysian special needs children, similar to that shown in the Western population. Hence, the Mercy weight estimation method is recommended to predict the actual weight in Malaysian special needs children aged 2 to 18 years.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable requests.
Abbreviations
- MUAC:
-
Mid-upper arm circumference
- HL:
-
Humeral length
- GMFCS:
-
Gross motor function classification system
- CP:
-
Cerebral palsy
- DS:
-
Down syndrome
- CWSN:
-
Children with special needs
References
Rieken R, van Goudoever JB, Schierbeek H, Willemsen SP, Calis EA, Tibboel D, Evenhuis HM, Penning C. Measuring body composition and energy expenditure in children with severe neurologic impairment and intellectual disability. Am J Clin Nutr. 2011;94(3):759–66. https://doi.org/10.3945/ajcn.110.003798.
Nor Safiza MN, Nur Shahida AA, Siew Man C, Rashidah A, Mohd Azahadi O. Nutritional status of children with autism spectrum disorders, cerebral palsy and down syndrome: a sco** review. Open Access J Sci Technol. 2015;3(9):1–11.
Kuperminc MN, Stevenson RD. Growth and nutrition disorders in children with cerebral palsy. Dev Disabil Res Rev. 2008;14(2):137–46.
Rajikan R, Zakaria NM, Manaf ZA, Yusoff NAM, Shahar S. The effect of feeding problems on the growth of children and adolescents with cerebral palsy. J Fundam Appl Sci. 2017;9(6S):787–804.
Aggarwal S, Chadha R, Pathak R. Nutritional status and growth in children with cerebral palsy: a review. Int J Med Sci Public Health. 2015;4(6):737–44.
Yi TI, Huh WS, Ku HK, Seo IS, Shim JW, Lee GE, Kim JS, Park JS. Nutritional status of children with Cerebral palsy. J Korean Acad Rehabilit Med. 2011;35(1):42–7.
Kerac M, Postels DG, Mallewa M, Jalloh AA, Voskuijl WP, Groce N, Gladstone M, Molyneux E. The interaction of malnutrition and neurologic disability in Africa. In: Seminars in pediatric neurology. WB Saunders; 2014;21(1):42–49.
Polack S, Adams M, O’banion D, Baltussen M, Asante S, Kerac M, Gladstone M, Zuurmond M. Children with cerebral palsy in Ghana: malnutrition, feeding challenges, and caregiver quality of life. Dev Med Child Neurol. 2018;60(9):914–21.
Groce N, Challenger E, Berman-Bieler R, Farkas A, Yilmaz N, Schultink W, Clark D, Kaplan C, Kerac M. Malnutrition and disability: unexplored opportunities for collaboration. Paediatr Int Child Health. 2014;34(4):308–14.
Udoh II, Moses IJ. A comparison of three age-based formulae of estimating weight in Nigerian children. Am J Med Sci Med. 2015;3:24–7.
Abdel-Rahman SM, Ahlers N, Holmes A, Wright K, Harris A, Weigel J, Hill T, Baird K, Michaels M, Kearns GL. Validation of an improved pediatric weight estimation strategy. J Pediatr Pharmacol Ther. 2013;18(2):112–21.
Manirafasha A, Yi S, Cattermole GN. Estimating children’s weight in a Rwandan emergency centre. Afr J Emerg Med. 2018;8(2):55–8.
Mohd Azman S, Norsyam Juliana N, Ahmad Tajuddin MN, Mohd Idzwan Z. Weight estimation method in Emergency Department in Malaysia: Is Broselow Tape (BT) reliable? J Teknol 2016;78(6–8).
Nordin NJ, Sahar MA, Nor ATM, Zakaria MI. Weight estimation method in Emergency Department in Malaysia: Is Broselow Tape (BT) reliable? Jurnal Teknologi (Sciences & Engineering) 2016;78:6–8, 113–117.
Talib NJ, Rahm G, Abdel-Rahman SM. Estimating weight in children with down syndrome. Glob Pediatr Health. 2015;2:2333794X14568450.
Lee RD, Niemen DC. Chapter 6: Anthropometry. Nutritional assessment (4th ed., Vols. 169–221). New York: McGraw-Hill. 2007.
International Society for the Advancement of Kinanthropometry (ISAK) (2001) International standards for anthropometric assessment. ISAK, Patche Fstroom.
Cattermole GN, Leung PYM, Mak PSK, Graham CA, Rainer TH. Mid-arm circumference can be used to estimate children’s weights. Resuscitation. 2010;81(9):1105–10.
Wells M, Goldstein LN, Bentley A. The accuracy of emergency weight estimation systems in children-a systematic review and meta-analysis. Int J Emerg Med. 2017;10(1):29. https://doi.org/10.1186/s12245-017-0156-5
Suh D, Jung SY, Kim DK, Kwak YH. 166 Validation of pediatric weight estimation methods using mid-upper arm circumference. Ann Emerg Med. 2014;64(4):S60.
Choi JY, Suh D, Kwak YH, Jung JY, Lee JH, Jeong JH, Kwon H, Paek SH. Validation of the mid-arm-based weight estimation formula (the Cattermole formula) for Korean children. Resuscitation. 2018;132:13–6.
Samerchua A, Suraseranivongse S, Komoltri C. A comparison of pediatric weight estimation methods for emergency resuscitation. Pediatr Emerg Care. 2019;35(10):705–11.
Abdel-Rahman SM, Ridge AL. An improved pediatric weight estimation strategy. Open Med Dev J. 2012;4:87–97.
Batmanabane G, Jena PK, Dikshit R, Abdel-Rahman S. Using the Mercy Method for weight estimation in Indian children. Glob Pediatr Health. 2015;2:2333794X14566625.
Dicko A, Alhousseini ML, Sidibé B, Traoré M, Abdel-Rahman SM. Evaluation of the Mercy weight estimation method in Ouelessebougou. Mali BMC Public Health. 2014;14(1):270.
Acknowledgements
The authors would like to acknowledge the Director General of Health Malaysia for permission to publish this paper. Appreciation goes to the Department of Social Welfare (Malaysia), for permission to run this study at their facilities and recruit the trainees. Acknowledgement also goes to the Family Health Development Division, Ministry of Health Malaysia in the preparation and during the data collection. Our sincere appreciation also goes to all participants and data collectors.
Funding
Publication costs are funded by the National Institute of Health Malaysia with grant and research ID no of NMRR-17-2743-35970. The funders had no role in the study design, data collection, data analysis, data interpretation or writing of the article.
Author information
Authors and Affiliations
Contributions
NHI, NK, SO, MAO, NS, AAA, NMN, MNZ, MNA, MFS, NAR and SFM were responsible for the concept and project development. NHI and NK supervised the project’s progress. NHI, NK and SFM designed the outline of the manuscript. MOA and SO contributed to a critical review of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approvals for the study were obtained from the Medical Research Ethics Committee (MREC), Ministry of Health Malaysia (NMRR-17-423-34969) prior to conducting the study. Informed written consent was collected from all respondents at the beginning of the study Consent for publication Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ibrahim, N.H., Kassim, N., Othman, S. et al. Validation study on a prediction formula to estimate the weight of children & adolescents with special needs aged 2–18 years old. J Health Popul Nutr 42, 129 (2023). https://doi.org/10.1186/s41043-023-00464-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-023-00464-5