Loebel C, Burdick JA. Engineering Stem and Stromal Cell Therapies for Musculoskeletal Tissue Repair. Cell Stem Cell. 2018;22:325–39.
Article
CAS
Google Scholar
Lv B, Lu L, Hu L, Cheng P, Hu Y, **e X, et al. Recent advances in GelMA hydrogel transplantation for musculoskeletal disorders and related disease treatment. Theranostics. 2023;13:2015–39.
Article
CAS
Google Scholar
Khodabukus A, Guyer T, Moore AC, Stevens MM, Guldberg RE, Bursac N. Translating musculoskeletal bioengineering into tissue regeneration therapies. Sci Transl Med. 2022;14:eabn9074.
Article
CAS
Google Scholar
Safiri S, Kolahi AA, Cross M, Hill C, Smith E, Carson-Chahhoud K, et al. Prevalence, Deaths, and Disability-Adjusted Life Years Due to Musculoskeletal Disorders for 195 Countries and Territories 1990-2017. Arthritis Rheumatol. 2021;73:702–14.
Article
CAS
Google Scholar
Wubneh A, Tsekoura EK, Ayranci C, Uludağ H. Current state of fabrication technologies and materials for bone tissue engineering. Acta Biomater. 2018;80:1–30.
Article
CAS
Google Scholar
Bartok B, Firestein GS. Fibroblast-like synoviocytes: key effector cells in rheumatoid arthritis. Immunol Rev. 2010;233:233–55.
Article
CAS
Google Scholar
Pan S, Yin J, Yu L, Zhang C, Zhu Y, Gao Y, et al. 2D MXene-Integrated 3D-Printing Scaffolds for Augmented Osteosarcoma Phototherapy and Accelerated Tissue Reconstruction. Adv Sci (Weinh). 2020;7:1901511.
CAS
Google Scholar
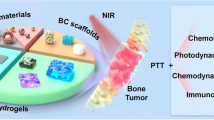
Liao J, Han R, Wu Y, Qian Z. Review of a new bone tumor therapy strategy based on bifunctional biomaterials. Bone Res. 2021;9:18.
Article
Google Scholar
Huo J, Jia Q, Huang H, Zhang J, Li P, Dong X, et al. Emerging photothermal-derived multimodal synergistic therapy in combating bacterial infections. Chem Soc Rev. 2021;50:8762–89.
Article
CAS
Google Scholar
Kong H, Chu Q, Fang C, Cao G, Han G, Li X. Cu-Ferrocene-Functionalized CaO(2) Nanoparticles to Enable Tumor-Specific Synergistic Therapy with GSH Depletion and Calcium Overload. Adv Sci (Weinh). 2021;8:e2100241.
Google Scholar
Zhang L, Oudeng G, Wen F, Liao G. Recent advances in near-infrared-II hollow nanoplatforms for photothermal-based cancer treatment. Biomater Res. 2022;26:61.
Article
Google Scholar
Xue Y, Zhang L, Liu F, Zhao Y, Zhou J, Hou Y, et al. Surface Bandgap Engineering of Nanostructured Implants for Rapid Photothermal Ion Therapy of Bone Defects. Adv Healthc Mater. 2022;11:e2200998.
Article
Google Scholar
Yi X, Duan QY, Wu FG. Low-Temperature Photothermal Therapy: Strategies and Applications. Research (Wash D C). 2021;2021:9816594.
CAS
Google Scholar
Liu Y, Bhattarai P, Dai Z, Chen X. Photothermal therapy and photoacoustic imaging via nanotheranostics in fighting cancer. Chem Soc Rev. 2019;48:2053–108.
Article
CAS
Google Scholar
Sun H, Xu J, Wang Y, Shen S, Xu X, Zhang L, et al. Bone microenvironment regulative hydrogels with ROS scavenging and prolonged oxygen-generating for enhancing bone repair. Bioact Mater. 2023;24:477–96.
CAS
Google Scholar
Rockwood DN, Gil ES, Park SH, Kluge JA, Grayson W, Bhumiratana S, et al. Ingrowth of human mesenchymal stem cells into porous silk particle reinforced silk composite scaffolds: An in vitro study. Acta Biomater. 2011;7:144–51.
Article
CAS
Google Scholar
Collins MN, Ren G, Young K, Pina S, Reis RL, Oliveira JM. Scaffold Fabrication Technologies and Structure/Function Properties in Bone Tissue Engineering. Adv Funct Mater. 2021;31:2010609.
Article
CAS
Google Scholar
Huang Y, Zhai X, Ma T, Zhang M, Yang H, Zhang S, et al. A Unified Therapeutic–Prophylactic Tissue-Engineering Scaffold Demonstrated to Prevent Tumor Recurrence and Overcoming Infection toward Bone Remodeling. Adv Mater. 2023;35:2300313.
Article
CAS
Google Scholar
Inyushin M, Meshalkina D, Zueva L, Zayas-Santiago A. Tissue Transparency In Vivo. Molecules. 2019;24:2388.
Hsieh ZH, Fan CH, Ho YJ, Li ML, Yeh CK. Improvement of light penetration in biological tissue using an ultrasound-induced heating tunnel. Sci Rep. 2020;10:17406.
Article
CAS
Google Scholar
Hong G, Antaris AL, Dai H. Near-infrared fluorophores for biomedical imaging. Nature Biomed Eng. 2017;1:0010.
Hong G, Diao S, Antaris AL, Dai H. Carbon Nanomaterials for Biological Imaging and Nanomedicinal Therapy. Chem Rev. 2015;115:10816–906.
Article
CAS
Google Scholar
Juzenas P, Juzeniene A, Kaalhus O, Iani V, Moan J. Noninvasive fluorescence excitation spectroscopy during application of 5-aminolevulinic acid in vivo. Photochem Photobiol Sci. 2002;1:745–8.
Article
CAS
Google Scholar
Carr JA, Aellen M, Franke D, So PTC, Bruns OT, Bawendi MG. Absorption by water increases fluorescence image contrast of biological tissue in the shortwave infrared. Proc Natl Acad Sci USA. 2018;115:9080–5.
Article
CAS
Google Scholar
Tian L, Xu Z, Zhao S, Cui Y, Liang Z, Zhang J, et al. The Upconversion Luminescence of Er3+/Yb3+/Nd3+ Triply-Doped β-NaYF4 Nanocrystals under 808-nm Excitation. Materials (Basel). 2014;7:7289–303.
Article
Google Scholar
Lin H, Gao S, Dai C, Chen Y, Shi J. A Two-Dimensional Biodegradable Niobium Carbide (MXene) for Photothermal Tumor Eradication in NIR-I and NIR-II Biowindows. J Am Chem Soc. 2017;139:16235–47.
Article
CAS
Google Scholar
Hemmer E, Benayas A, Légaré F, Vetrone F. Exploiting the biological windows: current perspectives on fluorescent bioprobes emitting above 1000 nm. Nanoscale Horiz. 2016;1:168–84.
Article
CAS
Google Scholar
**g D, Yi Y, Luo W, Zhang S, Yuan Q, Wang J, et al. Tissue Clearing and Its Application to Bone and Dental Tissues. J Dent Res. 2019;98:621–31.
Article
CAS
Google Scholar
Firbank M, Hiraoka M, Essenpreis M, Delpy DT. Measurement of the optical properties of the skull in the wavelength range 650-950 nm. Phys Med Biol. 1993;38:503–10.
Article
CAS
Google Scholar
Ugryumova N, Matcher SJ, Attenburrow DP. Measurement of bone mineral density via light scattering. Phys Med Biol. 2004;49:469–83.
Article
Google Scholar
Saul D, Khosla S. Fracture Healing in the Setting of Endocrine Diseases, Aging, and Cellular Senescence. Endocr Rev. 2022;43:984–1002.
Article
Google Scholar
Pajarinen J, Lin T, Gibon E, Kohno Y, Maruyama M, Nathan K, et al. Mesenchymal stem cell-macrophage crosstalk and bone healing. Biomaterials. 2019;196:80–9.
Article
CAS
Google Scholar
Zhang W, Gu J, Li K, Zhao J, Ma H, Wu C, et al. A hydrogenated black TiO2 coating with excellent effects for photothermal therapy of bone tumor and bone regeneration. Mater Sci Eng C Mater Biol Appl. 2019;102:458–70.
Article
CAS
Google Scholar
Zhao Y, Peng X, Wang D, Zhang H, **n Q, Wu M, et al. Chloroplast-inspired Scaffold for Infected Bone Defect Therapy: Towards Stable Photothermal Properties and Self-Defensive Functionality. Adv Sci (Weinh). 2022;9:e2204535.
Google Scholar
Tong L, Liao Q, Zhao Y, Huang H, Gao A, Zhang W, et al. Near-infrared light control of bone regeneration with biodegradable photothermal osteoimplant. Biomaterials. 2019;193:1–11.
Article
CAS
Google Scholar
Ali MRK, Wu Y, Tang Y, **ao H, Chen K, Han T, et al. Targeting cancer cell integrins using gold nanorods in photothermal therapy inhibits migration through affecting cytoskeletal proteins. Proc Natl Acad Sci USA. 2017;114:E5655–63.
Article
CAS
Google Scholar
Zhang J, Tang S, Ding N, Ma P, Zhang Z. Surface-modified Ti(3)C(2) MXene nanosheets for mesenchymal stem cell osteogenic differentiation via photothermal conversion. Nanoscale Adv. 2023;5:2921–32.
Article
CAS
Google Scholar
Wu M, Liu H, Zhu Y, Chen F, Chen Z, Guo L, et al. Mild Photothermal-Stimulation Based on Injectable and Photocurable Hydrogels Orchestrates Immunomodulation and Osteogenesis for High-Performance Bone Regeneration. Small. 2023;19:e2300111.
Ma K, Liao C, Huang L, Liang R, Zhao J, Zheng L, et al. Electrospun PCL/MoS(2) Nanofiber Membranes Combined with NIR-Triggered Photothermal Therapy to Accelerate Bone Regeneration. Small. 2021;17:e2104747.
Article
Google Scholar
Shan H, Zhou X, Tian B, Zhou C, Gao X, Bai C, et al. Gold nanorods modified by endogenous protein with light-irradiation enhance bone repair via multiple osteogenic signal pathways. Biomaterials. 2022;284:121482.
Article
CAS
Google Scholar
Yanli Z, Jiayao M, Chunqing Z, Yuting Z, Zhiyan Z, Yulin Z, et al. MY-1 Loaded Nano-Hydroxyapatite Accelerated Bone Regeneration by Increasing Type III Collagen Deposition in Early-stage ECM via a Hsp47 Dependent Mechanism. Adv Healthc Mater. 2023;12:e2300332.
Amirkavei M, Pitkänen M, Kaikkonen O, Kaarniranta K, André H, Koskelainen A. Induction of Heat Shock Protein 70 in Mouse RPE as an In Vivo Model of Transpupillary Thermal Stimulation. Int J Mol Sci. 2020;21:2063.
Sayed S, Faruq O, Hossain M, Im S-B, Kim Y-S, Lee B-T. Thermal cycling effect on osteogenic differentiation of MC3T3-E1 cells loaded on 3D-porous Biphasic Calcium Phosphate (BCP) scaffolds for early osteogenesis. Mater Sci Eng C Mater Biol Appl. 2019;105:110027.
Article
CAS
Google Scholar
Li W, Li S, Zhang J, Zhong H, Liang J, Huang S, et al. Fabrication and evaluation of bone morphogenetic protein-2 microspheres coated black phosphorus nanosheets@polylactic-glycolic acid copolymers scaffold: A multifunctional antibacterial photothermal scaffold for bone regeneration. Int J Biol Macromol. 2022;210:350–64.
Article
CAS
Google Scholar
Fan Q, Bai J, Shan H, Fei Z, Chen H, Xu J, et al. Implantable blood clot loaded with BMP-2 for regulation of osteoimmunology and enhancement of bone repair. Bioact Mater. 2021;6:4014–26.
CAS
Google Scholar
Qu X, Guo Y, **e C, Li S, Liu Z, Lei B. Photoactivated MXene Nanosheets for Integrated Bone-Soft Tissue Therapy: Effect and Potential Mechanism. ACS Nano. 2023;17:7229–240.
Google Scholar
Li Y, Xu Z, Wang J, Pei X, Chen J, Wan Q. Alginate-based biomaterial-mediated regulation of macrophages in bone tissue engineering. Int J Biol Macromol. 2023;230:123246.
Article
CAS
Google Scholar
**e X, Wei J, Zhang B, **ong W, He Z, Zhang Y, et al. A self-assembled bilayer polypeptide-engineered hydrogel for spatiotemporal modulation of bactericidal and anti-inflammation process in osteomyelitis treatment. J Nanobiotechnol. 2022;20:416.
Article
CAS
Google Scholar
Li B, Liu F, Ye J, Cai X, Qian R, Zhang K, et al. Regulation of Macrophage Polarization Through Periodic Photo-Thermal Treatment to Facilitate Osteogenesis. Small. 2022;18:e2202691.
Article
Google Scholar
Stegen S, van Gastel N, Carmeliet G. Bringing new life to damaged bone: the importance of angiogenesis in bone repair and regeneration. Bone. 2015;70:19–27.
Article
CAS
Google Scholar
Fröhlich LF. Micrornas at the Interface between Osteogenesis and Angiogenesis as Targets for Bone Regeneration. Cells. 2019;8:121.
Wu Y, Zhang X, Tan B, Shan Y, Zhao X, Liao J. Near-infrared light control of GelMA/PMMA/PDA hydrogel with mild photothermal therapy for skull regeneration. Biomater Adv. 2022;133:112641.
Article
Google Scholar
Zhang X, Cheng G, **ng X, Liu J, Cheng Y, Ye T, et al. Near-Infrared Light-Triggered Porous AuPd Alloy Nanoparticles To Produce Mild Localized Heat To Accelerate Bone Regeneration. J Phys Chem Lett. 2019;10:4185–91.
Article
CAS
Google Scholar
Zhang Y, Li C, Zhang W, Deng J, Nie Y, Du X, et al. 3D-printed NIR-responsive shape memory polyurethane/magnesium scaffolds with tight-contact for robust bone regeneration. Bioact Mater. 2022;16:218–31.
CAS
Google Scholar
Huang Z, Li J, Chen X, Yang Q, Zeng X, Bai R, et al. Photothermal Sensitive 3D Printed Biodegradable Polyester Scaffolds with Polydopamine Coating for Bone Tissue Engineering. Polymers (Basel). 2023;15:381.
Liu S, Han Z, Hao JN, Zhang D, Li X, Cao Y, et al. Engineering of a NIR-activable hydrogel-coated mesoporous bioactive glass scaffold with dual-mode parathyroid hormone derivative release property for angiogenesis and bone regeneration. Bioact Mater. 2023;26:1–13.
Google Scholar
Li Q, Liu W, Hou W, Wu X, Wei W, Liu J, et al. Micropatterned photothermal double-layer periosteum with angiogenesis-neurogenesis coupling effect for bone regeneration. Mater Today Bio. 2022;18:100536.
Article
CAS
Google Scholar
Wang C, Yue H, Liu J, Zhao Q, He Z, Li K, et al. Advanced reconfigurable scaffolds fabricated by 4D printing for treating critical-size bone defects of irregular shapes. Biofabrication. 2020;12:045025.
Article
CAS
Google Scholar
Wang Y, Hu X, Zhang L, Zhu C, Wang J, Li Y, et al. Bioinspired extracellular vesicles embedded with black phosphorus for molecular recognition-guided biomineralization. Nat Commun. 2019;10:2829.
Article
Google Scholar
Wang X, Shao J, Abd El Raouf M, **e H, Huang H, Wang H, et al. Near-infrared light-triggered drug delivery system based on black phosphorus for in vivo bone regeneration. Biomaterials. 2018;179:164–74.
Article
CAS
Google Scholar
**g X, **ong Z, Lin Z, Sun T. The Application of Black Phosphorus Nanomaterials in Bone Tissue Engineering. Pharmaceutics. 2022;14:2634.
Zhang F, **a Y, Liu Y, Leng J. Nano/microstructures of shape memory polymers: from materials to applications. Nanoscale Horiz. 2020;5:1155–73.
Article
CAS
Google Scholar
Pfau MR, Beltran FO, Woodard LN, Dobson LK, Gasson SB, Robbins AB, et al. Evaluation of a self-fitting, shape memory polymer scaffold in a rabbit calvarial defect model. Acta Biomater. 2021;136:233–42.
Article
CAS
Google Scholar
Wang L, Qiu Y, Guo Y, Si Y, Liu L, Cao J, et al. Smart, Elastic, and Nanofiber-Based 3D Scaffolds with Self-Deploying Capability for Osteoporotic Bone Regeneration. Nano Lett. 2019;19:9112–20.
Article
CAS
Google Scholar
Huang K, Lin B, Liu Y, Ren H, Guo Q. Correlation Analysis between Chronic Osteomyelitis and Bacterial Biofilm. Stem Cells Int. 2022;2022:9433847.
Article
Google Scholar
Cui Y, Liu H, Tian Y, Fan Y, Li S, Wang G, et al. Dual-functional composite scaffolds for inhibiting infection and promoting bone regeneration. Mater Today Bio. 2022;16:100409.
Article
CAS
Google Scholar
Kremers HM, Nwojo ME, Ransom JE, Wood-Wentz CM, Melton LJ 3rd, Huddleston PM 3rd. Trends in the epidemiology of osteomyelitis: a population-based study, 1969 to 2009. J Bone Joint Surg Am. 2015;97:837–45.
Article
Google Scholar
Murray CK, Obremskey WT, Hsu JR, Andersen RC, Calhoun JH, Clasper JC, et al. Prevention of infections associated with combat-related extremity injuries. J Trauma. 2011;71:S235–57.
CAS
Google Scholar
Masters EA, Ricciardi BF, Bentley KLM, Moriarty TF, Schwarz EM, Muthukrishnan G. Skeletal infections: microbial pathogenesis, immunity and clinical management. Nat Rev Microbiol. 2022;20:385–400.
Article
CAS
Google Scholar
Dos Reis JA Jr, Dos Santos JN, Barreto BS, de Assis PN, Almeida PF, Pinheiro AL. Photodynamic Antimicrobial Chemotherapy (PACT) in osteomyelitis induced by Staphylococcus aureus: Microbiological and histological study. J Photochem Photobiol B. 2015;149:235–42.
Article
CAS
Google Scholar
Pierfelice TV, D'Amico E, D'Ercole S, Lepore S, Piattelli A, Barone A, et al. Functionalization of a Cortical Membrane with a Photodynamic Protocol. J Funct Biomater. 2023;14:133.
Yuan X, Zhu W, Yang Z, Chen F, Han X. Three-Dimensional Printing of Poly-L-Lactic Acid Composite Scaffolds with Enhanced Bioactivity and Controllable Zn Ion Release Capability by Coupling with Carbon-ZnO. Bioengineering (Basel). 2023;10:307.
Yuan B, Zhou X, Li Y, Zhao Y, Xue M, Guo Q, et al. Black-Phosphorus-Nanosheet-Reinforced Coating of Implants for Sequential Biofilm Ablation and Bone Fracture Healing Acceleration. ACS Appl Mater Interfaces. 2022;14:47036–51.
Article
CAS
Google Scholar
Wu Y, Liao Q, Wu L, Luo Y, Zhang W, Guan M, et al. ZnL(2)-BPs Integrated Bone Scaffold under Sequential Photothermal Mediation: A Win-Win Strategy Delivering Antibacterial Therapy and Fostering Osteogenesis Thereafter. ACS Nano. 2021;15:17854–69.
Article
CAS
Google Scholar
**g X, Xu C, Su W, Ding Q, Ye B, Su Y, et al. Photosensitive and Conductive Hydrogel Induced Innerved Bone Regeneration for Infected Bone Defect Repair. Adv Healthc Mater. 2023;12:e2201349.
Article
Google Scholar
Chai M, An M, Zhang X. Construction of a TiO(2)/MoSe(2)/CHI coating on dental implants for combating Streptococcus mutans infection. Mater Sci Eng C Mater Biol Appl. 2021;129:112416.
Article
CAS
Google Scholar
Wang S, Duan C, Yang W, Gao X, Shi J, Kang J, et al. Two-dimensional nanocoating-enabled orthopedic implants for bimodal therapeutic applications. Nanoscale. 2020;12:11936–46.
Article
CAS
Google Scholar
Lu HT, Huang GY, Chang WJ, Lu TW, Huang TW, Ho MH, et al. Modification of chitosan nanofibers with CuS and fucoidan for antibacterial and bone tissue engineering applications. Carbohydr Polym. 2022;281:119035.
Article
CAS
Google Scholar
Yang Y, Zan J, Shuai Y, Yang L, Zhang L, Zhang H, et al. In Situ Growth of a Metal-Organic Framework on Graphene Oxide for the Chemo-Photothermal Therapy of Bacterial Infection in Bone Repair. ACS Appl Mater Interfaces. 2022;14:21996–2005.
Article
CAS
Google Scholar
Zhang Z, Wang Y, Teng W, Zhou X, Ye Y, Zhou H, et al. An orthobiologics-free strategy for synergistic photocatalytic antibacterial and osseointegration. Biomaterials. 2021;274:120853.
Article
CAS
Google Scholar
Huo J, Jia Q, Wang K, Chen J, Zhang J, Li P, et al. Metal-Phenolic Networks Assembled on TiO(2) Nanospikes for Antimicrobial Peptide Deposition and Osteoconductivity Enhancement in Orthopedic Applications. Langmuir. 2023;39:1238–49.
Google Scholar
Zhang G, Yang Y, Shi J, Yao X, Chen W, Wei X, et al. Near-infrared light II - assisted rapid biofilm elimination platform for bone implants at mild temperature. Biomaterials. 2021;269:120634.
Article
CAS
Google Scholar
Li Y, Xu X, Liu X, Li B, Han Y, Zheng Y, et al. Photoelectrons Mediating Angiogenesis and Immunotherapy through Heterojunction Film for Noninvasive Disinfection. Adv Sci (Weinh). 2020;7:2000023.
CAS
Google Scholar
Hall CW, Mah TF. Molecular mechanisms of biofilm-based antibiotic resistance and tolerance in pathogenic bacteria. FEMS Microbiol Rev. 2017;41:276–301.
Article
CAS
Google Scholar
Dieltjens L, Appermans K, Lissens M, Lories B, Kim W, Van der Eycken EV, et al. Inhibiting bacterial cooperation is an evolutionarily robust anti-biofilm strategy. Nat Commun. 2020;11:107.
Article
CAS
Google Scholar
Yuan Z, Tao B, He Y, Mu C, Liu G, Zhang J, et al. Remote eradication of biofilm on titanium implant via near-infrared light triggered photothermal/photodynamic therapy strategy. Biomaterials. 2019;223:119479.
Article
CAS
Google Scholar
Isakoff MS, Bielack SS, Meltzer P, Gorlick R. Osteosarcoma: Current Treatment and a Collaborative Pathway to Success. J Clin Oncol. 2015;33:3029–35.
Article
CAS
Google Scholar
Weilbaecher KN, Guise TA, McCauley LK. Cancer to bone: a fatal attraction. Nat Rev Cancer. 2011;11:411–25.
Article
CAS
Google Scholar
Zou B, **ong Z, He L, Chen T. Reversing breast cancer bone metastasis by metal organic framework-capped nanotherapeutics via suppressing osteoclastogenesis. Biomaterials. 2022;285:121549.
Article
CAS
Google Scholar
Long J, Zhang W, Chen Y, Teng B, Liu B, Li H, et al. Multifunctional magnesium incorporated scaffolds by 3D-Printing for comprehensive postsurgical management of osteosarcoma. Biomaterials. 2021;275:120950.
Article
CAS
Google Scholar
Deng X, Shao Z, Zhao Y. Solutions to the Drawbacks of Photothermal and Photodynamic Cancer Therapy. Adv Sci (Weinh). 2021;8:2002504.
CAS
Google Scholar
Sun P, Qu F, Zhang C, Cheng P, Li X, Shen Q, et al. NIR-II Excitation Phototheranostic Platform for Synergistic Photothermal Therapy/Chemotherapy/Chemodynamic Therapy of Breast Cancer Bone Metastases. Adv Sci (Weinh). 2022;9:e2204718.
Google Scholar
Xue Y, Niu W, Wang M, Chen M, Guo Y, Lei B. Engineering a Biodegradable Multifunctional Antibacterial Bioactive Nanosystem for Enhancing Tumor Photothermo-Chemotherapy and Bone Regeneration. ACS Nano. 2020;14:442–53.
Article
CAS
Google Scholar
Han X, Zhou L, Zhuang H, Wei P, Li F, Jiang L, et al. Hybrid Mesoporous MnO(2)-Upconversion Nanoparticles for Image-Guided Lung Cancer Spinal Metastasis Therapy. ACS Appl Mater Interfaces. 2022;14:18031–42.
Article
CAS
Google Scholar
Wan Z, Zhang P, Lv L, Zhou Y. NIR light-assisted phototherapies for bone-related diseases and bone tissue regeneration: A systematic review. Theranostics. 2020;10:11837–61.
Article
CAS
Google Scholar
Gao X, Li L, Cai X, Huang Q, **ao J, Cheng Y. Targeting nanoparticles for diagnosis and therapy of bone tumors: Opportunities and challenges. Biomaterials. 2021;265:120404.
Article
CAS
Google Scholar
Liu WB, Dong SH, Hu WH, Gao M, Li T, Ji QB, et al. A simple, universal and multifunctional template agent for personalized treatment of bone tumors. Bioact Mater. 2021;12:292–302.
CAS
Google Scholar
Sharma A, Nair R, Achreja A, Mittal A, Gupta P, Balakrishnan K, et al. Therapeutic implications of mitochondrial stress-induced proteasome inhibitor resistance in multiple myeloma. Sci Adv. 2022;8:eabq5575.
Article
CAS
Google Scholar
Huang Y, **ao Z, Guan Z, Shen Y, Jiang Y, Xu X, et al. A light-triggered self-reinforced nanoagent for targeted chemo-photodynamic therapy of breast cancer bone metastases via ER stress and mitochondria mediated apoptotic pathways. J Control Release. 2020;319:119–34.
Article
CAS
Google Scholar
Yang Z, Li Z, Zhao Y, Zhao Y, Li X, He L, et al. Lotus Seedpod-Inspired Crosslinking-Assembled Hydrogels Based on Gold Nanoclusters for Synergistic Osteosarcoma Multimode Imaging and Therapy. ACS Appl Mater Interfaces. 2022;14:34377–87.
Article
CAS
Google Scholar
Guo R, Wang S, Zhao L, Zong Q, Li T, Ling G, et al. Engineered nanomaterials for synergistic photo-immunotherapy. Biomaterials. 2022;282:121425.
Article
CAS
Google Scholar
Li Z, Lai X, Fu S, Ren L, Cai H, Zhang H, et al. Immunogenic Cell Death Activates the Tumor Immune Microenvironment to Boost the Immunotherapy Efficiency. Adv Sci (Weinh). 2022;9:e2201734.
Google Scholar
Gao S, Yang X, Xu J, Qiu N, Zhai G. Nanotechnology for Boosting Cancer Immunotherapy and Remodeling Tumor Microenvironment: The Horizons in Cancer Treatment. ACS Nano. 2021;15:12567–603.
Article
CAS
Google Scholar
Tian H, Cao J, Li B, Nice EC, Mao H, Zhang Y, et al. Managing the immune microenvironment of osteosarcoma: the outlook for osteosarcoma treatment. Bone Res. 2023;11:11.
Article
CAS
Google Scholar
Zhang X, Wan J, Mo F, Tang D, **ao H, Li Z, et al. Targeting Bone Tumor and Subcellular Endoplasmic Reticulum via Near Infrared II Fluorescent Polymer for Photodynamic-Immunotherapy to Break the Step-Reduction Delivery Dilemma. Adv Sci (Weinh). 2022;9:e2201819.
Google Scholar
Huang Y, Guan Z, Dai X, Shen Y, Wei Q, Ren L, et al. Engineered macrophages as near-infrared light activated drug vectors for chemo-photodynamic therapy of primary and bone metastatic breast cancer. Nat Commun. 2021;12:4310.
Article
CAS
Google Scholar
Zhou L, Liang H, Ge Y, Ding W, Chen Q, Zhang T, et al. Precisely Targeted Nano-Controller of PD-L1 Level for Non-Small Cell Lung Cancer Spinal Metastasis Immunotherapy. Adv Healthc Mater. 2022;11:e2200938.
Article
Google Scholar
Sullivan RJ, Flaherty KT. Immunotherapy: Anti-PD-1 therapies-a new first-line option in advanced melanoma. Nat Rev Clin Oncol. 2015;12:625–6.
Article
Google Scholar
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373:1627–39.
Article
CAS
Google Scholar
Wang L, Long NJ, Li L, Lu Y, Li M, Cao J, et al. Multi-functional bismuth-doped bioglasses: combining bioactivity and photothermal response for bone tumor treatment and tissue repair. Light Sci App. 2018;7:1.
Article
Google Scholar
Yang B, Yin J, Chen Y, Pan S, Yao H, Gao Y, et al. 2D-Black-Phosphorus-Reinforced 3D-Printed Scaffolds:A Stepwise Countermeasure for Osteosarcoma. Adv Mater. 2018;30:1705611.
He C, Dong C, Yu L, Chen Y, Hao Y. Ultrathin 2D Inorganic Ancient Pigment Decorated 3D-Printing Scaffold Enables Photonic Hyperthermia of Osteosarcoma in NIR-II Biowindow and Concurrently Augments Bone Regeneration. Adv Sci (Weinh). 2021;8:e2101739.
Google Scholar
Yang C, Ma H, Wang Z, Younis MR, Liu C, Wu C, et al. 3D Printed Wesselsite Nanosheets Functionalized Scaffold Facilitates NIR-II Photothermal Therapy and Vascularized Bone Regeneration. Adv Sci (Weinh). 2021;8:e2100894.
Google Scholar
Lin H, Shi S, Lan X, Quan X, Xu Q, Yao G, et al. Scaffold 3D-Printed from Metallic Nanoparticles-Containing Ink Simultaneously Eradicates Tumor and Repairs Tumor-Associated Bone Defects. Small Methods. 2021;5:e2100536.
Article
Google Scholar
Xu C, **a Y, Zhuang P, Liu W, Mu C, Liu Z, et al. FePSe(3) -Nanosheets-Integrated Cryogenic-3D-Printed Multifunctional Calcium Phosphate Scaffolds for Synergistic Therapy of Osteosarcoma. Small. 2023;19:e2303636.
Zeng Y, Pan Z, Yuan J, Song Y, Feng Z, Chen Z, et al. Inhibiting Osteolytic Breast Cancer Bone Metastasis by Bone-Targeted Nanoagent via Remodeling the Bone Tumor Microenvironment Combined with NIR-II Photothermal Therapy. Small. 2023:e2301003.
Shupp AB, Kolb AD, Mukhopadhyay D, Bussard KM. Cancer Metastases to Bone: Concepts, Mechanisms, and Interactions with Bone Osteoblasts. Cancers (Basel). 2018;10:182.
Yang H, Yu Z, Ji S, Huo Q, Yan J, Gao Y, et al. Targeting bone microenvironments for treatment and early detection of cancer bone metastatic niches. J Control Release. 2022;341:443–56.
Article
CAS
Google Scholar
Sun W, Ge K, ** Y, Han Y, Zhang H, Zhou G, et al. Bone-Targeted Nanoplatform Combining Zoledronate and Photothermal Therapy To Treat Breast Cancer Bone Metastasis. ACS Nano. 2019;13:7556–67.
Article
CAS
Google Scholar
Reichenbach S, Felson DT, Hincapié CA, Heldner S, Bütikofer L, Lenz A, et al. Effect of Biomechanical Footwear on Knee Pain in People With Knee Osteoarthritis: The BIOTOK Randomized Clinical Trial. Jama. 2020;323:1802–12.
Article
Google Scholar
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393:1745–59.
Article
CAS
Google Scholar
Bateman JF, Rowley L, Belluoccio D, Chan B, Bell K, Fosang AJ, et al. Transcriptomics of wild-type mice and mice lacking ADAMTS-5 activity identifies genes involved in osteoarthritis initiation and cartilage destruction. Arthritis Rheum. 2013;65:1547–60.
Article
CAS
Google Scholar
Yao Q, Wu X, Tao C, Gong W, Chen M, Qu M, et al. Osteoarthritis: pathogenic signaling pathways and therapeutic targets. Signal Transduct Target Ther. 2023;8:56.
Article
Google Scholar
Xu S, Chang L, Zhao X, Hu Y, Lin Y, Chen Z, et al. Preparation of epigallocatechin gallate decorated Au-Ag nano-heterostructures as NIR-sensitive nano-enzymes for the treatment of osteoarthritis through mitochondrial repair and cartilage protection. Acta Biomater. 2022;144:168–82.
Article
CAS
Google Scholar
Jiang S, Guo W, Tian G, Luo X, Peng L, Liu S, et al. Clinical Application Status of Articular Cartilage Regeneration Techniques: Tissue-Engineered Cartilage Brings New Hope. Stem Cells Int. 2020;2020:5690252.
Article
Google Scholar
Liu Y, Dzidotor G, Le TT, Vinikoor T, Morgan K, Curry EJ, et al. Exercise-induced piezoelectric stimulation for cartilage regeneration in rabbits. Sci Transl Med. 2022;14:eabi7282.
Article
CAS
Google Scholar
Sart S, Song L, Li Y. Controlling Redox Status for Stem Cell Survival, Expansion, and Differentiation. Oxidative Med Cell Longev. 2015;2015:105135.
Article
Google Scholar
Kim KS, Choi HW, Yoon HE, Kim IY. Reactive oxygen species generated by NADPH oxidase 2 and 4 are required for chondrogenic differentiation. J Biol Chem. 2010;285:40294–302.
Article
CAS
Google Scholar
Lu Z, Liu S, Le Y, Qin Z, He M, Xu F, et al. An injectable collagen-genipin-carbon dot hydrogel combined with photodynamic therapy to enhance chondrogenesis. Biomaterials. 2019;218:119190.
Article
CAS
Google Scholar
Zheng L, Liu S, Cheng X, Qin Z, Lu Z, Zhang K, et al. Intensified Stiffness and Photodynamic Provocation in a Collagen-Based Composite Hydrogel Drive Chondrogenesis. Adv Sci (Weinh). 2019;6:1900099.
Google Scholar
Tong L, Yu H, Huang X, Shen J, **ao G, Chen L, et al. Current understanding of osteoarthritis pathogenesis and relevant new approaches. Bone Res. 2022;10:60.
Article
CAS
Google Scholar
Au MT, Shi J, Fan Y, Ni J, Wen C, Yang M. Nerve Growth Factor-Targeted Molecular Theranostics Based on Molybdenum Disulfide Nanosheet-Coated Gold Nanorods (MoS(2)-AuNR) for Osteoarthritis Pain. ACS Nano. 2021;15:11711–23.
Article
CAS
Google Scholar
Zhao Y, Wei C, Chen X, Liu J, Yu Q, Liu Y, et al. Drug Delivery System Based on Near-Infrared Light-Responsive Molybdenum Disulfide Nanosheets Controls the High-Efficiency Release of Dexamethasone To Inhibit Inflammation and Treat Osteoarthritis. ACS Appl Mater Interfaces. 2019;11:11587–601.
Article
CAS
Google Scholar
Chen X, Liu Y, Wen Y, Yu Q, Liu J, Zhao Y, et al. A photothermal-triggered nitric oxide nanogenerator combined with siRNA for precise therapy of osteoarthritis by suppressing macrophage inflammation. Nanoscale. 2019;11:6693–709.
Article
CAS
Google Scholar
Chen Z, Zhang F, Zhang H, Cheng L, Chen K, Shen J, et al. DNA-Grafted Hyaluronic Acid System with Enhanced Injectability and Biostability for Photo-Controlled Osteoarthritis Gene Therapy. Adv Sci (Weinh). 2021;8:2004793.
CAS
Google Scholar
Fu K, Robbins SR, McDougall JJ. Osteoarthritis: the genesis of pain. Rheumatology (Oxford). 2018;57:iv43–50.
Article
CAS
Google Scholar
Yu H, Huang T, Lu WW, Tong L, Chen D. Osteoarthritis Pain. Int J Mol Sci. 2022;23:4642.
Huang J, Zhao L, Fan Y, Liao L, Ma PX, **ao G, et al. The microRNAs miR-204 and miR-211 maintain joint homeostasis and protect against osteoarthritis progression. Nat Commun. 2019;10:2876.
Article
Google Scholar
Vargas ESNCO, Dos Anjos RL, Santana MMC, Battistella LR, Marcon AF. Discordance between radiographic findings, pain, and superficial temperature in knee osteoarthritis. Reumatologia. 2020;58:375–80.
Article
Google Scholar
Zhao L, Huang J, Fan Y, Li J, You T, He S, et al. Exploration of CRISPR/Cas9-based gene editing as therapy for osteoarthritis. Ann Rheum Dis. 2019;78:676–82.
Article
CAS
Google Scholar
Kwon HK, Lee I, Yu KE, Cahill SV, Alder KD, Lee S, et al. Dual therapeutic targeting of intra-articular inflammation and intracellular bacteria enhances chondroprotection in septic arthritis. Sci Adv. 2021;7:eabf2665.
Gravallese EM, Firestein GS. Rheumatoid Arthritis - Common Origins, Divergent Mechanisms. N Engl J Med. 2023;388:529–42.
Article
CAS
Google Scholar
Aletaha D, Smolen JS. Diagnosis and Management of Rheumatoid Arthritis: A Review. Jama. 2018;320:1360–72.
Article
Google Scholar
Roodenrijs NMT, Welsing PMJ, van der Goes MC, Tekstra J, Lafeber F, Jacobs JWG, et al. Healthcare utilization and economic burden of difficult-to-treat rheumatoid arthritis: a cost-of-illness study. Rheumatology (Oxford). 2021;60:4681–90.
Article
Google Scholar
Roodenrijs NMT, van der Goes MC, Welsing PMJ, Tekstra J, Lafeber F, Jacobs JWG, et al. Difficult-to-treat rheumatoid arthritis: contributing factors and burden of disease. Rheumatology (Oxford). 2021;60:3778–88.
Article
Google Scholar
Scherer HU, Häupl T, Burmester GR. The etiology of rheumatoid arthritis. J Autoimmun. 2020;110:102400.
Article
CAS
Google Scholar
Weyand CM, Goronzy JJ. The immunology of rheumatoid arthritis. Nat Immunol. 2021;22:10–8.
Article
CAS
Google Scholar
Hendrich C, Hüttmann G, Lehnert C, Diddens H, Siebert WE. Photodynamic laser therapy for rheumatoid arthritis. Cell culture studies and animal experiments. Knee Surg Sports Traumatol Arthrosc. 1997;5:58–63.
Article
CAS
Google Scholar
Gallardo-Villagrán M, Paulus L, Charissoux JL, Sutour S, Vergne-Salle P, Leger DY, et al. Evaluation of Ruthenium-Based Assemblies as Carriers of Photosensitizers to Treat Rheumatoid Arthritis by Photodynamic Therapy. Pharmaceutics. 2021;13:2104.
Gallardo-Villagrán M, Paulus L, Charissoux JL, Leger DY, Vergne-Salle P, Therrien B, et al. Ruthenium-based assemblies incorporating tetrapyridylporphyrin panels: a photosensitizer delivery strategy for the treatment of rheumatoid arthritis by photodynamic therapy. Dalton Trans. 2022;51:9673–80.
Article
Google Scholar
Hu S, Lin Y, Tong C, Huang H, Yi O, Dai Z, et al. A pH-Driven indomethacin-loaded nanomedicine for effective rheumatoid arthritis therapy by combining with photothermal therapy. J Drug Target. 2022;30:737–52.
Article
CAS
Google Scholar
Gabriel D, Busso N, So A, van den Bergh H, Gurny R, Lange N. Thrombin-sensitive photodynamic agents: a novel strategy for selective synovectomy in rheumatoid arthritis. J Control Release. 2009;138:225–34.
Article
CAS
Google Scholar
Lan M, Zhao S, Liu W, Lee CS, Zhang W, Wang P. Photosensitizers for Photodynamic Therapy. Adv Healthc Mater. 2019;8:e1900132.
Article
Google Scholar
Kim MA, Shin SR, Kim HJ, Lee JS, Lee CM. Chemo-photothermal therapeutic effect of chitosan-gelatin hydrogels containing methotrexate and melanin on a collagen-induced arthritis mouse model. Int J Biol Macromol. 2022;218:1013–20.
Article
CAS
Google Scholar
Lu Y, Li L, Lin Z, Wang L, Lin L, Li M, et al. A New Treatment Modality for Rheumatoid Arthritis: Combined Photothermal and Photodynamic Therapy Using Cu(7.2) S(4) Nanoparticles. Adv Healthc Mater. 2018;7:e1800013.
Article
Google Scholar
Ren H, He Y, Liang J, Cheng Z, Zhang M, Zhu Y, et al. Role of Liposome Size, Surface Charge, and PEGylation on Rheumatoid Arthritis Targeting Therapy. ACS Appl Mater Interfaces. 2019;11:20304–15.
Article
CAS
Google Scholar
Dorst DN, Boss M, Rijpkema M, Walgreen B, Helsen MMA, Bos DL, et al. Photodynamic Therapy Targeting Macrophages Using IRDye700DX-Liposomes Decreases Experimental Arthritis Development. Pharmaceutics. 2021;13:1868.
Zhang S, Wu L, Cao J, Wang K, Ge Y, Ma W, et al. Effect of magnetic nanoparticles size on rheumatoid arthritis targeting and photothermal therapy. Colloids Surf B Biointerfaces. 2018;170:224–32.
Article
CAS
Google Scholar
Yu H, Fan J, Shehla N, Qiu Y, Lin Y, Wang Z, et al. Biomimetic Hybrid Membrane-Coated Xuetongsu Assisted with Laser Irradiation for Efficient Rheumatoid Arthritis Therapy. ACS Nano. 2022;16:502–21.
Article
CAS
Google Scholar
Zheng C, Wu A, Zhai X, Ji H, Chen Z, Chen X, et al. The cellular immunotherapy of integrated photothermal anti-oxidation Pd-Se nanoparticles in inhibition of the macrophage inflammatory response in rheumatoid arthritis. Acta Pharm Sin B. 2021;11:1993–2003.
Article
CAS
Google Scholar
Dorst DN, Rijpkema M, Buitinga M, Walgreen B, Helsen MMA, Brennan E, et al. Targeting of fibroblast activation protein in rheumatoid arthritis patients: imaging and ex vivo photodynamic therapy. Rheumatology (Oxford). 2022;61:2999–3009.
Article
CAS
Google Scholar
Qiu S, Wu X, Li Z, Xu X, Wang J, Du Y, et al. A Smart Nanoreactor Based on an O(2)-Economized Dual Energy Inhibition Strategy Armed with Dual Multi-stimuli-Responsive "Doorkeepers" for Enhanced CDT/PTT of Rheumatoid Arthritis. ACS Nano. 2022;16:17062–79.
Article
CAS
Google Scholar
Li X, Hou Y, Meng X, Li G, Xu F, Teng L, et al. Folate receptor-targeting mesoporous silica-coated gold nanorod nanoparticles for the synergistic photothermal therapy and chemotherapy of rheumatoid arthritis. RSC Adv. 2021;11:3567–74.
Article
Google Scholar
Pandey PK, Maheshwari R, Raval N, Gondaliya P, Kalia K, Tekade RK. Nanogold-core multifunctional dendrimer for pulsatile chemo-, photothermal- and photodynamic- therapy of rheumatoid arthritis. J Colloid Interface Sci. 2019;544:61–77.
Article
CAS
Google Scholar
Chen X, Zhu X, Ma L, Lin A, Gong Y, Yuan G, et al. A core-shell structure QRu-PLGA-RES-DS NP nanocomposite with photothermal response-induced M2 macrophage polarization for rheumatoid arthritis therapy. Nanoscale. 2019;11:18209–23.
Article
CAS
Google Scholar
Chen X, Zhu X, Xu T, Xu M, Wen Y, Liu Y, et al. Targeted hexagonal Pd nanosheet combination therapy for rheumatoid arthritis via the photothermal controlled release of MTX. J Mater Chem B. 2019;7:112–22.
Article
CAS
Google Scholar
Tsaltskan V, Firestein GS. Targeting fibroblast-like synoviocytes in rheumatoid arthritis. Curr Opin Pharmacol. 2022;67:102304.
Article
CAS
Google Scholar
Nygaard G, Firestein GS. Restoring synovial homeostasis in rheumatoid arthritis by targeting fibroblast-like synoviocytes. Nat Rev Rheumatol. 2020;16:316–33.
Article
Google Scholar
Huang R, Zhang C, Bu Y, Li Z, Zheng X, Qiu S, et al. A multifunctional nano-therapeutic platform based on octahedral yolk-shell Au NR@CuS: Photothermal/photodynamic and targeted drug delivery tri-combined therapy for rheumatoid arthritis. Biomaterials. 2021;277:121088.
Article
CAS
Google Scholar
Ha YJ, Lee SM, Mun CH, Kim HJ, Bae Y, Lim JH, et al. Methotrexate-loaded multifunctional nanoparticles with near-infrared irradiation for the treatment of rheumatoid arthritis. Arthritis Res Ther. 2020;22:146.
Article
CAS
Google Scholar
da Fonseca LJS, Nunes-Souza V, Goulart MOF, Rabelo LA. Oxidative Stress in Rheumatoid Arthritis: What the Future Might Hold regarding Novel Biomarkers and Add-On Therapies. Oxidative Med Cell Longev. 2019;2019:7536805.
Article
Google Scholar
Umar S, Palasiewicz K, Volin MV, Romay B, Rahat R, Tetali C, et al. Metabolic regulation of RA macrophages is distinct from RA fibroblasts and blockade of glycolysis alleviates inflammatory phenotype in both cell types. Cell Mol Life Sci. 2021;78:7693–707.
Article
CAS
Google Scholar
Rana AK, Li Y, Dang Q, Yang F. Monocytes in rheumatoid arthritis: Circulating precursors of macrophages and osteoclasts and, their heterogeneity and plasticity role in RA pathogenesis. Int Immunopharmacol. 2018;65:348–59.
Article
CAS
Google Scholar
Li X, Zhang S, Zhang M, Li G, Yang B, Lu X, et al. A Multifunctional Nano-Delivery System Against Rheumatoid Arthritis by Combined Phototherapy, Hypoxia-Activated Chemotherapy, and RNA Interference. Int J Nanomed. 2022;17:6257–73.
Article
Google Scholar
Li X, Zhang S, Zhang X, Hou Y, Meng X, Li G, et al. Folate receptor-targeting semiconducting polymer dots hybrid mesoporous silica nanoparticles against rheumatoid arthritis through synergistic photothermal therapy, photodynamic therapy, and chemotherapy. Int J Pharm. 2021;607:120947.
Article
CAS
Google Scholar
Fearon U, Canavan M, Biniecka M, Veale DJ. Hypoxia, mitochondrial dysfunction and synovial invasiveness in rheumatoid arthritis. Nat Rev Rheumatol. 2016;12:385–97.
Article
CAS
Google Scholar
Wang S, Chen R, Yu Q, Huang W, Lai P, Tang J, et al. Near-Infrared Plasmon-Boosted Heat/Oxygen Enrichment for Reversing Rheumatoid Arthritis with Metal/Semiconductor Composites. ACS Appl Mater Interfaces. 2020;12:45796–806.
Article
CAS
Google Scholar
Tang Q, Cui J, Tian Z, Sun J, Wang Z, Chang S, et al. Oxygen and indocyanine green loaded phase-transition nanoparticle-mediated photo-sonodynamic cytotoxic effects on rheumatoid arthritis fibroblast-like synoviocytes. Int J Nanomed. 2017;12:381–93.
Article
CAS
Google Scholar
Chen MW, Lu QJ, Chen YJ, Hou YK, Zou YM, Zhou Q, et al. NIR-PTT/ROS-Scavenging/Oxygen-Enriched Synergetic Therapy for Rheumatoid Arthritis by a pH-Responsive Hybrid CeO(2)-ZIF-8 Coated with Polydopamine. ACS Biomater Sci Eng. 2022;8:3361–76.
Article
CAS
Google Scholar
Peng X, Xu Z, Dentinger A, Kewalramani S, Jo J, Xu G, et al. Longitudinal volumetric assessment of inflammatory arthritis via photoacoustic imaging and Doppler ultrasound imaging. Photoacoustics. 2023;31:100514.
Article
Google Scholar
Wang Z, Tong Z, Chen H, Nie G, Hu J, Liu W, et al. Photoacoustic/ultrasonic dual-mode imaging for monitoring angiogenesis and synovial erosion in rheumatoid arthritis. Photoacoustics. 2023;29:100458.
Article
Google Scholar
Jo J, Xu G, Cao M, Marquardt A, Francis S, Gandikota G, et al. A Functional Study of Human Inflammatory Arthritis Using Photoacoustic Imaging. Sci Rep. 2017;7:15026.
Article
Google Scholar
Yang M, Zhao C, Wang M, Wang Q, Zhang R, Bai W, et al. Synovial Oxygenation at Photoacoustic Imaging to Assess Rheumatoid Arthritis Disease Activity. Radiology. 2023;306:220–8.
Article
Google Scholar
Chen J, Zeng S, Xue Q, Hong Y, Liu L, Song L, et al. Photoacoustic image-guided biomimetic nanoparticles targeting rheumatoid arthritis. Proc Natl Acad Sci USA. 2022;119:e2213373119.
Article
CAS
Google Scholar
Yan T, Su M, Wang Z, Zhang J. Second Near-Infrared Plasmonic Nanomaterials for Photoacoustic Imaging and Photothermal Therapy. Small. 2023;19:e2300539.
Chen J, Qi J, Chen C, Chen J, Liu L, Gao R, et al. Tocilizumab-Conjugated Polymer Nanoparticles for NIR-II Photoacoustic-Imaging-Guided Therapy of Rheumatoid Arthritis. Adv Mater. 2020;32:e2003399.
Article
Google Scholar
Wang R, Shi J, Zhang Q, Peng Q, Sun X, Song L, et al. Dual-Triggered Near-Infrared Persistent Luminescence Nanoprobe for Autofluorescence-Free Imaging-Guided Precise Therapy of Rheumatoid Arthritis. Adv Sci (Weinh). 2023;10:e2205320.
Google Scholar
Liu N, Chen X, Sun X, Sun X, Shi J. Persistent luminescence nanoparticles for cancer theranostics application. J Nanobiotechnol. 2021;19:113.
Article
CAS
Google Scholar
Pan W, Li Z, Qiu S, Dai C, Wu S, Zheng X, et al. Octahedral Pt-MOF with Au deposition for plasmonic effect and Schottky junction enhanced hydrogenothermal therapy of rheumatoid arthritis. Materials Today Bio. 2022;13:100214.
Article
CAS
Google Scholar
Yamakawa H, Kusumoto D, Hashimoto H, Yuasa S. Stem Cell Aging in Skeletal Muscle Regeneration and Disease. Int J Mol Sci. 2020;21:1830.
Morgan J, Partridge T. Skeletal muscle in health and disease. Dis Model Mech. 2020;13:dmm042192.
Cezar CA, Mooney DJ. Biomaterial-based delivery for skeletal muscle repair. Adv Drug Deliv Rev. 2015;84:188–97.
Article
CAS
Google Scholar
Shibaguchi T, Sugiura T, Fujitsu T, Nomura T, Yoshihara T, Naito H, et al. Effects of icing or heat stress on the induction of fibrosis and/or regeneration of injured rat soleus muscle. J Physiol Sci. 2016;66:345–57.
Article
CAS
Google Scholar
Mayer JM, Mooney V, Matheson LN, Erasala GN, Verna JL, Udermann BE, et al. Continuous low-level heat wrap therapy for the prevention and early phase treatment of delayed-onset muscle soreness of the low back: a randomized controlled trial. Arch Phys Med Rehabil. 2006;87:1310–7.
Article
Google Scholar
Zhang C, Jia S, Huang J, Peng H, Zhang J, Liu L, et al. A carbonized wormwood modified photothermal microneedle patch for the repair of damaged skeletal muscles. J Mater Chem B. 2021;9:8014–20.
Article
CAS
Google Scholar
McGorm H, Roberts LA, Coombes JS, Peake JM. Turning Up the Heat: An Evaluation of the Evidence for Heating to Promote Exercise Recovery, Muscle Rehabilitation and Adaptation. Sports Med. 2018;48:1311–28.