Abstract
Background
Symptomatic congenital biliary dilatation (CBD) during early infancy is always characterized by cystic dilation of the common bile duct with a narrow segment connecting the pancreatic duct.
Case presentation
In two consecutive infants with a prenatal diagnosis of CBD, we found that biliary sludge had formed in the cyst upon the appearance of symptoms including acholic stool and hypertransaminasemia. Infrared absorption spectrometry revealed that the sludge consisted of calcium bilirubinate.
Conclusion
We suggest that overproduction of bilirubin by neonatal hemolysis causes sedimentation of bilirubin calcium, resulting in obstruction of the narrow segment and development of symptoms.
Similar content being viewed by others
Background
Congenital biliary dilatation (CBD), also known as a choledochal cyst, is a malformation characterized by a dilated common bile duct and pancreaticobiliary maljunction [1]. Children with CBD develop characteristically intermittent symptoms such as abdominal pain, vomiting, jaundice, and elevated levels of serum transaminases and amylase. These symptoms are caused by protein plugs that form in the bile duct because of pancreatobiliary reflux and obstruct the common channel or the narrow segment distal to the dilated bile duct [2, 3]. However, some neonates and young infants with CBD present with obstructive cholangiopathy, which is similar to that seen in biliary atresia [4, 5]. In most such patients, CBD is diagnosed prenatally and is likely to cause liver fibrosis [4]. The symptomatology during early infancy is different from that in older children, but the precise mechanism is unknown. We herein report two cases that may help to illustrate the underlying mechanism.
Case presentation
Case 1
At 27 weeks’ gestation, ultrasonography revealed a cyst in the abdomen. A female neonate was born at 40 weeks’ gestation. A huge choledochal cyst was confirmed by ultrasound and magnetic resonance cholangiopancreatography. The neonate was asymptomatic until she developed acholic stool at 37 days of age. At 45 days, ultrasonography revealed debris in the cyst (Fig. 1b), and laboratory testing showed elevated serum transaminase levels (Fig. 2a). At 72 days, we performed choledochal cyst excision and confirmed a narrow segment distal to the huge cyst (Fig. 1d). The bile contained a large quantity of sludge. Infrared absorption spectrometry revealed that the sludge consisted of calcium bilirubinate (Fig. 1f). The amylase level in the bile was 5 U/L, and the lipase level was 66 U/L (24 and 8 U/L in the serum, respectively). The total bilirubin and direct bilirubin levels in the bile were respectively 6.07 mg/dl and 4.54 mg/dl.
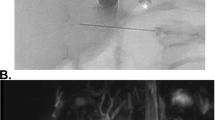
Data of Case 1. a Ultrasonography on day 2 showed a large choledochal cyst but no debris. b Ultrasonography on day 45 revealed debris in the cyst. c, d Magnetic resonance imaging and surgical findings confirmed a huge cyst and a narrow segment (arrow). e, f Infrared absorption spectra of the debris. Four major absorption bands (arrows) were characteristic of calcium bilirubinate
Laboratory data. a Preoperative laboratory data of Case 1. The transaminase and gamma-glutamyl transpeptidase (γGTP) concentration were elevated, but the direct bilirubin concentration was not significantly increased. b Preoperative laboratory data of Case 2. The hemoglobin level gradually decreased but the transaminase and γGTP concentrations did not increase during the neonatal period. However, the serum levels of transaminases and γGTP began to gradually increase at 4 months
Case 2
At 29 weeks’ gestation, ultrasonography revealed a cyst in the abdomen. A female neonate was born at 40 weeks’ gestation. A 3-cm-diameter choledochal cyst was confirmed by ultrasound. The neonate was asymptomatic, and her serum transaminase levels were not elevated (Fig. 2b). At 5 days of age, debris appeared in the dilated bile duct (Fig. 3a). At 4 months, her serum transaminase levels began to rise. The cyst gradually enlarged and the diameter was 33 mm at 5 days, 38 mm at 1 month, 44 mm at 3 months, and 50 mm at 6 months. At 6 months, acholic stool appeared and we performed laparoscopic choledochal cyst excision. The narrow segment was too thin to be identified. The bile was yellow and contained sludge (Fig. 3c), and infrared absorption spectrometry showed that the sludge consisted of calcium bilirubinate (Fig. 3d).
Data of Case 2. a Ultrasonography detected debris in the cyst. b Magnetic resonance imaging showed a cyst of the common bile duct. c The sludge in the bile duct consisted of fine black particles. d Infrared absorption spectra of the debris. Four major absorption bands (arrows) were characteristic of calcium bilirubinate
The amylase level in the bile was 1 U/L, and the lipase level was 282 U/L (37 and 31 U/L in the serum, respectively). The total bilirubin and direct bilirubin levels in the bile were respectively 14.50 mg/dl and 12.27 mg/dl.
Conclusions
Symptomatic CBD during early infancy is inevitably of the cystic-dilated type and is accompanied by a narrow segment distal to the cyst [4, 6]. The fusiform-dilated type of CBD does not cause symptoms during this period [6]. In early infancy, hemolysis accelerates because of physiological polycythemia of red blood cells with a short half-life of fetal hemoglobin. The fetal hemoglobin concentration typically decreases from 77% at 1 day to 52% at 6 to 9 weeks [7]. The association between hemolysis and pigment gallstones is well known [8]. Although biliary sludge had been recognized in neonates with CBD [9, 10], the present report is the first to reveal that the sludge was composed of calcium bilirubinate. Considering these facts, the following mechanism is probable. Neonatal hemolysis results in overproduction of bilirubin, causing a high concentration of bilirubin in bile. Stagnation of bilirubin-rich bile in the cystic-dilated bile duct results in sedimentation of calcium bilirubinate. This debris obstructs the narrow segment, causing obstructive cholangiopathy. The mechanism in neonates clearly differs from that in older infants and children, in whom protein plugs or rarely fatty acid calcium stones cause symptoms [1,2,3, 11].
The occurrence of obstruction depends on the amount of debris and caliber of the narrow segment. Our first patient had a relatively large caliber of the narrow segment but had a large amount of bile sludge, resulting in obstructive symptoms including elevated transaminase levels. However, incomplete obstruction did not cause complete obstructive jaundice (Fig. 2). The second patient had a smaller amount of debris, which caused no symptoms in the neonatal hemolytic period but resulted in gradually more severe obstructive cholangiopathy over a period of several months. This is the first report to suggest the mechanism of symptomatic CBD in neonates and young infants.
We perform operation for prenatally diagnosed CBD soon after the symptoms and signs of the biliary obstruction occur, which were the elevated levels of transaminase and gamma-glutamyl transpeptidase in Case 1 and acholic stool in Case 2. We wait operation unless obstructive symptoms, because congenital biliary stenoses around the hepatic hilum are more easily treated in older infants. Leaving the stenoses causes later hepatolithiasis [12].
Availability of data and materials
During the course of this research, no data were analyzed, reused, or generated.
Abbreviations
- CBD:
-
Congenital biliary dilatation
References
Kamisawa T, Kaneko K, Itoi T, Ando H. Pancreaticobiliary maljunction and congenital biliary dilatation. Lancet Gastroenterol Hepatol. 2017;2:610–8.
Kaneko K, Ando H, Ito T, Watanabe Y, Seo T, Harada T, et al. Protein plugs cause symptoms in patients with choledochal cysts. Am J Gastroenterol. 1997;92:1018–21.
Kaneko K, Ando H, Seo T, Ono Y, Tainaka T, Sumida W. Proteomic analysis of protein plugs: causative agent of symptoms in patients with choledochal cyst. Dig Dis Sci. 2007;52:1979–86.
Miyano T. The clinical and pathological study of the congenital dilatation of the common bile duct. Jpn J Pediatr Surg. 1973;9:605–20.
Todani T, Urushihara N, Morotomi Y, Watanabe Y, Uemura S, Noda T, et al. Characteristics of choledochal cysts in neonates and early infants. Eur Pediatr Surg. 1995;5:143–5.
Urushihara N, Fukumoto K, Yamoto M, Miyake H, Takahashi T, Nomura A, et al. Characteristics, management, and outcomes of congenital biliary dilation in neonates and early infants: a 20-year, single-institution study. J Hepatobiliary Pancreat Sci. 2018;25:544–9.
Bunn HF, Forget BG, Ranney HM. Human hemoglobins, vol. 107. Philadelphia: WB Saunders; 1977. p. 94.
Schwesinger WH, Kurtin WE. Changes in serum and bile bilirubin induced by acute hemolysis. J Surg Res. 1983;35:520–4.
Jesus MM, Jorge HRQ, Sonia CV, Luis CB. Giant choledochal cyst presenting during third trimester of pregnancy. BMJ Case Rep. 2018;5:78.
Zhou LY, Guan BY, Li L, Xu ZF, Dai CP, Wang W, et al. Objective differential characteristics of cystic biliary atresia and choledochal cysts in neonates and young infants. J Ultrasound Med. 2012;31:833–41.
Kaneko K, Ono Y, Tainaka T, Sumida W, Ando H. Fatty acid calcium stones in patients with pancreaticobiliary maljunction/choledochal cyst as another cause of obstructive symptoms besides protein plugs. J Pediatr Surg. 2008;43:564–7.
Ando H, Ito T, Kaneko K, Seo T, Ito F. Intrahepatic bile duct stenosis causing intrahepatic calculi formation following excision of a choledochal cyst. J Am Coll Surg. 1996;183:56–60.
Acknowledgements
We thank Angela Morben, DVM, ELS, from Edanz Group (https://en-author-services.edanz.com/ac), for editing a draft of this manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
SK and KK analyzed and interpreted the patient data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of Aichi Medical University approved this study, and the patients’ caregivers provided consent.
Consent for publication
The patients’ caregivers provided consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kato, S., Kaneko, K., Matsushita, N. et al. Calcium bilirubinate sludge causes early onset of congenital biliary dilatation: a report of two cases. surg case rep 7, 92 (2021). https://doi.org/10.1186/s40792-021-01175-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-021-01175-x