Abstract
A slope-correcting anterior closing wedge proximal tibial osteotomy is a powerful tool for correcting increased posterior tibial slope in the setting of a failed anterior cruciate ligament reconstruction. This case series documents three cases in which patients collapsed into varus following an anterior closing wedge proximal tibia osteotomy. Two patients had osteotomies fixated with a “suture-staple” construct, and all had medical comorbidities or reported noncompliance post-operatively. Therefore, meticulous care during the planning, execution, and rehabilitation phases is critical as multiple factors throughout the arc of care may contribute towards anterior closing wedge proximal tibial osteotomy varus collapse. Careful optimization of medical comorbidities and rigid fixation with either a plate and screws or compression staples should be used rather than a “suture-staple” to mitigate this risk.
Level of evidence: IV.
Similar content being viewed by others
Introduction
An anterior closing wedge proximal tibia osteotomy (PTO) is an important treatment option (Fig. 1A-D) for pathologic posterior tibial slope (PTS) in the setting of anterior cruciate ligament reconstruction (ACL-R) failure. While there are many potential contributing factors for ACL-R failure, increasingly recognized is the contribution of PTS [6, 23, 27]. Numerous studies have identified a normal PTS range between 7 and 10 degrees with PTS > 12 degrees being a risk factor for graft rupture and an indication for a slope correcting osteotomy [5, 7, 17, 25, 26]. Cadaveric studies have identified increased loads on the ACL in the setting of increased PTS as well as the decreased translational forces on the ACL following an anterior closing wedge PTO [3, 7, 9, 15, 16].
The literature on clinical outcomes of proximal tibia anterior slope-correcting osteotomies is limited to several small, retrospective studies. These suggest that an anterior slope-correcting PTO may be an effective tool to minimize the risk of subsequent ACL re-rupture in appropriately selected patients [1, 5, 19]. However, the occurrence of complications is not well-reported in the literature. In this series, 10 anterior closing wedge PTOs were performed between the two institutions during the study period. We report on three cases of varus malunion collapse occurring after an anterior closing wedge osteotomy for failed ACL-R in the setting of increased PTS.
Case reports
Case #1
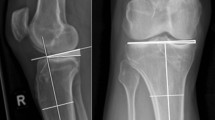
A 31-year-old female with a history of two prior ipsilateral ACL reconstructions presented 7 years after her previous ACL-R with about 5 years of recurrent left knee instability (Table 1). Exam and imaging were consistent with full knee range of motion (ROM), a torn ACL graft, tunnel osteolysis > 14 mm, and increased PTS (Fig. 2A-C). She had physiologic varus on mechanical axis views (Fig. 3).
She was indicated for a two-stage revision ACL-R (Table 1). There were no complications during her stage 1 procedure and the posterior cortical hinge of the osteotomy was maintained. Afterwards, patient was followed serially in clinic with interval radiographs showing correction of her posterior slope but with concern that the osteotomy was drifting into varus on mechanical axis views at 6 weeks. At 4 months, left knee films and standing mechanical alignment films were obtained which confirmed the varus malunion (Fig. 4).
The patient underwent her stage 2 procedure 5 months after stage 1. This corrected her varus (Fig. 5), but a CT scan at 4 months following this showed a delayed union (Fig. 6). However, with use of a bone stimulator and close surveillance, she healed her osteotomy (Fig. 7). At final follow up, she was doing well, and her exam demonstrated no residual anterior laxity.
Case #2
A 39-year-old male with a history of one ipsilateral ACL-R 11 years prior presented with 2 months of right knee pain, swelling, and instability that occurred while boxing (Table 1). Exam and imaging were consistent with full knee ROM, a torn ACL graft, a vertical femoral tunnel, tunnel osteolysis > 14 mm, and increased PTS (Fig. 8A-C).
He was indicated for a staged ACL-R. Stage 1 occurred without intra-operative complications and the posterior cortical hinge was maintained with no gap** at the osteotomy site throughout ROM following fixation.
A standing mechanical axis view and right knee radiographs at 6 weeks showed concern that the osteotomy had fallen into varus (Fig. 9). A 6-month CT scan showed the bone dowel allografts had incorporated. It also verified the varus collapse with areas of nonunion along the medial aspect of the osteotomy (Fig. 10). Ten months following stage 1, the patient underwent stage 2. The patient moved away a month after this and was lost to in-person follow up. However, by email he indicated he had returned to running and was doing well.
Case #3
A 51-year-old male with a history of two prior ipsilateral ACL reconstructions presented 5 years after his previous ACL-R with left knee pain and instability following a pivoting injury during a baseball game. Exam and imaging confirmed full knee ROM, ACL graft rupture, and increased PTS. A preoperative mechanical axis radiograph showed slight varus alignment (Fig. 11). During the osteotomy, the posterior cortical hinge was maintained, and there was no gap** throughout ROM following fixation. A millimeter more bone was removed laterally to provide some coronal correction.
At the 6-week post op appointment, the patient was noted to have collapsed into varus (Fig. 12). The patient noted that he had not been able to comply with the weight bearing restrictions given his job and social factors (Table 2). The osteotomy subsequently healed without further progression (Fig. 13). The patient was able to return to basketball with a stable knee but has had difficulty returning to full running. Revision osteotomy to correct varus was discussed but the patient has not wished to proceed.
Discussion
This case series demonstrates the importance of rigid fixation of anterior closing wedge PTOs with plate and screws or compression staples. This is especially critical in the setting of specific patient comorbidities that may elevate the risk of nonunion or malunion. A “suture-staple” construct does not provide enough stability to ensure routine healing and may risk varus collapse of the osteotomy.
Due to the infrequency with which anterior closing wedge PTOs are performed, the literature on their outcomes is limited to 4 retrospective series totaling 52 patients. A 2020 study by Akoto et al. consisting of 20 patients who underwent a 2-stage ACL revision consisting of an anterior closing wedge osteotomy in stage 1 and ACL-R with lateral extraarticular tenodesis (LET) in stage 2 noted an effective decrease in PTS, a stable ligamentous exam, and no cases of failure with an average of 30.5 months of follow up [1]. No intra-operative or post-operative complications were noted except for one patient with a post-operative hematoma which required return to the operative room on post-operative day 4. A similar series was published by Song et al. in which 18 patients with primary ACL ruptures and associated posterior horn of medial meniscus tears underwent an anterior closing wedge osteotomy for elevated PTS in the primary procedure [19]. At a minimum of 2 year follow up, all patients had stable ligamentous exams and there were no failures. No complications were noted.
A smaller series by Dejour et al. consisting of 9 patients with failed ACL-Rs also found good outcomes without failure at a mean 4-year follow up [5]. No intra-operative or post-operative complications were noted. Finally, Sonnery-Cottet et al. reported on 5 patients with combined anterior closing wedge osteotomies and revision ACL-R with a mean of 31.6 months follow up [20]. They reported no failures or complications, and all patients but one returned to pre-operative activity level. However, from the literature on concurrent high tibial osteotomy (HTO) and ACL-R, it is known there is up to a 30% complication rate and nonunion rates range from 0.7–4.4% [4, 11, 13, 21, 24].
Method of fixation varies greatly with this procedure (Table 3). If the posterior cortex is violated, a fracture plate and screw construct is necessary to ensure healing and alignment maintenance. An intact posterior hinge affords greater options. A plate with proximal locking screws provides good fixation and often greater surgeon confidence in advancing weight bearing restrictions more quickly. However, many patients find these constructs bulky and require the symptomatic hardware to be removed at a later time. Compression staple fixation offers a lower profile method that can also be used with more proximal supratubercle osteotomies with less proximal bone available for fixation. A high-strength tape-like suture and knotless anchors theoretically can be used to construct a suture-staple on either side of the tibial tubercle in much the same way a compression staple would be used. This also creates a tension band-like construct. It has been used for fixating osteotomies around the elbow and foot but has not previously been reported on for use with anterior closing wedge PTOs [2, 14, 18]. While this method avoids the issue of symptomatic hardware due to plates or staples, the authors do not recommend using this technique. Two of the 3 cases utilized this technique and failed despite being technically well-executed. Though a tension band construct with an intact posterior cortex has sufficient strength to prevent intra-operative gap**, the overall rigidity of the construct is likely insufficient to yield reliable healing especially when patients contain risk factors for nonunion.
Patient specific factors may also have contributed to the risk of varus collapse in this series. Smoking, obesity, and noncompliance with post-operative restrictions were present in cases 1, 2, and 3, respectively. Additionally, alcohol abuse, diabetes, vitamin D deficiency, and endocrine disorders all increase the risk of nonunion or malunion [8, 10, 12, 22, 28, 29]. As such, the presence of these risk factors should be screened for and any opportunity to address these and optimize their management prior to surgery should be undertaken.
In conclusion, meticulous care during the planning, execution, and rehabilitation phases is critical as multiple factors throughout the arc of care may contribute towards anterior closing wedge PTO varus collapse. Careful optimization of medical comorbidities and rigid fixation with either a plate and screws or compression staples should be used rather than a “suture-staple” to mitigate this risk.
Abbreviations
- ACL:
-
Anterior Cruciate Ligament
- ACL-R:
-
Anterior Cruciate Ligament Reconstruction
- PTS:
-
Posterior Tibial Slope
- PTO:
-
Proximal Tibia Osteotomy
- ROM:
-
Range of Motion
References
Akoto R, Alm L, Drenck TC, Frings J, Krause M, Frosch KH (2020) Slope-correction osteotomy with lateral extra-articular Tenodesis and revision anterior cruciate ligament reconstruction is highly effective in treating high-grade anterior knee laxity. Am J Sports Med 48:3478–3485
Bateman DK, Barlow JD, VanBeek C, Abboud JA (2015) Suture anchor fixation of displaced olecranon fractures in the elderly: a case series and surgical technique. J Shoulder Elb Surg 24:1090–1097
Bernhardson AS, Aman ZS, Dornan GJ, Kemler BR, Storaci HW, Brady AW et al (2019) Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior Tibial slope increases. Am J Sports Med 47:296–302
Crawford MD, Diehl LH, Amendola A (2017) Surgical management and treatment of the anterior cruciate ligament-deficient knee with malalignment. Clin Sports Med 36:119–133
Dejour D, Saffarini M, Demey G, Baverel L (2015) Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc 23:2846–2852
Di Benedetto P, Di Benedetto E, Fiocchi A, Beltrame A, Causero A (2016) Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res 28:319–324
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32:376–382
Gorter EA, Krijnen P, Schipper IB (2017) Vitamin D status and adult fracture healing. J Clin Orthop Trauma 8:34–37
Imhoff FB, Mehl J, Comer BJ, Obopilwe E, Cote MP, Feucht MJ et al (2019) Slope-reducing tibial osteotomy decreases ACL-graft forces and anterior tibial translation under axial load. Knee Surg Sports Traumatol Arthrosc 27:3381–3389
Lavery LA, Lavery DC, Green T, Hunt N, La Fontaine J, Kim PJ et al (2020) Increased risk of nonunion and Charcot Arthropathy after ankle fracture in people with diabetes. J Foot Ankle Surg 59:653–656
Li Y, Zhang H, Zhang J, Li X, Song G, Feng H (2015) Clinical outcome of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction for medial compartment osteoarthritis in young patients with anterior cruciate ligament-deficient knees: a systematic review. Arthroscopy 31:507–519
Liska F, Haller B, Voss A, Mehl J, Imhoff FB, Willinger L et al (2018) Smoking and obesity influence the risk of nonunion in lateral opening wedge, closing wedge and torsional distal femoral osteotomies. Knee Surg Sports Traumatol Arthrosc 26:2551–2557
Malahias MA, Shahpari O, Kaseta MK (2018) The clinical outcome of one-stage high Tibial osteotomy and anterior cruciate ligament reconstruction. A current concept systematic and comprehensive review. Arch Bone Jt Surg 6:161–168
McGee R, Howard S, LeCavalier D, Eudy A, Bascharon R, Hoang V (2021) Low-profile, suture anchor tension band construct for olecranon fractures and osteotomies. Arthrosc Tech 10:e325–e331
McLean SG, Lucey SM, Rohrer S, Brandon C (2010) Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clin Biomech (Bristol, Avon) 25:781–788
McLean SG, Oh YK, Palmer ML, Lucey SM, Lucarelli DG, Ashton-Miller JA et al (2011) The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am 93:1310–1317
Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA (2018) 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior Tibial slope. Am J Sports Med 46:531–543
Sinnett T, Fang Y, Nattfogel E, O'Gorman A, Charalambides C (2017) Suture fixation of an akin osteotomy: a cost effective and clinically reliable technique. Foot Ankle Surg 23:40–43
Song GY, Ni QK, Zheng T, Zhang ZJ, Feng H, Zhang H (2020) Slope-reducing Tibial osteotomy combined with primary anterior cruciate ligament reconstruction produces improved knee stability in patients with steep posterior Tibial slope, excessive anterior Tibial subluxation in extension, and chronic meniscal posterior horn tears. Am J Sports Med 48:3486–3494
Sonnery-Cottet B, Mogos S, Thaunat M, Archbold P, Fayard JM, Freychet B et al (2014) Proximal Tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med 42:1873–1880
Spahn G (2004) Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg 124:649–653
Tian R, Zheng F, Zhao W, Zhang Y, Yuan J, Zhang B et al (2020) Prevalence and influencing factors of nonunion in patients with tibial fracture: systematic review and meta-analysis. J Orthop Surg Res 15:377
Trojani C, Sbihi A, Djian P, Potel JF, Hulet C, Jouve F et al (2011) Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc 19:196–201
Turner RS, Griffiths H, Heatley FW (1993) The incidence of deep-vein thrombosis after upper tibial osteotomy. A venographic study. J Bone Joint Surg Br 75:942–944
Vyas S, van Eck CF, Vyas N, Fu FH, Otsuka NY (2011) Increased medial tibial slope in teenage pediatric population with open physes and anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 19:372–377
Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP (2013) Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med 41:2800–2804
Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR et al (2010) Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med 38:1979–1986
Zura R, Mehta S, Della Rocca GJ, Steen RG (2016) Biological risk factors for nonunion of bone fracture. JBJS Rev 4(1):e5
Zura R, **ong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ et al (2016) Epidemiology of fracture nonunion in 18 human bones. JAMA Surg 151:e162775
Disclosures
Mark D. Miler, MD
• Arthrex, Inc.: IP royalties; Paid consultant
• Saunders/Mosby-Elsevier: Publishing royalties, financial or material support
• Wolters Kluwer Health - Lippincott Williams & Wilkins: Publishing royalties, financial or material support
Author information
Authors and Affiliations
Contributions
All authors were involved with manuscript preparation including writing, editing, and approval of the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
MacLean, I.S., Tyndall, W.A., Schenck, R.C. et al. Varus collapse following anterior closing wedge proximal tibial osteotomy for ACL revision reconstruction: a case series. J EXP ORTOP 9, 100 (2022). https://doi.org/10.1186/s40634-022-00539-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-022-00539-y